The prevalence of the human immunodeficiency virus HIV in people of childbearing age, and the progress of antiretroviral treatments which improve the quality of life of HIV-positive patients, mean that more and more serodiscordant couples wish to have children of their own.
A serodiscordant couple is one in which only one partner is a carrier of the virus. In the case of the male partner, seminal lavage and assisted reproduction can be used to minimize the risk of transmitting the virus to his partner.
Provided below is an index with the 7 points we are going to expand on in this article.
- 1.
- 2.
- 2.1.
- 2.2.
- 3.
- 4.
- 4.1.
- 4.2.
- 4.3.
- 4.4.
- 5.
- 6.
- 7.
What is HIV and how is it transmitted?
The human immunodeficiency virus (HIV) is a retrovirus that is transmitted through blood, sexual fluids, and by vertical transmission (through mothers to children).
It is important not to confuse it with AIDS (Acquired Immune Deficiency Syndrome), which is the most serious manifestation of a series of alterations affecting people infected with HIV because their immune system is strongly affected by the virus.
The fact that it is sexually transmitted makes it advisable to turn to assisted reproduction techniques to minimize the risk of transmission of the virus from one partner to the other in the case of being serodiscordant.
If both partners are HIV-positive, re-infection with different strains can also be harmful, as it can worsen the state of the disease. Therefore, it is also recommended to opt for assisted reproduction if children are desired.
If the man is the carrier of HIV, there is the option of performing a sperm washing to avoid the transmission of the infection to the mother and even to the future baby when trying to get pregnant.
What is sperm washing?
Sperm washing consists of processing the semen sample to eliminate the viral particles of the seminal plasma and the cells that may be HIV carriers. Thus, separating the mobile spermatozoa to be used in an assisted reproduction technique.
Semen is mainly made up of three fractions or parts: seminal plasma, spermatozoa and other cells.
Despite being a controversial issue, the most widely accepted theory today is that sperm do not transmit the retrovirus. Therefore, by washing the sample, the risk of the woman becoming infected is practically zero.
How will sperm washing be done?
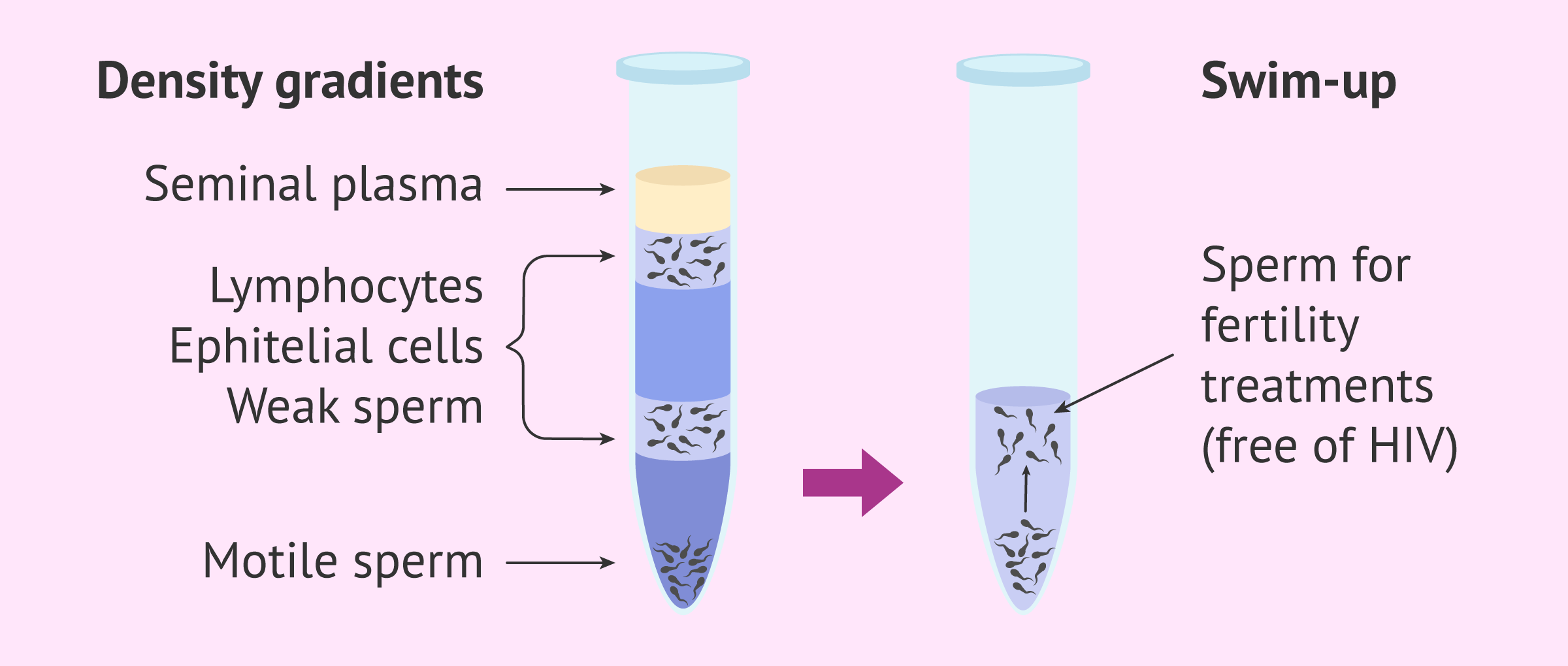
To perform the washing, the patient must leave a semen sample in the andrology laboratory. Using different techniques, sperm with better mobility are separated from the rest of the semen components: seminal plasma, lymphocytes, epithelial cells, weak sperm...
