Hysterosalpingography (HSG) is a gynecological test used to study the structures of the uterine cavity and the Fallopian tubes, as well as their permeability. It is, therefore, a test for the study of female fertility.
Usually, patients who turn to assisted reproduction have a hysterosalpingography to check if there is any uterine or tubal factor that prevents pregnancy. This test is not dangerous, but many women fear it because of the discomfort it causes.
Provided below is an index with the 9 points we are going to expand on in this article.
- 1.
- 2.
- 2.1.
- 3.
- 3.1.
- 4.
- 4.1.
- 4.2.
- 4.3.
- 5.
- 5.1.
- 6.
- 6.1.
- 6.2.
- 6.3.
- 6.4.
- 6.5.
- 6.6.
- 6.7.
- 6.8.
- 7.
- 8.
- 9.
Fertility tests
When a couple or woman with fertility problems visits a fertility clinic for the first time, a medical history will be carried out in which different aspects of their reproductive life are evaluated. For example, whether they have previous children, how long they have been trying to get pregnant, and so on.
Depending on the information collected, both men and women will then undergo a series of tests to analyze the state of their fertility. One of the tests that is frequently ordered to check female fertility is hysterosalpingography.
In general, this diagnostic test is very feared by women because of the discomfort it causes and subsequent recovery. However, it can provide doctors with a lot of information about the causes of infertility and the possible treatment needed to achieve pregnancy.
Other medical tests that are requested along with the HSG are the ultrasound and the hormone profile, which provide information about the ovarian reserve and the woman's ovulatory capacity.
Definition of Hysterosalpingography
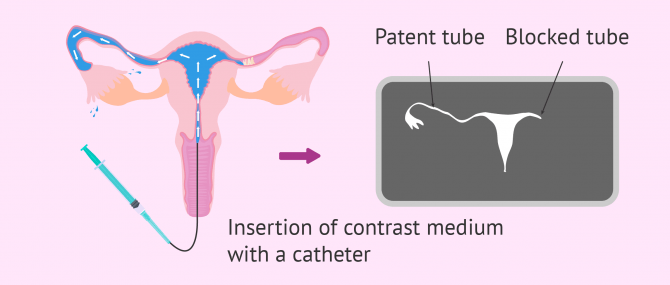
Hysterosalpingography is one of the main diagnostic tests to find out the possible causes of female sterility. This test involves taking an x-ray of the woman's uterus and fallopian tubes. To do this, the specialist uses a type of iodized contrast that is introduced through the cervix with the help of a cannula.
As the contrast fluid flows into the uterine cavity and tubes, the radiologist will take the necessary images using a special x-ray technique that allows internal organs to be seen in motion: fluoroscopy.
Unlike ultrasound, hysterosalpingography is not routinely performed in gynecology practices until there is a specific indication for it.
Types of HSG
Today, there is an improved version of hysterosalpingography that allows this test to be performed in less time and with less discomfort for the patient.
This new variant is known as hysterosalpingosonography (HSSG) and, as the name suggests, uses ultrasound to obtain the images instead of X-rays, which is already a great advantage.
Furthermore, depending on the contrast medium used, the following types of HSSG are differentiated:
- HyCoSy: is short for Hysterosalpingo-Contrast-Sonography, a type of HSSG that uses saline or a galactose solution as contrast. This contrast is injected through the cervix and, through a transvaginal ultrasound, is followed through the uterus and fallopian tubes.
- HyFoSy: is short for Hysterosalpingo-Foam-Sonography, an even newer type of HSSG that does not use contrast agents. Instead, a foaming gel is injected vaginally that fills the uterine cavity and diffuses into the fallopian tubes, providing much clearer and sharper images via ultrasound.
Indications of the HSG
For fertilization and natural pregnancy to take place, the sperm ejaculated during intercourse need to reach the egg released by the woman's ovary in the Fallopian tube. The fertilized embryo from this union then travels through the Fallopian tube to the uterus, where it implants in the endometrium and begins gestation.
If there is a tubal obstruction that prevents contact between the egg and sperm in both Fallopian tubes, then obviously pregnancy cannot occur naturally until this obstruction is cleared.
