If a couple has been trying to conceive for 12 months without achieving pregnancy, it could be that there are some underlying fertility problems. At this point, the couple should visit a specialist who will order several tests to perform a fertility study.
For men, the male fertility study par excellence consists of the sperm analysis or spermogram, which analyzes the quality of the semen, and a sperm count. However, there are other additional studies, such as hormonal testing, karyotyping or FISH of spermatozoa, among others.
Once the cause of infertility has been discovered, it is possible to choose the most appropriate fertility treatment in order to achieve pregnancy.
Provided below is an index with the 10 points we are going to expand on in this article.
- 1.
- 2.
- 3.
- 3.1.
- 3.2.
- 4.
- 5.
- 5.1.
- 5.2.
- 5.3.
- 5.4.
- 5.5.
- 5.6.
- 6.
- 7.
- 7.1.
- 7.2.
- 7.3.
- 7.4.
- 7.5.
- 7.6.
- 7.7.
- 7.8.
- 7.9.
- 8.
- 9.
- 10.
How do you get tested for infertility?
The first step is for the couple to attend a fertility clinic. In general, it is recommended to visit a specialist when the couple has been having regular unprotected sex for at least one year and are unable to get pregnant.
From here, the doctor will ask a series of questions to create a medical history and will request tests for both members of the couple. The objective is to determine the cause of infertility and thus decide on the best treatment.
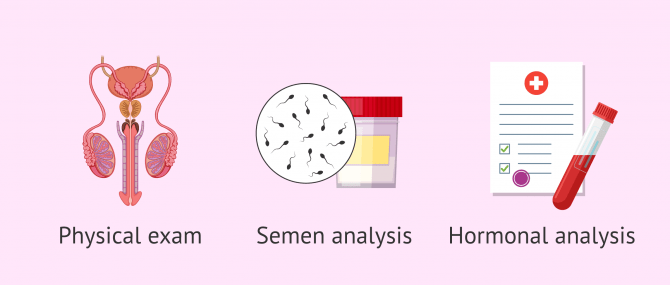
Specifically, the basic tests for a male fertility study are as follows:
- Physical exploration to see his general health status and that of his sexual organs.
- Semen analysis to assess sperm quality.
- Hormone analysis to determine if there is any alteration in the male sex hormones.
It should be noted that male fertility evaluation should always be personalized. Therefore, the tests that are carried out depend on each individual.
If you have doubts or queries about the results of your fertility tests or the tests you should undergo to have your fertility checked, do not hesitate to ask here: Male infertility and men's fertility forum.
Assisted procreation, as any other medical treatment, requires that you rely on the professionalism of the doctors and staff of the clinic you choose. Obviously, each clinic is different. Get now your Fertility Report, which will select several clinics for you out of the pool of clinics that meet our strict quality criteria. Moreover, it will offer you a comparison between the fees and conditions each clinic offers in order for you to make a well informed choice.
Physical examination
The first test that the man undergoes is a physical exam. This is to dismiss the possibility of infertility due to problems of the testes or related with ejaculation.
To this end, the urologist can perform the following exams:
- Measurement of weight and height
- Abdomen and groin exploration
- Genitalia and prostate examination
- Evaluation of the testis, including testicular size and consistency
- Testicular ultrasound
The goal is rule out anatomical problems that could be causing infertility and evaluate whether the male has ejaculation problems or diseases. If the cause of infertility is not found through these examinations, the next step is to carry out a semen test.
Semen analysis
A semen analysis, also known as sperm test, seminogram or semenogram, is a study of the sperm to determine its quality. For this test to be accurate 3 to 5 days of abstience is required before providing the sample.
The World Health Organization (WHO) establishes minimum values for a normal semen sample. Depending on the results of the seminogram, we can know if there are any pathologies or if the semen is normal (normozoospermia).
If the results show abnormalities in the sperm, we can then categorize the condition from which the man suffers according to the alterations observed.
Macroscopic study
When a macroscopic analysis of the semen is performed, basic characteristics of the sperm are analyzed with the naked eye without using a microscope.
The following is a list of seminal parameters that can be analyzed through a macroscopic study:
- Volume
- the normal amount of semen per ejaculate is between 2 and 4 mL. However, this value can vary according to days of abstinence, stress, etc.
- Liquefaction
- occurs after allowing the semen sample to rest for approximately 20 minutes.
- Color
- the semen should have a yellowish-gray color; if it looks different, it may indicate infection.
- Viscosity
- the presence of threads in the sample is evaluated.
