Male sex hormones play a major role in fertility, since they are directly associated with the sperm production process, which is called spermatogenesis. The most important hormones involved in this function are testosterone, dihydrotestosterone, LH, and FSH.
Hormone analysis in men is carried out through a blood test. If the results obtained show altered values of some of these hormones, it could the reason for the difficulty experienced in becoming a father.
Provided below is an index with the 7 points we are going to expand on in this article.
- 1.
- 2.
- 2.1.
- 2.2.
- 2.3.
- 3.
- 3.1.
- 3.2.
- 3.3.
- 4.
- 4.1.
- 4.2.
- 4.3.
- 5.
- 6.
- 7.
Male fertility tests
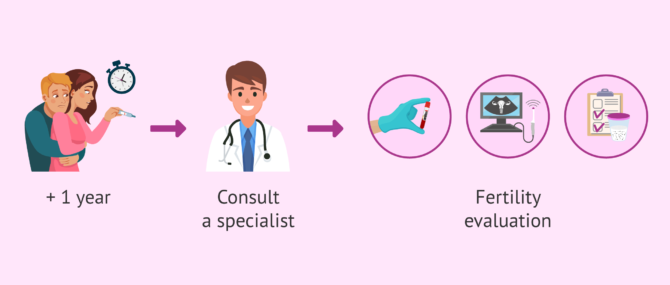
Achieving a pregnancy is not always an easy task. If it has not happened after trying to conceive for a year, couples are strongly recommended to visit a fertility specialist to see if there is some kind of infertility issue that is preventing pregnancy.
Infertility specialists typically ask new patients to undergo a complete fertility evaluation to check fertility in both the man and the woman, since both play a part in the TTC journey, and any abnormality can be the cause of infertility totally or partially.
To check male fertility, the simplest, most informative test is a semen analysis report. It involves examining a semen sample to look for the presence of sperm cells, and see if they are normal in terms of motility, concentration, morphology, etc.
Assisted procreation, as any other medical treatment, requires that you rely on the professionalism of the doctors and staff of the clinic you choose. Obviously, each clinic is different. Get now your Fertility Report, which will select several clinics for you out of the pool of clinics that meet our strict quality criteria. Moreover, it will offer you a comparison between the fees and conditions each clinic offers in order for you to make a well informed choice.
In case that severe abnormalities are found through a semen analysis, such as azoospermia or cryptozoospermia, your doctor may ask you to do a blood test to check your hormone levels and try to find the cause of the poor sperm quality. Sometimes, sperm quality can be improveds with a hormone treatment.
According to Valeria Sotelo, MD:
The first fertility test done in males is a semen analysis. It is used to evaluate the sperm count, motility, and morphology. If the first semen analysis is normal, no other tests are required. But, if the results are abnormal, the man has to repeat it after 15 days.
Function of male sex hormones
Regulation of male sex hormones starts in the hypothalamus, a crucial part of the brain. Its function is to trigger the release of GnRH hormone, responsible for stimulating the pituitary gland to produce FSH and LH.
FSH and LH
The functions of both FSH and LH are interrelated between each other, since both affect the testicular function of males.
On the one hand, FSH regulates spermatogenesis (formation of new spermatozoa) in the seminiferous tubules of the testis. It affects the Sertoli cells, which are responsible for protecting and nourishing the cells that lead to sperm formation (spermatogonia). Moreover, FSH promotes the production of the testicular proteins that bind androgens (ABP).
Testosterone and dihydrotestosterone
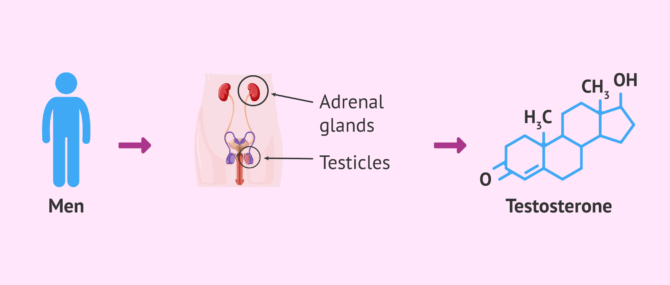
Testosterone is the main male sex hormone. It is produced in the testicles due to the action of LH. It is also produced by the adrenal glands in both men and women, as well as by the ovaries in women, although in a small quantities.
5α-dihydrotestosterone (5α-DHT) derives from testosterone, that is, it is generated out of testosterone thanks to the action of 5α-reductases enzymes.
Both hormones are involved in the development of male sex characteristics, including body mass building, as well as facial and body hair growth.