Hysterosalpingography allows both the anatomical integrity of the female reproductive system and the functionality of the Fallopian tubes to be assessed, as it provides information on tubal patency.
In short, hysterosalpingography is a great help in determining the cause of infertility and deciding which assisted reproduction technique has the greatest chance of success, either artificial insemination (AI) or in vitro fertilization (IVF).
Hysterosalpingography is also indicated for the study of women with menstrual disorders, pelvic pain, pelvic tumors, and congenital malformations. It can also be done to test the success of tubal ligation.
In assisted reproduction, like any medical treatment, it is necessary for you to trust the professionalism of the doctors and the clinic you choose.
This Tool generates you a personalized report with all information necessary about the treatment you will need. Besides, there is a list of clinics in your area which we have chosen based on our selection criteria with their budget plan included. Last but not least, you will find a series of useful tips for your first clinic visit.
What alterations does HSG detect?
Once the hysterosalpingography is done, it is possible to check for abnormalities at the level of the cervix, the uterine cavity or the Fallopian tubes. Here are some examples:
- In the cervix
- cervical incompetence if the cervix is too narrow or wide, the cervix is duplicated in a possible uterus didelphys, elongated cervix, and so on.
- In the uterus
- structural abnormalities of the uterus (septua, unicornis or bicornuate uterus, etc.), fibroids and uterine polyps, adhesions in a possible Asherman's syndrome, adenomyosis, hypoplasia, etc.
- In the Fallopian tubes
- salpingitis, hydrosalpinx, endometriosis, blocked tubes, etc.
All alterations affecting the Fallopian tubes can cause them to swell and become blocked.
How is hysterosalpingography done?
HSG is a test very similar to an x-ray, in which radiopaque contrast dye is injected into the cervix to view the anatomy of the cervix, uterus, and fallopian tubes through an x-ray machine.
Below, we will discuss all the details to be taken into account when performing a hysterosalpingogram, what it consists of, and how your recovery will be.
Preparation
It is important to make sure that the woman is not pregnant at the time of the hysterosalpingogram, as the x-rays would be harmful to the fetus.
Therefore, the following considerations are very important before doing this test, in addition to other recommendations:
- Performing HSG between days 8 and 10 of the menstrual cycle, when menstrual bleeding is already over and before ovulation occurs.
- Take a laxative or enema the night before or a few hours before the test to empty your bowels. This allows the uterus and tubes to be seen more clearly.
- There is no need to fast since no anesthesia will be administered. However, it is advisable not to eat any food in the previous hours.
- It is possible to take a painkiller earlier to reduce the discomfort of hysterosalpingography.
- A woman should not have this test if she has a genital infection. Her gynecologist may prescribe a pre and post HSG antibiotic to avoid this risk.
There are other contraindications to hysterosalpingography apart from those already mentioned in this section, such as the following: pelvic inflammatory disease, inflammation, metrorrhagia (bleeding between periods), or in the case of having recently ingested a contrast for some other radiological study of the digestive system.
Procedure
Hysterosalpingography is a test that takes approximately 20-30 minutes and is very easy to perform by the medical specialist. In addition, this technique does not require anesthesia.
The placement of the woman will be the same as for a gynecological exam, placing her feet in stirrups, as if she were going to have a simple pap smear.
Once the patient is in the proper position, a speculum will be placed in the vagina so that the cervical area can be washed with a saline solution. Then, through a cannula that will be introduced through the cervix, the contrast dye will begin to be passed into the uterine cavity.
During hysterosalpingography, the woman may feel mild abdominal pain. Some women feel even more intense discomfort. However, these pains disappear once the contrast is stopped.
The x-ray machine will be positioned above the patient's abdomen and will take the necessary images.
Recovery after HSG
After hysterosalpingography, it is not necessary for the woman to rest, although it is also not advisable to do heavy activity during the rest of the day.
The patient may feel slight discomfort during the day of the hysterosalpingogram. If you have more severe abdominal pain, cramping, or other subsequent discomforts, your doctor may prescribe a drug such as buscapine to relieve the pain. It is also possible to have slight vaginal bleeding or brownish discharge during the days following HSG.
