Polycystic Ovary Syndrome (PCOS) is an endocrine disorder that affects the female reproductive tract by causing abnormalities in sex hormone levels.
For this reason, about 75 percent of women with PCOS have infertility problems and find trouble when attempting to get pregnant.
The main symptom of this endocrine cause of female infertility is anovulation, that is when the ovaries are unable to release an oocyte during the menstrual cycle.
Provided below is an index with the 6 points we are going to expand on in this article.
- 1.
- 1.1.
- 1.2.
- 2.
- 2.1.
- 2.2.
- 3.
- 3.1.
- 3.2.
- 3.3.
- 3.4.
- 3.5.
- 3.6.
- 3.7.
- 3.8.
- 4.
- 5.
- 6.
PCOS & infertility
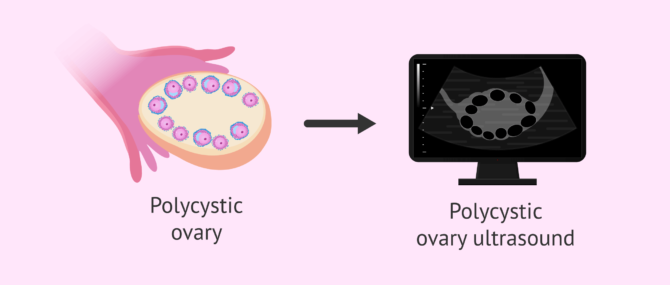
PCOS is the most common endocrine disorder in women of childbearing age. It is diagnosed in about 5-10% of women after seeing multiple antral follicles with a common pattern through an ultrasound scan.
Nonetheless, a hormone analysis is the only test that can render a conclusive diagnosis of PCOS, since this disorder causes abnormalities in sex hormone levels.
The following are the main signs and symptoms of PCOS, which are linked to infertility issues in females.
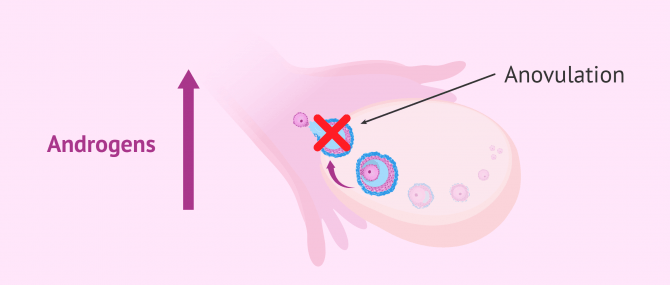
Anovulation
In PCOS patients, menstrual irregularities (including abnormalities during menstruation or amenorrhea), are an indicator of anovulation (absent ovulation).
Chronic anovulation is the main clinical sign of Polycystic Ovary Syndrome (PCOS).
The reason why the woman lacks ovulation is an imbalance in FSH and LH levels, the hormones that are in charge, or regulating the menstrual cycle. Specifically, increased FSH levels trigger follicle development. Then, the LH surge causes the egg to be released during the ovulation phase of the cycle.
Abnormalities in FSH and LH levels are associated with the following abnormalities as well:
- Hyperandrogenism
- Since stimulation of FSH production does not occur, androgens do not become estrogens due to the action of aromatase enzyme. As a result, the levels of male hormones in blood are too elevated, causing side effects such as hirsutism.
- Insulin resistance
- High insulin concentrations in blood contribute to increasing the levels of androgens, and therefore to aggravate the situation of anovulation.
Finally, diminished FSH levels, and the subsequent lack of estrogens, cause the follicles to become atretic, forming cysts in the ovaries.
If you liked this section, you may want to go through this: What Is Anovulation?