- pH
- the values for a normal sperm pH are between 7.2 and 8.0, i.e. a basic pH..
Taking into account this simple semen analyses, it is not complicated for the patient to interpret the results of the seminogram by himself.
Microscopic study
The microscopic study of the semen consists of analyzing a small sample under the microscope. The most important seminal parameters that are examined in the semen analysis are:
- Sperm motility
- For the sperm to reach the egg and fertilize it, they should move forward rapidly and progressively.
- Sperm concentration
- Refers to the sperm count per milliliter of ejaculate or in the entire sample.
- Sperm morphology
- Sperms with abnormal forms will find moving forward and the obstacles of the female reproductive tract more complicated to navigate.
- Sperm vitality
- Sometimes, a sperm test shows the presence of dead sperm in the ejaculate, which are incapable of fertilizing an egg. This parameter is determined when there is a large number of immotile spermatozoa.
- Presence of leukocytes
- Would be indicative of a possible infection.
Do you want to learn more about the seminogram test? Learn about it in detail with the following guide: Semen analysis: procedure, cost and interpretation.
If you need to undergo IVF to become a mother, we recommend that you generate your Fertility Report now. In 3 simple steps, it will show you a list of clinics that fit your preferences and meet our strict quality criteria. Moreover, you will receive a report via email with useful tips to visit a fertility clinic for the first time.
Hormone analysis
If the seminogram comes back with abnormal results, your doctor may order a hormonal analysis by means of blood work. This study helps the specialist to determine what is causing the results of the semen analysis to be outside the normal range.
Sperm production occurs in the testis thanks to the action of the male sex hormones, including testosterone, FSH (follicle-stimulating hormone), LH (luteinizing hormone), and prolactin.
As such, alterations in the levels of these hormones can affect the sperm production process (spermatogenesis), and therefore the sperm count and quality.
Additional fertility tests for males
When an abnormal result is obtained in the seminogram or there is an alteration in the parameters of concentration, motility, or morphology of the sperm, complementary tests are usually requested to confirm the cause.
Below are details of each of these additional tests that are performed on the man.
Sperm DNA fragmentation test
For the sperms to be able to fertilize the egg properly and give rise to a healthy embryo, capable of attaching to the uterus, it is important for sperm DNA not to be fragmented.
A high degree of sperm DNA fragmentation can translate into fertilization problems, as well as early embryonic development failure.
In recent years, the percentage of men with high levels of sperm DNA fragmentation has increased. The most common causes are exposure to contaminants, pharmacological therapies, smoking or high testicular temperature.
For this reason, those men who present a percentage of sperm fragmentation above 30% should resort to assisted reproduction techniques to achieve a pregnancy.
Semen culture
If the semen analysis reveals the presence of more than 1 million leukocytes/ml, a semen culture is required. Basically, it is a bacteriological study of the sperm to detect microorganisms.
A semen culture may be needed also if the man has testicular pain or swelling, blood in the semen, or a change in the color or smell of the semen is detected.
If the result of the semen culture is negative, which occurs more often than not, it means that there is no infection. In contrast, if the quantity of microorganisms is greater than the normal values, infection is present.
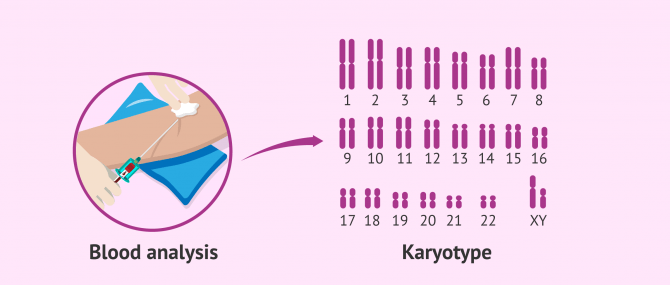
Genetic test - the karyotype study
The karyotype is the set of chromosomes that has every cell of an individual. Specifically, in the human being, there are 23 pairs of chromosomes and one of them corresponds to the sex chromosomes (XX for the female and XY for the male).
Therefore, the karyotype study consists of analyzing the chromosomes to see if there is any alteration, both numerically and structurally, that could be the cause of infertility. This study is carried out by means of a blood analysis.
The karyotype is a very important diagnostic test and is routinely performed in cases of both male and female infertility. If the parents have a genetic or chromosomal abnormality, it is very possible that this is the cause of their problem in trying to conceive.