In general, it is recommended that the patient continue with her normal life and follow any specific directions from the doctor.
Hysterosalpingography results
The interpretation of the results should be done by a specialist, who is usually the gynecologist who monitors the patient.
In the image obtained, the uterine cavity can be seen as an oval or inverted pear-shaped accumulation and, in addition, two thin lines coming out of the upper part that correspond to the Fallopian tubes.
With regard to tubal permeability, the results of the HSG are summarized as follows:
- HSG Positive
- indicates that the tubes are permeable and therefore contrast is seen to pass through the two tubes and be expelled into the abdominal cavity. Therefore, the patient does not present any alteration.
- HSG Negative
- Whether unilateral or bilateral, it means that one or both tubes are blocked and, as a consequence, do not allow contrast to pass through their structure, causing them to inflate. It is also possible that the Fallopian tubes may not be visible due to a tubal or uterine malformation.
Choosing a fertility treatment
Based on the results obtained from the HSG, in addition to other medical tests, it will be possible to determine which infertility treatment is the most appropriate for attempting a pregnancy.
- Artificial insemination
- as long as the tubes are permeable, the seminal quality is good and the woman has a good ovarian reserve. In addition, the indicated age of the woman to do a successful AI is before the age of 36.
- In vitro fertilization
- is the right choice when the above requirements are not met, i.e. when the tubes are obstructed, the seminal quality is not optimal and the woman is over 36 years of age with the affected ovarian reserve.
Obviously, each particular case must be studied individually and the most appropriate technique must be recommended to the woman or the couple according to their possibilities.
FAQs from users
What are the recommendations prior to hysterosalpingography?
Hysterosalpingography is a radiological procedure that aims to assess the morphology of the uterine cavity, the contours of the endometrium and tubal patency, the latter factor being responsible for between 25 and 35% of the causes of infertility and a necessary aspect to know as part before an artificial insemination procedure.
As it is a somewhat invasive gynecological procedure, it is contraindicated to perform it if the patient has pelvic infection, but even in the absence of it, as a prophylactic measure, the administration of antibiotics is indicated the day or days prior to the study. Likewise, to avoid pain or discomfort after the procedure, it is recommended to take anti-inflammatory analgesic from the night before.

The procedure should be performed in the first half of the menstrual cycle (7 to 10 days after the onset of the last menstrual period) during the proliferative phase of the endometrium, which facilitates the interpretation of the image. In addition, it is recommended not to have unprotected sex in that cycle, which ensures that there is no ongoing pregnancy. Studies performed in the second phase of the cycle may lead to false results.
How is a Hysterosalpingogram performed?
A HSG is a type of x-ray examination that aims to examine the presence of pathologies in the uterine cavity, and well as tubal patency. It is recommended to evaluate potential causes of primary sterility. It involves inserting a cannula until the entrance of the uterus, through which a special radio-opaque contrast material dye is inserted. The contrast material dye will fill in the cavity and the tubes. Then, a series of x-rays will be done to detect potential abnormalities or blockages in the different structures. It is a simple procedure that is typically done in the first 10 days of the cycle. During its performance, the woman may feel period-like symptoms. Hospitalization is not required, and its duration ranges between 15 and 30 minutes approximately.
Can I get pregnant after hysterosalpingography?
Yes, in cases of mild tubal obstruction, the passage of liquid contrast through the tubes during hysterosalpingography may remove the obstruction. Therefore, pregnancy can be easily achieved after hysterosalpingography.
How much does hysterosalpingography cost?
The approximate price of hysterosalpingography is from $200 to approximately $900 depending on the fertility center. However, most insurances cover hysterosalpingography as it is a diagnostic test.
What is virtual hysterosalpingography?
Virtual hysterosalpingography is an advance over the conventional test, in which hysterosalpingography is performed by Multislice Computed Tomography, similar to the CT scan we are all familiar with. The advantages of this new technique are that it does not present any discomfort to the woman, it is non-invasive and, in addition, it offers more complete information with its images.
