Vasectomy is a method of male sterilization that involves the section and ligation of the male's vas deferens through a surgical procedure.
This is a permanent method of contraception, as it prevents the sperm from leaving with the ejaculate and therefore prevents pregnancy.
The effectiveness of vasectomy is very high and has few side effects. In addition, in most cases, it is reversible through a so-called vasovasostomy. However, its effectiveness will depend on the way the vasectomy was performed and the time that has elapsed.
Provided below is an index with the 8 points we are going to expand on in this article.
- 1.
- 1.1.
- 2.
- 2.1.
- 2.2.
- 3.
- 4.
- 5.
- 5.1.
- 5.2.
- 5.3.
- 5.4.
- 5.5.
- 5.6.
- 5.7.
- 6.
- 7.
- 8.
How is vasectomy done?
Vasectomy is a surgical procedure that involves blocking the vas deferens (channels that carry sperm ) of the male reproductive system so that sperm is stopped from passing from the testicles to the urethra.
After ejaculation, the sperm will be stored in the epididymis instead of coming out, and will eventually be reabsorbed by the body itself.
Vasectomy does not alter sperm production (spermatogenesis) or hormone production. It only prevents the sperm from leaving the semen in order to avoid pregnancy.
To perform a vasectomy, surgical intervention is necessary that lasts about 20 minutes and can be carried out in two basic ways that are discussed in the following section.
Types of vasectomy
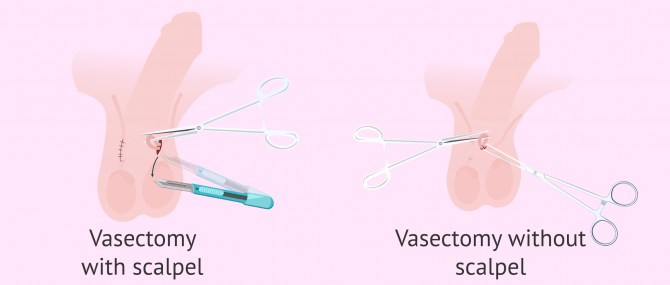
There are two ways to perform a vasectomy on a male, an incisional method and a non-incisional method. Each of the possibilities is detailed below:
- Scalpel Vasectomy
- through a cut in the scrotum (pouch of the testicles), the surgeon accesses the vas deferens, binds it and cuts it, thus blocking the passage of the sperm. You can also cauterize them with an electric scalpel.
- Vasectomy without scalpel
- instead of using the scalpel to make a cut, simply make a small hole with special pliers to reach both vas deferens. First, the surgeon will look for the vas deferens by palpation of the scrotum and will hold it in place with ring-shaped forceps. Then, with sharper tweezers, a tiny puncture is made to allow access to the vas deferens to bind or cauterize it.
In both cases, local anesthesia is used to do the procedure. Finally, the remaining hole is sealed with a stitch or surgical rubber.
The operation without a scalpel is less uncomfortable for the patient since the size of the hole made is smaller, bleeding is less and it takes less time to heal. Also, the risks of infection or other complications are less.
After vasectomy
Recovery from vasectomy surgery is rapid. The man will only need to rest for a few days for the wound to heal properly.
Some men have described feeling discomfort, some pain or swelling in the testicles. However, these symptoms are not intense.
In addition, before the vasectomy is performed, the man should be aware that this method of definitive sterilization also has other advantages and disadvantages that may arise in the future.
Advantages
Vasectomy effectiveness is close to 100%. Once 3 months have passed since the operation and it is proven that the man has no sperm in his semen through a seminogram, the possibility of pregnancy will be almost nil.
This will allow the couple to enjoy sex more, as concerns about a possible unwanted pregnancy disappear.
It should be noted that vasectomy does not prevent ejaculation. The semen will have the same volume and composition from the secretions of the prostate and the seminal vesicle. However, the vasectomized male will go into a situation of azoospermia, that is, the total absence of sperm in the semen.
Vasectomy is a simpler, safer, and more effective procedure than tubal ligation for women. In addition, it is also cheaper and, for all this, it is the preferred option among couples who do not wish to have more children.
Vasectomy also does not influence a man's sexuality or masculinity. Vasectomized men have the same sexual desire and erection capacity as they had prior to the operation.
Another advantage of vasectomy is that it is a simple procedure, with negligible side effects and few risks.
Disadvantages
The effectiveness of vasectomy is not immediate. In order to guarantee the complete absence of spermatozoa in the ejaculate, a period of about three months or more than 20 ejaculations is required after the operation.
To check that the semen is indeed already free of sperm, it will be necessary to perform a post-vasectomy control semen analysis. Although it is a simple surgical operation, it is not totally risk-free. There are specific situations in which the man may feel a swelling or more acute discomfort in the testicular area, as well as being able to suffer from orchitis.
Another disadvantage as a contraceptive method is that it does not protect against sexually transmitted diseases. Therefore, it is recommended to use a condom in case of casual sex with different women.