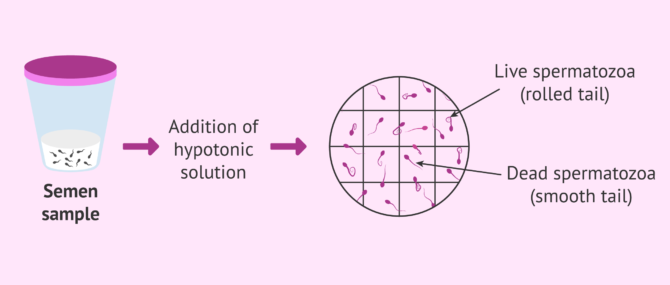
Hypo-osmotic swelling test (HOS)
This test is used to check if the sperm plasma membrane works properly or is damaged. To this end, the sperms are exposed to a hypotonic solution (low in salts), causing an osmotic imbalance in the cells. This imbalance would cause the solution to enter the sperm, increasing its cell volume and the sperm cell becomes swollen.
If the sperm plasma membrane is neither intact nor functional, fertilization cannot occur, hence the importance of the HOS test.
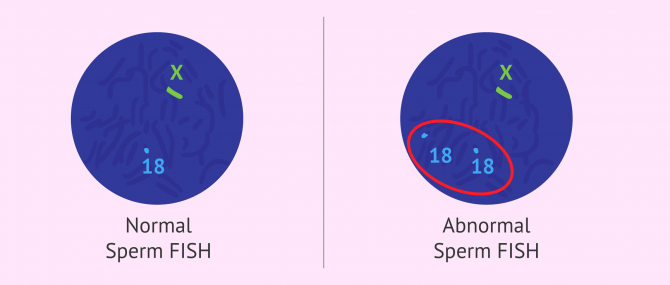
Sperm FISH
Fluorescent in situ hybridization or FISH of sperm is a cytogenetic analysis test in which specific chromosomes of the sperm are marked with fluorescent DNA probes. The purpose is to check if the spermatozoa have a normal chromosome make-up. Therefore, the spermatozoon FISH provides great information about the male's seminal quality.
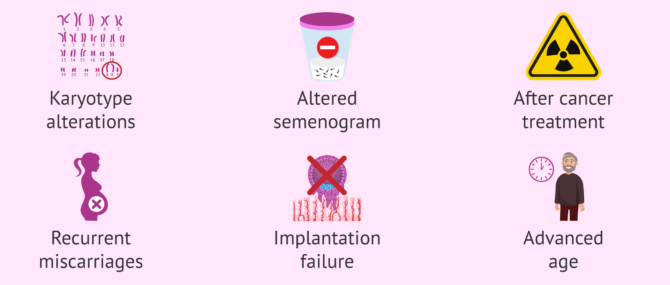
Some situations in which sperm FISH is advisable are the following:
- Genetic disorders.
- Abnormal semen analysis results, especially in cases with low concentration or serious morphology problems.
- Men undergoing chemotherapy or radiotherapy.
- Couples with unexplained recurrent pregnancy loss.
- Repeated implantation failure after applying assisted reproduction techniques.
- Couples who have had a child with a chromosomal disorder.
- Advanced age.
Usually, the chromosomes that are usually analyzed are chromosomes 13, 18, 21, X, and Y. This is known as the 5-probe FISH. However, this study can be performed on other chromosomes.
In general, an abnormal FISH result is considered when, after analysis of between 100 and 2000 spermatozoa, an increased incidence of chromosomal disorders is observed compared to a control group of fertile sperm donors.
You can get more detailed information about this complementary male fertility study in the following article: Fluorescent in situ hybridisation.
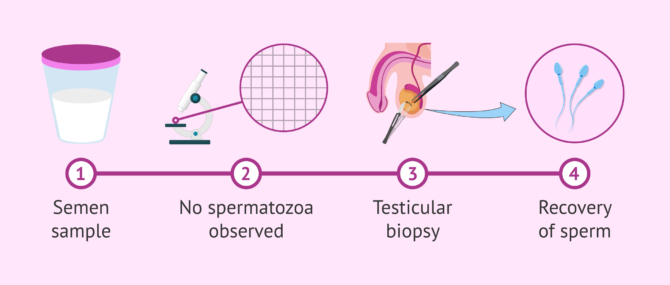
Testicular biopsy
A testicular biopsy is a surgical intervention whereby small samples of the testicular tissue are removed to check whether sperm production is taking place. It is done when the sperm is absent in the semen sample, a condition known as azoospermia.