What are the risks of hysterosalpingography?
Although not very frequent, some complications that may arise as a result of hysterosalpingography are the following: allergic reaction to contrast (iodine), endometritis, salpingitis, perforation of the uterus, etc., in addition to the added risks of any test in which the patient is exposed to x-rays.
Can hysterosalpingography cause changes in premenstrual symptoms and/or menstruation?
The answer is no. No changes in the menstrual cycle should occur, as the ovaries are not compromised. However, some women do experience occasional premenstrual discomfort as a result of the use of contrast fluid.
Read more
Is hysterosalpingography covered by Social Security?
If the woman is eligible for assisted reproduction treatment under the Social Security system, the cost of the hysterosalpingography will also be covered, as well as the other medical tests.
However, it is possible that there is a waiting list for the test and, when the time comes, the woman is not at the ideal time in her menstrual cycle. In that case, the woman can take a pregnancy test to prove that she is not pregnant.
Recommended reading
As we have discussed, the hysterosalpingography test is used to see if the Fallopian tubes are blocked. There can be several causes of tubal obstruction. In the following post, you can find more information about all of them: Blocked Fallopian tubes.
In the event of a positive HSG result, i.e. there are no apparent uterine or tubal problems in the woman, it will be possible to perform artificial insemination to attempt a pregnancy. If you want to learn more about this reproductive technique, we recommend reading the following article: What is AI?
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
Al-Badawi IA, Fluker MR, Bebbington MW. Diagnostic laparoscopy in infertile women with normal hysterosalpingograms. J Reprod Med 1999; 44:953-7.
Broekmans FJ, Kwee J, Hendriks DJ, Mol BW, Lambalk CB (2006). A systematic review of tests predicting ovarian reserve and IVF outcome. Hum Reprod Update; 12:685-718 (View)
Bruna I, Sánchez de Rivera MD, Collado O. Protocolo de diagnóstico básico de la disfunción reproductiva. En: Diagnóstico y prevención de la disfunción reproductiva. Documentos de consenso SEGO, 2011, pp 71-89.
Crosignani PG, Rubin BL. ESHRE Capri Workshop Group. Optimal use of infertility diagnostic tests and treatments. Hum Reprod 2000; 15: 723-732 (View)
Mol BW, Collins JA, Burrows EA, van der Veen F, Bossuyt PM. Comparison of hysterosalpingography and laparoscopy in predicting fertility outcome. Hum Reprod 1999;14:1237-42 (View)
Pellerito JS, McCarthy SM, Doyle MB, Glickman MG, DeCherney AH. Diagnosis of uterine anomalies: relative accuracy of MR imaging, endovaginal sonography, and hysterosalpingography. Radiology 1992; 183:795-800 (View)
Romero Guadix B, Martínez Navarro L, Arribas Mir L. Esterilidad: manejo desde la consulta del médico de familia. AMF. 2002; 8 (6): 304-311 (View)
Swart P, Mol BW, van der Veen F, van Beurden M, Redekop WK, Bossuyt PM. The accuracy of hysterosalpingography in the diagnosis of tubal pathology: a meta-analysis. Fertil Steril 1995;64: 486-91 (View)
FAQs from users: 'What are the recommendations prior to hysterosalpingography?', 'How is a Hysterosalpingogram performed?', 'Can I get pregnant after hysterosalpingography?', 'How much does hysterosalpingography cost?', 'What is virtual hysterosalpingography?', 'What are the risks of hysterosalpingography?', 'Can hysterosalpingography cause changes in premenstrual symptoms and/or menstruation?' and 'Is hysterosalpingography covered by Social Security?'.