The most common way to separate the best spermatozoa from the rest of the semen sample is to apply a double washing process. Therefore, a density gradient is performed followed by a swim-up.
- Density Gradients
- several layers of different concentrations are added to separate the different cellular fractions of semen. The sample is added to the top. After centrifugation the motile sperm are found at the bottom of the tube.
- Swim-up
- sperm recovered from the density gradients are added to a tube with semen preparation medium and incubated under controlled conditions. The sperm with the best motility will be found at the top of the sample, from where they will be retrieved.
Once the best quality sperms have been isolated, it is important to confirm the absence of the virus in the sample. This must be done before use in artificial insemination or in vitro fertilization (IVF).
Confirmation of the absence of the virus
After performing the seminal lavage, half of the sample obtained is analyzed, usually by PCR, to verify that no viral particles are present. The other half of the sample is then frozen, awaiting the results.
If the test result is negative, i.e. there is no virus, the part of the sample that remains frozen is considered suitable for assisted reproduction treatment. On the contrary, if the presence of virus is confirmed, the frozen sample is discarded. In the latter case, it will be necessary to start the entire seminal lavage procedure with a new semen sample.
However, these samples are usually virus-free in a high percentage of cases. Moreover, it can be said that the guarantee of success is very high. So far, no case of HIV transmission after seminal lavage has been described.
Sperm washing and assisted reproduction tecniques
Once it has been confirmed that the sample is free of viral particles, it can be used to perform the assisted reproduction technique indicated. This could be either artificial insemination or in vitro fertilization (IVF).
However, some specialists prefer not to perform artificial inseminations because the risk of theoretical infection is higher. Furthermore, the initial seminal quality must be very good so that, once processed, it has sufficient concentration to achieve pregnancy with this technique.
For all these reasons, the chosen technique after sperm washing is usually IVF with ICSI (intracytoplasmic sperm injection).
It should also be kept in mind that HIV-positive patients may have the quality of semen affected by the infection itself or by antiretroviral treatments. Therefore, in cases where the initial quality of the seminal sample is not very good, the chosen technique will be IVF-ICSI (intracytoplasmic sperm injection).
Furthermore, if there are other fertility problems in the couple that hinder pregnancy by artificial insemination, IVF-ICSI will also be chosen. For example, if the woman has blocked fallopian tubes or is of advanced age.
Fertility treatments, like any other medical treatment, require that you trust the fertility specialists that will be by your side during your journey. Logically, each clinic has a different work methodology. Our Fertility Report will offer you a selection of recommended clinics, that is, fertility centers that have passed our rigorous selection process. Moreover, our system is capable of comparing the costs and conditions of each one so that you can make a well-informed decision.
FAQs from users
Is seminal washing in men with HIV effective in achieving a pregnancy without risks for the mother and the foetus?
One of the ways of transmission of the human immunodeficiency virus is sexual and, indeed, the seminal sample of an HIV+ male may contain a viral load that allows infection of his partner.
Seminal washing is a laboratory technique that is applied to couples in which the male may be affected by an HIV infection and also by hepatitis B or C virus. It is based on the fact that viruses are located in seminal plasma and non-sperm cells, but not in sperm.
When the spermatozoa are separated from both seminal components, we are sure that the risk of viral transmission has been reduced to the maximum and this is confirmed by the determination of the negative viral load in the treated sample in the laboratory, which shall be used for assisted reproduction.