Normally, this technique does not cause complications in the male. However, as in any surgical procedure, wound infection or minor discomfort may occur in the area.
If you would like to learn more about this procedure please click the following link: What is a testis or testicular biopsy?
Male fertility testing video
In the following video, Michelle Emblenton, a biochemist at inviTRA, tells us about the different tests for the study of male fertility:
When you visit a clinic your specialists will start by asking a series of questions to build up a medical history and order a series of tests on both the man and the woman to check on the fertility. Specifically, the fertility tests involved in a male fertility study will include a physical examination to check overall health and of the reproductive organs, a semen analysis to check the quality and quantity of the sperm and hormonal tests to check the levels of the male sex hormones.
FAQs from users
What is the male factor study?
The male factor as a possible cause of sterility will be studied mainly by performing a semen analysis. This test consists of analyzing a semen sample to evaluate different parameters and thus find out if there is any alteration that may explain or be the cause of sterility. Basically, the pH, volume, concentration and total number of spermatozoa in the sample are evaluated, as well as their motility and morphology. For assisted reproductive techniques, ideally we will also request an EMR (motile sperm count) to know how many motile sperm are actually recovered after processing the sample.
If the semen analysis is altered, it is recommended to repeat it after at least one month to verify that the alterations are still present and have not appeared only occasionally. There are cases in which, if the alterations are important, it will be necessary to complement the study with more tests such as a semen and urine culture to rule out infection; a sperm fragmentation; a genetic study in case this could be the cause of the male factor, etc.
Can I suffer fertility problems because of my advanced age or does it only affect women?
Although in the male there is never a cessation of gamete production, numerous studies have shown that there is a decrease in sperm quality directly related to the age of the male, although it is not as drastic as it would be in the female case.
Between 40 and 70 years of age, a gradual process of decrease in testosterone production begins, which finally affects sperm quality, understood as a decrease in the volume, motility and morphology of spermatozoa, together with damage to sperm DNA.
How can you tell if I am fertile?
If a man has been having unprotected sexual intercourse for a year and has not achieved pregnancy, or if he wants to know if he is fertile, a male fertility study can be performed.
The first thing to do is to take a medical history and a complete physical examination, together with a seminogram, a test that detects the volume, concentration, motility, viability and morphology of the spermatozoa, and which also helps us to prevent, avoid or cure disorders that cause sterility and that usually go unnoticed.
What is the cost of fertility tests for males?
The cost of male fertility tests can range from $50-300, although it depends on the clinic chosen. As for blood tests, the price can range from $200-400. In case you require additional tests, an increase of the overall cost should be expected.
Can a male fertility test be performed even if I am not looking for a child at the moment?
Yes, in fact, it is advisable that all people who wish to have children at some point in their lives, whether they are men or women, carry out a fertility study to verify whether all the necessary factors are present for a pregnancy to occur and to be able to carry to term.
The male fertility study is carried out by means of a semen analysis. This is a test in which the spermatozoa are analysed through the analysis of a semen sample obtained by masturbation. Among the aspects studied are: the degree of male fertility based on the volume, appearance and PH of the semen and the number, morphology and mobility of the spermatozoa. It is important that this semen sample is obtained under optimal conditions and is evaluated by specialists in andrology.
Read more
How can you tell if a man is infertile without medical tests? Are there any home fertility tests or tests sold in pharmacies?
Although sperm count plays a major role when determining a man's fertility, there are at-home kits that allow a man to evaluate his sperm count without involving a professional. Some kits contain a microscope that allows couples to examine the count of sperm. Even though this option can be somewhat helpful, we do not recommend this method to evaluate your infertility.
Read more
What does healthy sperm look and smell like?
Semen color, texture and even smell can provide us with a lot of information about your fertility and health. After ejaculation, we can observe the semen's color, texture, consistency, and smell, and get information on our fertility to some extent.
The color of healthy sperm is normally white or light gray. If it ranges from yellow to even green, you may have a prostate infection and should speak to your medical provider as soon as possible to determine if there is an infection causing your sperm to be non-fertile. In this case, antibiotics may be required.
Yellow can also indicate the presence of urine in the semen. If the color of your semen is pink or reddish-brown, it may be an indication of an inflammation of your prostate and that color is caused by bleeding.
As for the texture/consistency, semen is normally thick after ejaculation. If it changes into a sticky texture, it is likely that a medical condition is present.
Where can a man go to check his fertility?