Finally, something that is an advantage for some and a disadvantage for others is that it is permanent. While it is true that vasectomy can be reversible, this option is more complicated and does not always allow for the recovery of reproductive capacity.
Post-vasectomy treatment
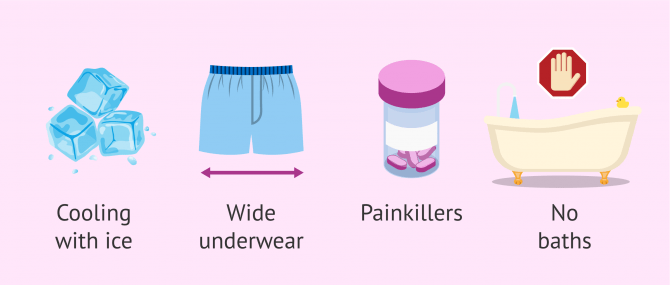
As we have said, vasectomy is a simple operation, but it can cause some discomfort in the first few days. Therefore, it is recommended that the patient not make great efforts, especially in cases of vasectomy with a scalpel.
If the man has a job that involves heavy physical exertion or a lot of walking, he may need to take time off work for about a week. If the scrotal area is quite painful, it is recommended to apply ice for about 15 minutes and take painkillers, except for aspirin, which is an anticoagulant.
Furthermore, it is recommended that the wound be treated about twice a day, as indicated by the specialist. Normally, the cure is done with saline, betadine and gauze.
It is advisable to be careful when showering and to avoid baths. It is also important to wear loose-fitting clothing and underwear to avoid testicular swelling.
Finally, it is important to avoid ejaculation for at least the first 7 days, as it can be painful and cause bleeding from the wound.
Vasectomy and pregnancy
As we have already mentioned, vasectomy is a surgical contraceptive method that prevents pregnancy permanently. It is therefore essential that the man who is to undergo this intervention should be clear that he does not wish to have any more children.
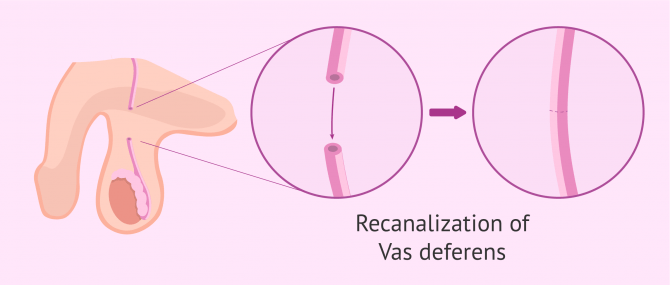
Despite this, there are many men who change their minds and, after a while, want to reverse the vasectomy so they can become parents.
The operation to recanalise the vas deferens and allow sperm to pass back into the urethra is known as vasovasostomy. It's more complex and lasts longer than a vasectomy. In addition, its success will also depend on the way the vasectomy was performed and the time that has passed since the surgery.
The probability of regaining fertility after vasovasostomy is high and many men have achieved natural pregnancy again. Still, this has not always been possible.
There are other options related to assisted reproduction so that men with the vasectomy done can be parents again. Below, we are going to detail reproductive alternatives:
- In vitro fertilization (IVF) with sperm obtained from testicular biopsy or epididymis aspiration.
- Sperm donation for artificial insemination (AI) or IVF depending on the characteristics of the woman.
If you need to undergo IVF to become a mother, we recommend that you generate your Fertility Report now. In 3 simple steps, it will show you a list of clinics that fit your preferences and meet our strict quality criteria. Moreover, you will receive a report via email with useful tips to visit a fertility clinic for the first time.
Although all these techniques allow pregnancy to occur again, it is always advisable to think through the decision to have a vasectomy.
You may also want to consider freezing your sperm before your vasectomy. This is a method of preserving male fertility that would allow a biological child in the future with a simpler treatment
FAQs from users
When is it recommended to check if the vasectomy has been effective?
A seminogram is usually requested three months after the vasectomy. Given that the period of production of the sperm is approximately 3 months, if azoospermia is proven after this period, it is possible to deduce that the testicle is functioning at full capacity after the surgery and that the section has been a success since no sperm reaches the exterior.
Which fertility treatment is best for patients who have had a vasectomy?
Vasectomy is a permanent surgical contraceptive method that consists of blocking the vas deferens (channels that transport the semen) of the male reproductive system so that the passage of sperm from the testicles to the urethra is interrupted. This procedure is considered irreversible.
On some occasions, vasectomized men wish to have children again, for which they can resort to various treatments:
- Vasovasostomy. Intervention to recanalise the vas deferens and allow sperm to pass back into the urethra. It is a complex procedure and the result will depend on the way the vasectomy was done, as well as the time that has passed since it was performed. Its success rate is much lower than the success rate with an in vitro fertilization treatment. It has the disadvantage that once pregnancy has been achieved, the patient must undergo another vasectomy if he does not wish to have any more offspring.