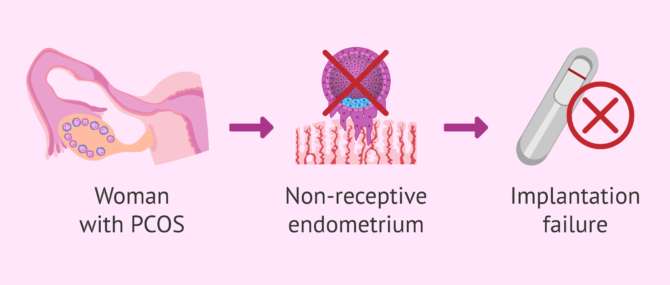
Endometrial receptivity
In addition to ovulation and fertilization to create a new embryo, endometrial quality is crucial for embryo implantation and development to occur.
The endometrial lining (endometrium) renews and becomes receptive monthly thanks to the effect of estrogens and progesterone, both produced by the ovaries.
As already explained, the synthesis of estrogens and progesterone is altered is women with PCOS.
As a consequence of these abnormalities, endometrial receptivity is significantly lower in PCOS patients, and hence the chances for the embryo to attach to the uterus, causing implantation failure.
Risks of undergoing fertility treatment
Due to the number of infertility problems caused by PCOS, many women decide to undergo ovarian stimulation with ovulation induction to be able to get pregnant.
Although these treatment options are recommended by reproductive endocrinologists, they are not risk-free due to an elevated amount of follicles in the ovaries. The following are the main side effects:
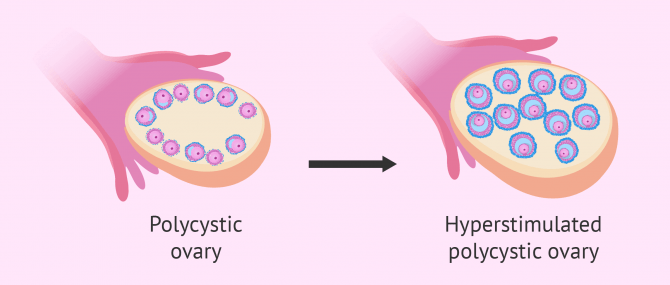
Ovarian hyperstimulation syndrome
Ovarian Hyperstimulation Syndrome (OHSS) is an excessive response of the ovaries to ovarian stimulation drugs.
Since women with PCOS have an exaggerated number of antral follicles, the risk of developing OHSS is higher for them.
Thus, reproductive endocrinologists should monitor the ovarian stimulation cycle more closely in these patients using ultrasound scans as well as measuring estradiol levels in the blood.
In the most severe cases of OHSS, the patient has symptoms of ascites (pathologic fluid collection within the abdomen), a rapid weight gain, tachycardia, and breathing difficulty.
More on this story: What Is the Ovarian Hyperstimulation Syndrome (OHSS)?
Multiple pregnancy
The risk of getting pregnant with multiples is a key aspect to consider when a couple undergoes timed intercourse or IUI (intrauterine insemination) and there exist more than 2 or 3 mature follicles in the ovaries.
For this reason, very low doses of hormone medications should be prescribed. If despite this, more follicles than desired develop, the cycle will have to be canceled, and the patient must have protected sexual intercourse.
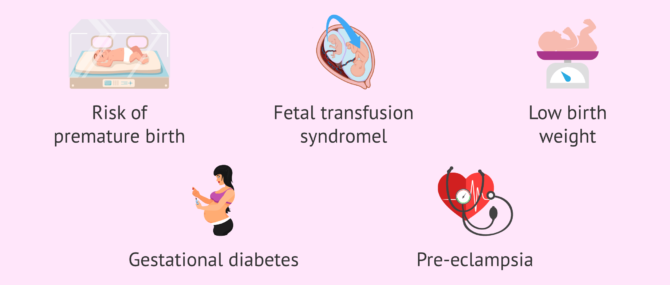
The following are the main complications of multiple pregnancies:
- Increased risk of preterm birth
- Twin-to-twin transfusion syndrome (TTTS)
- Low birth weight
- Increased likelihood of placental complications
- Increased maternal weight during pregnancy
- Gestational diabetes and preeclampsia
Related content: Multiple Pregnancy Risks.