Which one do you recommend in patients with HIV? IUI or IVF?
When a man is affected by HIV, the first thing we would do is wash the semen sample, which removes the seminal plasma, so that the sample contains spermatozoa only. Thanks to this technique, we are able to remove the virus from semen samples. After the washing, we examine the sample to detect copies of the virus using the PCR (Polymerase Chain Reaction) test. If the PCR is negative or the number of copies is low, the sample can be used for a fertility treatment. In this cases, we recommend patients to choose ICSI, as a sperm washing affects the sperm count and motility.
Does the time it takes to do sperm washing to eliminate HIV affect the quality of the eggs?
No, because it is taken into account when programming the woman's follicular puncture. In addition, the sperm sample is often frozen to ensure that on the day the eggs are obtained, a sample free of viral particles will be available.
Is sperm washing only performed in patients with HIV infection?
No. sperm washing can be performed in HIV serodiscordant couples in which the male partner is the carrier of the virus, but also when the male partner is infected with hepatitis B or C virus.
In any case, the purpose of seminal lavage is to minimize the risk of transmitting the infection to the partner in the search for pregnancy.
Recommended reading
As we have already mentioned, HIV can be transmitted sexually. In the following article we discuss other sexually transmitted diseases in case you need more information: Sexually transmitted diseases - STDs.
In the following article you can find more information about the management of seropositive patients when trying for a baby: Pregnancy with HIV.
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
Bujan L, Hollander L, Coudert M, Gilling-Smith C, Vucetich A, Guibert J, Vernazza P, Ohl J, Weigel M, Englert Y, Semprini AE; CREAThE network. Safety and efficacy of sperm washing in HIV-1-serodiscordant couples where the male is infected: results from the European CREAThE network. AIDS. 2007 Sep 12;21(14):1909-14. (View)
Carvalho WAP, Catafesta E, Rodart IF, Takata S, Estevam DL, Barbosa CP. Prevention of HIV transmission with sperm washing within fertile serodiscordant couples undergoing non-stimulated intrauterine insemination. AIDS Care. 2021 Apr;33(4):478-485. (View)
Eke AC, Oragwu C. Sperm washing to prevent HIV transmission from HIV-infected men but allowing conception in sero-discordant couples. Cochrane Database Syst Rev. 2011 Jan 19;(1):CD008498. (View)
Garrido N, Meseguer M, Remohí J, Simón C, Pellicer A. Semen characteristics in human immunodeficiency virus (HIV)- and hepatitis C (HCV)-seropositive males: predictors of the success of viral removal after sperm washing. Hum Reprod. 2005 Apr;20(4):1028-34. (View)
Kim LU, Johnson MR, Barton S, Nelson MR, Sontag G, Smith JR, Gotch FM, Gilmour JW. Evaluation of sperm washing as a potential method of reducing HIV transmission in HIV-discordant couples wishing to have children. AIDS. 1999 Apr 16;13(6):645-51. (View)
Sauer MV. Sperm washing techniques address the fertility needs of HIV-seropositive men: a clinical review. Reprod Biomed Online. 2005 Jan;10(1):135-40. (View)
Zafer M, Horvath H, Mmeje O, van der Poel S, Semprini AE, Rutherford G, Brown J. Effectiveness of semen washing to prevent human immunodeficiency virus (HIV) transmission and assist pregnancy in HIV-discordant couples: a systematic review and meta-analysis. Fertil Steril. 2016 Mar;105(3):645-655.e2. (View)
FAQs from users: 'Is seminal washing in men with HIV effective in achieving a pregnancy without risks for the mother and the foetus?', 'Which one do you recommend in patients with HIV? IUI or IVF?', 'Does the time it takes to do sperm washing to eliminate HIV affect the quality of the eggs?' and 'Is sperm washing only performed in patients with HIV infection?'.
Authors and contributors

More information about Michelle Lorraine Embleton







My husband he is in such situation: HIV postive with a viral load undetectable cd4 cout 604, while I’m negative. We’re planining to get our own kids without sperm donor. Pls how can we get access to the sperm washing? We live in Nigeria. Thx
Hello Victoria,
Are you planning to travel abroad? This is important before providing you with any advice. Anyway, my advice now is that you complete our form: https://www.invitra.com/en/estimates/ By doing it, you will receive detailed estimates with the approximate cost of sperm donation from various fertility clinics.
I hope this helps,
All the best