To a fertility clinic or a hospital with an assisted reproduction unit. They should be carried out by a urologist/andrologist that is experienced in the field of infertility.
What male fertility test should be done before marriage?
There are no compulsory pre-marital male or female fertility test that must be done by default.
However, some couples choose to be tested for HIV and other sexually transmitted diseases, blood group, fertility, possible genetic and/or chronic medical conditions, etc. However such tests are totally optional and at the couples discretion.
Recommended reading
If you want to learn more about the possible causes of male infertility, we recommend you continue reading with the following article: What are the causes of male infertility?
A basic test for the study of maculine fertility is the hormonal analysis. If you wish to obtain more information on this subject, you can visit the following link: Male hormones and fertility.
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
Andrade-Rocha FT (2003). Semen analysis in laboratory practice: an overview of routine test. J Clin Lab Anal 2003; 17: 247-258 (View)
Baker DJ (2007). Semen analysis. Clin Lab Sci; 20: 172-187; quiz 188-192 (View)
Cardona-Toro LE (1996). Espermograma: indicaciones e interpretación. Medicina & Laboratorio; 6: 267-275 (View)
G.R. Dohle, T. Diemer, A. Giwercman, A. Jungwirth, Z. Kopa, C. Krausz (2010). Guía clínica sobre la infertilidad masculina. European Association of Urology 2010 (actualización en abril de 2010) (View)
Guzick DS, Overstreet JW, Factor-Litvak P, Brazil CK, Nakajima ST, Coutifaris C, et al. (2001). Sperm morphology, motility, and concentration in fertile and infertile men. N Engl J Med; 345: 1388-1393 (View)
Kvist U, Björndahl L. ESHRE Monographs: Manual on Basic Semen Analysis. Oxford: Oxford University Press, 2002 (View)
Male infertility best practice policy committee of the American Urological Association (AUA) (2010). The optimal evaluation of the infertile male. AUA Best Practice Statement (View)
Weidner W, Colpi GM, Hargreave TB, Papp GK, Pomerol JM, Ghosh C; EAU Working Group on Male Infertility (2002). EAU guidelines on male infertility. Eur Urol;42:313-22 (View)
FAQs from users: 'What is the male factor study?', 'Which values are considered normal in a semen analysis report?', 'Can I suffer fertility problems because of my advanced age or does it only affect women?', 'How do men get tested for infertility?', 'How can you tell if I am fertile?', 'What physical examinations can a man have to assess fertility?', 'What is the cost of fertility tests for males?', 'How can a semen analysis indicate male infertility problems?', 'Can a male fertility test be performed even if I am not looking for a child at the moment?', 'How can you tell if a man is infertile without medical tests? Are there any home fertility tests or tests sold in pharmacies?', 'How can I know my sperm count?', 'What hormones are studied in male fertility testing?', 'What does healthy sperm look and smell like?', 'Where can a man go to check his fertility?', 'What is a sperm DNA fragmentation test?', 'What can cause a man to be infertile?', 'Why would a semen culture be performed?', 'What male fertility test should be done before marriage?', 'What is a fertility karyotype study?', 'What is a hypoosmotic swelling test?', 'Why would I need a testicular biopsy?' and 'What is the most important part of male fertility testing?'.
Authors and contributors


More information about Michelle Lorraine Embleton











Hello I’ve been trying to conceive for now 8 months and want to know when it’s time so see a fertility specialist?
Thx
Hi,
normally we speak of fertility problems when you have been trying to get pregnant for more than one year and that’s when you should see a fertility doctor.
Women 35 or older should see a fertility specialist after already 6 months.
Hope I have been able to help,
best regards
I got my semen analysis results and it said Oligospermia. What does this mean? Does this mean I can’t impregnate my wife?
Good morning Andrew,
Oligospermia is a sperm disorder that leads to male infertility. It affects the sperm count which appears diminished in a semen analysis report. It can be classified as mild, moderate, and severe which depends on the sperm count, that is, the number of sperms present in the ejaculate.
Depending on the severeness of oligospermia, you can either undergo intrauterine insemination, a simple and cost-effective technique that usually offers good outcomes. Should IUI be ineffective or in cases you have been diagnosed with moderate or severe oligospermia, the treatment of choice would be in vitro fertilization (IVF), either the classical type or IVF/ICSI.
In order to read more about oligospermia and how to get pregnant, have a look at the following post: What Is Oligospermia? – Low Sperm Count Causes & Treatment.
Hope this helps,
Happy holidays.