Considering seeing a fertility specialist? Don't forget that, in the field of Reproductive Medicine, as in any other medical area, it is crucial that patients rely on the doctors and staff that will help them through their treatment cycle. Logically, conditions vary from clinic to clinic. For this reason, we recommend that you generate your Fertility Report now. It will offer you a list of clinics that have passed our rigorous selection process successfully. Furthermore, the system will make a comparison between the fees and conditions of each clinic so that you can make a better-informed decision.
FAQs from users
Are PCOS and female infertility related?
Yes, they're related. Polycystic Ovary Syndrome is a hormonal and metabolic condition that affects ovarian function. One of the most characteristic symptoms is irregular menstruation, present in 70% of patients with PCOS. These are women who usually have long menstrual cycles, even some months without a period because ovulations are altered or even absent. If there is no ovulation or ovulation does not occur normally every month, the chances of pregnancy are lower.
It is described that due to PCOS 40% of these women will consult for fertility problems. When this happens, an exhaustive study must be carried out to assess which treatments can improve the fertility of each woman naturally, and when we should start a reproduction treatment in each case.
Why are AMH levels so high in women with PCOS?
Anti-Müllerian hormone (AMH) is produced by pre-antral and antral follicles present in the ovaries. For this reason, PCOS patients usually have too elevated AMH levels (about 6 ng/ml approximately).
What are the risks I should expect during pregnancy if I have PCOS?
Some studies have shown that women with PCOS have a greater risk of miscarrying. Moreover, there are other obstetric complications to keep in mind, including:
- Gestational diabetes
- Preeclampsia
- Low birth weight
- Preterm birth
- C-section
For these reasons, women with PCOS are more likely to go through a high-risk pregnancy.
Read more
I have PCOS but my body mass index is normal, should I lose weight to improve my insulin levels?
Diet and physical exercise to lose weight are general recommendations in cases of PCOS where, additionally, the woman is overweight. If you are already on your weight, you do not need to start a weight loss diet plan. In fact, losing weight can even worsen the situation.
What additional metabolic disorders are associated with PCOS?
Aside from the ones already listed, hyperinsulinemia associated with PCOS leads to the development of other long-term metabolic disorders, such as:
- Diabetes type II
- Cardiovascular risks
- Obesity, increased triglyceride, total cholesterol and LDL levels
- Endometrial hyperplasia and gynecological cancer
I have PCOS and I am about to undergo IVF, what are my chances of getting pregnant with multiples?
In this case, the chances of having a multiple pregnancy do not rise due to PCOS, since it depends on the number of embryos transferred.
If a woman with PCOS undergoes a different treatment, namely timed intercourse or intrauterine insemination, the risk of multiple pregnancy would increase, though. In these cases, it is not possible to monitor the exact number of eggs released.
What treatment options can help you get pregnant with PCOS?
The best treatment option depends on the results of your hormone analyses and the gynecological examination. Firstly, you can try with a change in lifestyle habits, which can be helpful to regulate the menstrual cycle. If this does not work to overcome anovulation, you may be prescribed a series of drugs to induce ovulation. Finally, if none of these treatment options work, you may be required to undergo a fertility treatment, such as IUI or IVF, if needed.
Why does a woman with PCOS have an increased risk of having gestational diabetes than a healthy woman?
A pregnancy is a natural physiological state that generates insulin resistance. Insulin, due to the many changes induced by the pregnancy, becomes less effective and the organism needs to produce it in higher amounts for glucose to be effectively absorbed.
On the other hand, insulin resistance is a common symptom of PCOS. So, if both situations occur simultaneously (pregnancy and PCOS), the chances for the woman to develop gestational diabetes or type II diabetes in the future increase.
Suggested for you
If you are trying to conceive but you suffer from PCOS, we strongly recommend that you have a look at this post: What Are a Woman’s Chances of Conceiving with PCOS?
Also, if you need further information on the possible treatment options of PCOS, continue reading here: What Are the Different Treatment Options for PCOS?