If you would like to continue reading about this male sex hormone then please take a look at this the following article: What is the function of testosterone?
Prolactin
As it happens with FSH and LH, prolactin is also produced by the pituitary gland, and is involved in male fertility to a large extent.
Prolactin is necessary for the well functioning of the male reproductive system, and affects the Leydig cells and testosterone production directly. As such, if the male has high levels of prolactin, the testosterone levels will be affected.
Male hormone reference ranges
Abnormal variations in the levels of the above mentioned hormones can affect spermatogenesis, either directly or indirectly. The following are the main hormones checked in males to find potential abnormalities:
Testosterone and dihydrotestosterone
Within the organism, testosterone can be free or linked to proteins. These are the normal testosterone levels in adult males:
- Free testosterone (bioavailable, not bound to proteins): 90-300 pg/mg.
- Total testosterone (free + bound to proteins): 270-1070 ng dl.
If the levels of testosterone are low, it can indicate there exists some sort of abnormality that is affecting sperm production, like damage to the testes. This can cause male infertility.
Certain syndrome can cause low testosterone levels, including Klinefelter syndrome or Kallmann syndrome.
If testosterone levels are high, it could be due to a testicular tumor or androgen resistance amongst other potential causes. Certain substances or drugs can also increase testosterone levels.
Finally, normal levels of 5α-DHT are 30-85 ng/dl. Insufficient levels of 5α-reductases enzymes can prevent the synthesis of 5α-DH, causing pseudohermaphroditism (a person that has the secondary sex characteristics of a female but is a man from the genetic viewpoint).
FSH and LH
If your doctor suspects that your male sexual characteristics are abnormal, or you have erectile dysfunction, low libido or infertility issues, he may request a blood test to examine your FSH and LH levels. The reference rangess are:
- FSH: 1.0-12.0 mIU/ml.
- LH: 2.0-12.0 mIU/ml.
Elevated levels of FSH and/or LH may indicate primary testicular failure (PTF), which can be the result of a wide range of indirect causes such as infection, trauma, chemotherapy etc.
Conversely, levels are too low indicate hypothalamic dysfunction or abnormalities in the pituitary gland.
Prolactin
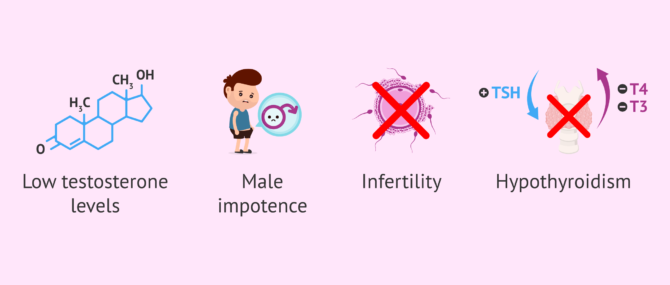
Normal prolactin levels should be between 2.5 and 17 ng/ml (53-360 mIU/l). If they are above this reference range, it can indicate any of the following abnormalities:
- Low testosterone levels
- Sexual dysfunction
- Gynecomastia (abnormal growth of mammary glands)
- Infertility
- Hypothyroidism
- Pituitary tumor
Prolactin can also be analyzed for clinical follow-up of men who have low testosterone concentrations.
FAQs from users
My hormone levels are normal but I have azoospermia. Is it normal?
It can be that the hormonal values are normal, but that there is some other problem affecting sperm production or the exit of the spermatozoa to the exterior.
In the latter case, this alteration is called obstructive azoospermia and, sometimes, sperm can be obtained by means of a testicular biopsy.
However, it should be borne in mind that it is not always possible to find the cause of sterility in both males and females.
What treatment options do I have for abnormal testosterone levels?
Artificial testosterone can be administered through different routes:
- Intramuscular injection: there exist different types of synthetic testosterone that can be administered intramuscularly. Propionate remains for a reduced time period in the body, so it has to be administered every 2-3 days. Testosterone enanthate and cypionate can be injected every two weeks (dose of 200 mg). Conversely, testosterone undecanoate can be administered every 12-15 weeks (1000 mg).
- Transfermal (patch): it can be administered in the form of a gel or cream daily, in the form of patches or implant.
- Oral (pills): this is the least common of all routes, since it is detrimental for the liver (hepatic toxicity).
Even though artificial testosterone can have many benefits, like muscle development or secondary male characteristics, one should keep in mind that, as with any other medication, it can have some side effects. Always follow your doctor's instructions before taking this type of medication.
What effects do hormones have on male fertility?