Authors and contributors

More information about Michelle Lorraine Embleton













Hi, 3 years ago I had this test and it was perfect. I have repeat abortions, and I should get a pgs treatment since several of the embryos I aborted had chromosomal defects de novo. I am in a clinic that is generally very satisfied, but I notice that they do not give importance to anything that I may have in the uterus. I read many forums here where they go to a particular clinic and ALL the patients seem to have pathologies such as “old” “fibrous” “septate” wombs or with various defects almost as a matter of routine. This makes me have many doubts: either why I don’t have specific exams (I understand that I did many ultrasounds and all of them mention homogeneous miometral structure, I don’t know if it has to do with that), or I never complained about painful periods, or importance is given to the fact that I got pregnant very easily even if the embryo is not good (and the problem is that), or if a hysterosalpingogram is enough to rule out pathologies. Neither did I ever have a curettage or an STD, all abortions were resolved with misoprostol and controlled by subsequent ultrasound, without anything conspicuous.
I wanted to know your opinion on this, in itself, about when the uterus is analyzed or when you suspect that you have abnormalities or if there is some kind of overdiagnosis.
Hi Gypsy,
Normally, when doing routine exams such as ultrasounds and hysterosalpingographies, gynecologists can see if there are any abnormalities in the uterus. Therefore they rule out using other diagnostic techniques more specific to the uterus because they do not see the need for them and there are no indications for them.
In your case, repeated abortions can have different causes. But the most frequent cause is due to chromosomal alterations. It is true that a uterine abnormality can affect the embryo and produce an abortion, but it is your gynecologist who must have previously ruled out these pathologies through a gynecological study. In any case, you should talk to your gynecologist and tell her about your concerns, perhaps she can help you and give you all the information about whether it is necessary to do additional studies of the uterus in your case.
Hope this answers your question,
all the best
Hi, my gynecologist ordered the study but I have to make an appointment when I have my period and it doesn’t come if I don’t induce it, can it be done anyway? Or do I have to menstruate? Thank you
Hi Marula,
You can get tested for HSG even if you are not on your period. The important thing is to make sure that you are not pregnant at the time of the test, as this could affect the development of the fetus.
Best regards
Hello, I had been trying to get pregnant for almost 3 years, I had an HSG at the end of May 2010 and I was advised not to have sex on my fertile days in June so that my body would be cleaned of the contrast fluid that might be left inside, after that I waited again for my fertile days and finally in July of that year I got pregnant, I could not believe it, my exam was good, I didn’t have obstructed tubes but I think that something made that exam in me because I got high, I must admit that it hurt a lot but it was worth all the suffering, today my daughter is 4 years 7 months old, now I have been 10 months without taking care of myself and nothing has happened, I took another HSG on 26/09/2015 and I am 2 days overdue, don’t lose hope I believe that this exam is worth it.
I have a 3 and a half year old baby, but since I didn’t get pregnant on the 2nd, I started going to the OB/GYN. At first everything was fine, hormones, semen analysis and everything… But we’ve had two AI’s and eight months of trying and nothing happend… Today I have done the hysterosalpingography and is bearable, uncomfortable because you feel pressure to the passage of contrast, but it is bearable. My question is: if I had it done at the 9th, can I still have sex?
Hi Erin,
It is advisable to let a few days pass after HSG to have sex. Two or three days would be enough to have the contrast fluid completely removed.
Hope I could help you,
Best regards
Good afternoon! How are you? I wanted to comment on my case, I made the hysterosalpingography this Monday and when I left there great, the only problem was that I had no compress in the bag and was stained all over and I began to notice some symptoms, small cramps, nausea and when I went to pee,A drop of blood came out but this morning the cramps became worse, my stains are already abundant and nausea disappeared, but I am concerned because I do not know if it is normal to have this pain and heavy bleeding, I would appreciate your help, thanks!
I didn’t have any problem at all, I noticed a slight discomfort, but it wasn’t painful, and the truth is that it’s a good thing they did it to me because my tube was slightly obstructed and thanks to the test it came out and I was able to get pregnant naturally.
Hello,
I want to share with you my experience, because I was very afraid of the test, but it was really not much more than a nuisance. The doctor told us earlier that there are cases where women get pregnant later, and that was my case! In fact twice, the first baby I lost but I got pregnant right away again and I’m 5 months pregnant now 🙂 Cheers everyone!
I had that study done and it came out fine my tubes are neither clogged nor covered