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
Anttila L, Karjala K, Panttila RA, et al. PCOS in women with gestational diabetes. Obstet Gynecol 1998; 92: 13-16
Balen AH, Conway GS, Homborg R, Legro RS. PCOS – A Guide to Clinical Management. London: Taylor & Francis 2005.
Balen, A.H., Dresner, M., Scott, E.M., Drife, J.O. (2006). Should obese women with polycystic ovary syndrome receive treatment for infertility? BMJ, 332, 434-435 (See)
Diamanti-Kandarakis, E. (2006). Insulin resistance in PCOS. Endocrine, 30(1), 13-17 (See)
Dunaif A. Insulin resistance and the polycystic ovary syndrome: mechanism and implications for pathogenesis. Endocr Rev 1997; 18(6): 774 (See)
Franks S. Polycystic ovary syndrome. N Eng J Med 1995; 333: 853-86 (See)
Golan A, Ron-El R, Herman A, Sofer Y. Ovarian hyperstimulaion syndrome: an update dreview. Obstet Gynecol Surv 1989; 44: 430-40.
Kiddy DS, Hamilton Fairley D, Bush A, et al. Improvement in endocrine and ovarian function during dietary treatment of obese women with PCOS. Clin Endocriol 1992; 36: 105-11 8 (See)
Portsky L. On the paradox of insulin induced hyperandrogenism in insulin resistant states. Endocr Rev 1991; 12: 3-13.
Schenker JG, Ezra Y. Complications of assisted reproduction techniques. Fertil Steril 1994; 61: 411-22.
Urman B, Sarac E, Dagan L, et al. Pregnancy in infertile PCOD patients, complications and outcome. J Reprod Med 1997; 42: 501-5
FAQs from users: 'Are PCOS and female infertility related?', 'Why are AMH levels so high in women with PCOS?', 'What are the risks I should expect during pregnancy if I have PCOS?', 'I have PCOS but my body mass index is normal, should I lose weight to improve my insulin levels?', 'What additional metabolic disorders are associated with PCOS?', 'I have PCOS and I am about to undergo IVF, what are my chances of getting pregnant with multiples?', 'What treatment options can help you get pregnant with PCOS?' and 'Why does a woman with PCOS have an increased risk of having gestational diabetes than a healthy woman?'.
Authors and contributors




Hello, I have polycystic ovaries but I’ve been on birth control pills for almost a year now, although I’ve recently had brown discharge for about two weeks and a small period with clots but I’m a week away from my period. However, I have a swollen stomach and a lot of cravings! Tell me what it could be?! Thanks
Can someone please advice me?
my husband has 8 million spermatozoa x ml
and total number of 18,2000,000
cells: few precursor cells at different stages of maturation.
color : colorless slightly opaline
aspect: homogeneous liquefied in the first hour
reaction: alkaline
ph: 8.4
volume 2.1
the translational mobility 75% are alive until the eighth hour and 24 hours there is 0% .
vibratory mobility 5% up to 24 hours .
mobility none 25% until the eighth hour and 95% at 24 hours .
positive fructose test
normal morphology: 94%.
elongated head:2,1%
amorphous head: 2,1%
others:2,2%
esosine test: 15%
(a natural pregnancy can be achieved if you only have 2 days of sexual intercourse)
And what are the odds of pregnancy if those two days were fertile
because I want to get out of a doubt cause my husband has a child of his own and he was only with the girl for 2 days and we have not been able to have children for more than three years and according to the doctor he told me that I am fine.
Hi, my name is Jennifer. I’m 27 years old. I have Polycystic Ovaries plus a reversed uterus and amenorrhea. I used to have periods every 4-6 months. but lately I’ve been improving my diet and exercising. so I’ve seen results and I’ve had periods every other month. I have calculated my fertile days with an online application but I experienced brown secretions followed by light pink secretions. I thought it might be a sign of implantation, so I took a urine test and it came back negative. Is a false negative possible? I don’t like to use medications and hormones I think cause harm that another natural solution recommends? Thank you in advance.