- In vitro fertilization (IVF) with sperm obtained from testicular biopsy or epididymis aspiration
- Sperm donation for artificial insemination (AI) or IVF depending on the characteristics of the woman.
What is the risk of pregnancy after vasectomy?
The likelihood of pregnancy in a couple where the man has had a vasectomy is virtually zero. There is a possibility that the tubes may recanalize on their own, but this occurs rarely and, moreover, with current surgical methods it is very rare.
It is important to remember that pregnancy can occur in the first few months after a vasectomy, so it is recommended that an additional method of contraception be used.
Can epididymitis be a complication of vasectomy?
Yes. Once a vasectomy is performed, a man may feel a sense of heaviness or discomfort in the genital area. In addition, he may have some testicular inflammation and pain, which could lead to epididymitis.
In these cases, it is essential to inform the specialist so that he can establish the best treatment for each particular case and some advice on how to alleviate the patient's symptoms.
How much does a vasectomy cost?
In the United States this procedure can cost anywhere between $300 to $3,000, depending on who and where you chose. Some health insurance plans do cover part of all of the costs so be sure to check this first.
In most parts of the UK you can have a vasectomy free of charge on the NHS, but waiting lists can be long. If you choose to go private then expect to pay between £500 and £2000 depending on your choice of clinic.
In Spain, a vasectomy costs between €500 and €1000, and the price will vary from clinic to clinic so it is worth doing some investigation first. It is also offered under the social security system for public health.
Is a vasectomy always bilateral?
Yes, it is necessary to cut both vas deferens to safely avoid pregnancy. If this were done unilaterally, the ejaculate would contain sperm from the non-vasectomized testicle.
When can I have sexual intercourse after vasectomy?
Normally, the man can have sex one week after the operation, as long as there is no discomfort. If sexual intercourse is uncomfortable, it is advisable to wait a few more days.
It is also important to remember that for the first few months after the operation there is still a risk of pregnancy. Therefore, it will be necessary to use other contraceptive methods.
Recommended reading
Vasectomy is not irreversible. If you decide to become a father again, you can evaluate the options we discussed in the following post: Is pregnancy possible with vasectomy?
We have discussed tubal ligation as a method of female sterilization. You can get more information about this in the following article: What is tubal ligation?
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
Shih G, Turok D, Parker W. Vasectomy: the other (better) form of sterilization. Contraception. 2011 Apr;83(4):310-5. doi: 10.1016/j.contraception.2010.08.019. Epub 2010 Oct 8.
Sooltangos A, Al-Ausi M. Local anaesthetic vasectomy is not as painful as patients expect. BMJ Sex Reprod Health. 2020 Jul;46(3):234-235. doi: 10.1136/bmjsrh-2019-200462. Epub 2019 Dec 26.
Weiske W. Vasectomy. Andrologia. 2001 May;33(3):125-34. doi: 10.1046/j.1439-0272.2001.00445.x.
FAQs from users: 'When is it recommended to check if the vasectomy has been effective?', 'Which fertility treatment is best for patients who have had a vasectomy?', 'What is the risk of pregnancy after vasectomy?', 'Can epididymitis be a complication of vasectomy?', 'How much does a vasectomy cost?', 'Is a vasectomy always bilateral?' and 'When can I have sexual intercourse after vasectomy?'.
Authors and contributors


More information about Michelle Lorraine Embleton





Hi
I had my vasectomy in March 2022 and I still have some discomfort when having intercourse. Is this normal?
Hi Frank74
I am sorry to hear you still have some discomfort. Although this is rare, Post-Vasectomy Pain Syndrome does exist, and can be caused by, for example, nerve compression, scar tissue or infection. If it become painful, or to put your mind further at rest, we recommend you contact your health provide to ensure eveything is ok.
I hope this answers your question
Hello!
Can someone help me? My girl and I are thinking about vasectomy but we are afraid it might have a bad effect on my sperm quality when we later decide to get children.
Hi Omar,
a vasectomy has an effect on semen in such a way that it ensures that no sperm cells are present in the ejaculate. This, however, doesn’t affect the quality of your sperm at all. Should you, therefore, get a vasectomy reversal, you can get a woman pregnant again.
However, you also have the option of sperm freezing before your vasectomy procedure and conceive through IVF. This makes a reversal redundant. Read more about your pregnancy options here: how to conceive after a vasectomy.
Hope this helps
All the best.
I just had a vasectomy. When can I safely start having intercourse again?
Hi Steve,
it is recommended to let pass at least 72 hours from the operation, because although it is simple can lead to some discomfort. In any case, it depends on how each patient recovers.
As for safety regarding the possibility of pregnancy, I advise you to use a barrier method such as a condom until you have verified, by means of a seminogram, that there are no spermatozoa in your ejaculate.
Best wishes