Yes, diet can significantly influence female fertility. Scientific evidence suggests that certain dietary patterns and adequate nutrient levels are associated with better ovarian function, more efficient hormonal regulation, and higher reproductive success rates, both naturally and in assisted reproduction contexts.
Female fertility is the result of a complex interaction between hormonal, metabolic, immunological,and environmental factors. Among these, nutrition plays a prominent role. Today, numerous scientific studies support the idea that eating habits significantly affect ovarian function, oocyte quality, embryo implantation, and ultimately, the ability to conceive and sustain a pregnancy.
From a physiological perspective, diet is involved in regulating the hypothalamic-pituitaryovarian axis, which controls the menstrual cycle and ovulation. Nutritional extremes, such as being underweight or obese, can disrupt this axis. Obesity, in particular, is associated with chronic inflammation, insulin resistance, and hormonal dysfunction, all of which can impair ovulation and oocyte quality. On the other hand, severe caloric deficits, as seen in women with eating disorders, may lead to functional hypothalamic amenorrhea, a common cause of infertility.
The composition of the diet also plays a key role. Diets high in simple carbohydrates and with a high glycemic index can promote insulin and androgen imbalances, hindering ovulation. Conversely, diets rich in complex carbohydrates and fiber improve insulin sensitivity and support more regular menstrual cycles. Similarly, higher intake of plantbased proteins over animal proteins, as well as a balanced intake of fats (prioritizing unsaturated fats and reducing trans fats), can improve the metabolic and hormonal environment.
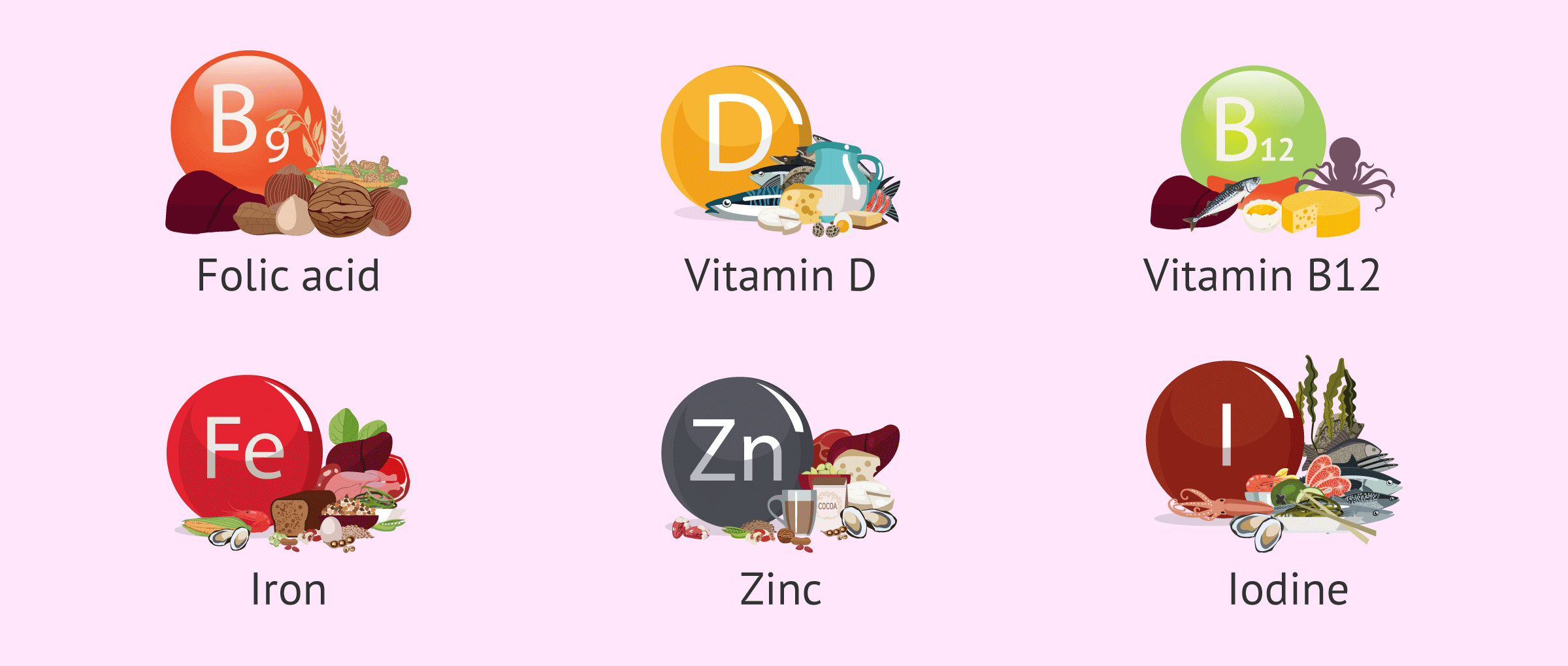
Micronutrients are equally essential. Vitamins such as folic acid, D, and B12, along with minerals like iron, zinc, selenium, and iodine, play a crucial role in ovulation, implantation, and embryo quality. Deficiency in these elements—even when not clinically evident—can silently impair fertility. Moreover, oxidative stress (processes that damage cellular genetic material, including oocytes) can be reduced with a diet rich in natural antioxidants found in fruits, vegetables, extra virgin olive oil, nuts, and other plant-based foods. Beyond isolated nutrients, what appears particularly relevant is the overall dietary pattern. In this regard, the Mediterranean diet has been recognized as a nutritional model associated with improved fertility rates. This diet, characterized by high intake of vegetables, legumes, fruits, whole grains, fish, and olive oil, and moderate consumption of animal products, is associated with lower systemic inflammation, better hormonal profiles, and higher pregnancy rates, both naturally and in assisted reproductive technologies such as in vitro fertilization (IVF).
In specific clinical contexts, such as polycystic ovary syndrome (PCOS), dietary intervention is the firstline treatment. Improving insulin sensitivity and reducing body weight through nutrition has been shown to increase spontaneous ovulation and enhance response to fertility treatments. In IVF, several studies have shown that women who follow healthy dietary patterns achieve higher fertilization, implantation, and full-term birth rates.
Additionally, healthy eating habits are often accompanied by other fertility-supportive behaviors, such as good sleep hygiene, lower alcohol and tobacco consumption, and a more proactive attitude toward self-care. These factors, though indirect, also influence reproductive health.
From our perspective at INEBIR, diet should not be seen as an isolated factor, but rather as a powerful tool within a comprehensive approach to female fertility. Adopting a balanced dietary pattern based on scientific evidence can enhance ovarian function, optimize oocyte quality, and support a more receptive uterine environment. Nutrition, therefore, not only nourishes the body but can also serve as a silent yet decisive ally on the path to motherhood.