Generally, hormonal analysis in men to study their fertility consists of determining the levels of testosterone, FSH (Follicle Stimulating Hormone) and LH (Luteinizing Hormone).
FSH is involved in spermatogenesis, that is, in the formation of spermatozoa in the seminiferous tubules.
On the other hand, LH acts on the Leydig cells and secretes testosterone, the male sex hormone par excellence.
Finally, testosterone is involved in the development of male sexual characteristics. Thus, testosterone is responsible for the growth of muscle mass, beards and body hair.
Recommended reading
In addition to an hormone test, there are other tests a man can undergo to learn more about his fertility. If you are interested in delving deeper into them, we recommend that you have a look at this guide: Male Fertility Testing – How Do You Know if You Are Infertile?
The most common, informative of all male fertility tests is, as we explained above, the semen analysis (SE). We recommend that you get more info on this test here: What Is a Semen Analysis Report? – Purpose, Preparation & Cost.
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
G.R. Dohle, T. Diemer, A. Giwercman, A. Jungwirth, Z. Kopa, C. Krausz (2010). Guía clínica sobre la infertilidad masculina. European Association of Urology 2010 updated Abril 2010)
Griffin JE, Wilson JD (1998). Disorders of the testes and the male reproductive tract. En: Wilson JD, et al. Williams Texbook of Endocrinology, 9th ed. Saunders Company, Philadelphia
Jockenhövel F (2004). Male hypogonadism. Ed.UNI-MED International Medical Publishers. Bremen, Germany.
Juárez de Diego JF (1999). Principales causas de infertilidad masculina. En: Arrondo JL. Actualización en Andrología. Publimed Comunicación SL. Pamplona.
Male infertility best practice policy committee of the American Urological Association (AUA) (2010). The optimal evaluation of the infertile male. AUA Best Practice Statement.
Matorras R, Hernández J (eds.) (2007): Estudio y tratamiento de la pareja estéril: Recomendaciones de la Sociedad Española de Fertilidad, con la colaboración de la Asociación Española para el Estudio de la Biología de la Reproducción, de la Asociación Española de Andrología y de la Sociedad Española de Contracepción. Adalia, Madrid.
Pierik FH, Van Ginneken AM, Dohle GR, Vreeburg JT, Weber RF (2000). The advantages of standardized evaluation of male infertility. Int J Androl; 23(6): 340-6.
Sociedad Española de Fertilidad (SEF) (2011). Manual de Andrología. Coordinador: Mario Brassesco. EdikaMed, S.L. ISBN: 978-84-7877.
Sociedad Española de Fertilidad (SEF) (2011). Recomendaciones para el estudio básico de la infertilidad masculina. En: Andrología (Cap. 43)
Trastornos endocrinos y metabólicos. En: Beers MH, Berkow R. El Manual Meck de diagnóstico y tratamiento, 10. ª ed. Ediciones Harcourt, Madrid 1999. p. 2388-92.
Working, P. K. (1995). Reproductive toxicology. In: Patty's Industrial Hygiene and Toxicology, Third Edition, Vol. 3, Part B, 193-230
World Health Organization (WHO) (2000). WHO Manual for the Standardized Investigation, Diagnosis and management of the infertile male. Cambridge: Cambridge University Press.
Reproducción Asistida ORG. Video: ¿Qué pruebas se realizan en el hombre y en qué consisten? (Male fertility tests and their usefulness), by Valeria Sotelo, MD, Apr 7, 2015. [See original video in Spanish].
FAQs from users: 'My hormone levels are normal but I have azoospermia. Is it normal?', 'What treatment options do I have for abnormal testosterone levels?' and 'What effects do hormones have on male fertility?'.
Authors and contributors


More information about Michelle Lorraine Embleton






My husband’s test results were azoospermia with FSH 29 and FH 9.10. He is 34 years old and they say he has damage that has no solution, is this true?
Hi ZoeCres88
Azoospermia with an FSH value almost 2 times higher than its normal value is an indication of a malfunction of the cells that regulate sperm formation. This points to the existence of a primary testicular failure and makes the possibility of pregnancy quite difficult even through assisted reproductive techniques.
You can consult with a reproductive specialist about the possibility of turning to testicular biopsy or epididymal aspiration, to try to find some viable sperm in the testicle with which to proceed to perform an ICSI. You can read more about these procedures here:
Testicular biopsy and epididymal sperm aspiration.
I hope this information is helpful.
Best regards.
Thanks for the article. My wife and I have been trying for a while now and it just isn’t happening. We are going for fertility testing next week so reading up on all I need to know before hand. Your site is very informative.