Reciprocal in vitro fertilization is also known as partner assisted reproduction, co-IVF, shared motherhood, or ROPA (reception of oocytes from partner), is a popular fertility treatment. It enables women in a lesbian relationship to share the motherhood of the baby.
This practice for LGBT family building, often referred to as partner assisted reproduction, is an in vitro fertilization (IVF) treatment in which one of the women provides the eggs and the other woman will carry out the pregnancy.
Therefore, like other assisted reproduction techniques, the ROPA method only allows one of the two women to provide the genetic material (DNA). However, what differentiates the ROPA method is that the other woman will be in charge of carrying the baby throughout pregnancy.
Availble for both lesbian couples and for transexual men (who have functional female reproductive organs), reciprocal IVF makes it possible for both parents to feel involved in the emotional and physical experiences of trying for a baby.
Provided below is an index with the 10 points we are going to expand on in this article.
- 1.
- 2.
- 2.1.
- 2.2.
- 2.3.
- 2.4.
- 2.5.
- 3.
- 3.1.
- 3.2.
- 4.
- 4.1.
- 4.2.
- 4.3.
- 5.
- 6.
- 7.
- 7.1.
- 7.2.
- 7.3.
- 7.4.
- 7.5.
- 7.6.
- 7.7.
- 8.
- 9.
- 10.
What exactly is reciprocal IVF?
Reciprocal IVF (RIVF) can be defined as a type of in vitro fertilization aimed at same sex, female couples, who do not have fertility issues. The eggs from one partner are inseminated with donor sperm, and the resulting embryo(s) transferred to the other partner, who will carry the pregnancy to term and give birth.
As such, although both women are involved the journey towards becoming lesbian mothers, their paths though it are diffferent.
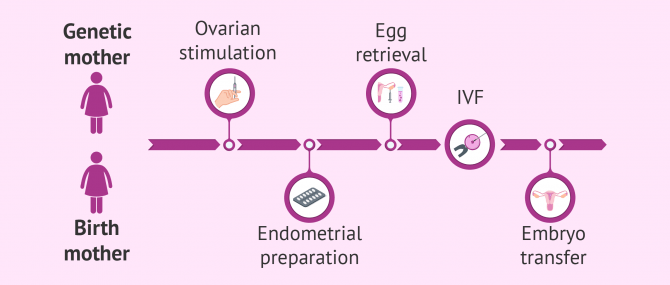
Thus, one of the two women (the egg "donor") will have to undergo controlled ovarian stimulation (COS) and follicular puncture. The other woman (the one who is going to become pregnant) will have to prepare her endometrium to favor implantation and, subsequently, undergo embryo transfer.
Reciprocal IVF step by step
The procedure of the ROPA method is the same as that of egg donation. The difference that the egg donor is not anonymous, since she will be one of the two women of the couple. Therefore, one of the mothers will provide the genes (DNA) to her future child and the other will carry the child.
Ovarian stimulation
The woman who provides the eggs, the genetic mother, receives hormonal medication to stimulate the maturation of mutliple egg. This treatment usually consists of a combination of GnRH analogs and gonadotropins that stimulate the development of multiple ovarian follicles. The objective of this treatment is to increase the probability of success of the reproductive method.
The administration of the hormonal drugs is done by the patient herself. Usually this is by subcutaneous injections in the abdominal area, following a detailed explanation from the specialist.
Throughout the period of ovarian stimulation (10-12 days), the woman should visit the doctor periodically. Both blood tests and ultrasounds are required for the specialist to monitor the follicular growth and schedule the best time to obtain the eggs.
If you would like to know more about this procedure, we recommend reading the following article:Ovarian stimulation protocols in IVF.
Follicular puncture
Once the ovarian follicles have reached the appropriate size (approximately 16-18 mm), the patient should be administered another hormonal drug to promote the final maturation of the eggs and trigger ovulation.
However, in order to perform the ROPA method, the eggs must be removed from the ovary before ovulation occurs. This is done through a simple surgical procedure called follicular puncture or ovum pick-up.
The ovarian puncture procedure lasts about 20-30 minutes and is performed under mild anesthesia. The process consists of the aspiration of the follicular fluid where the eggs are located. A needle is inserted vaginally under ultrasound guidance.
You can read more about this surgical intervention in the following article: Ovarian puncture.
Fertilization and embryo culture
In lesbian, reciprocal IVF, the mature eggs obtained after follicular puncture are fertilized with sperm from a donor. The identity of the sperm donor depends on the law of the country where you live.
For example, in the United States you may be able to select the donor from a "brochure" or chose a friend or family member. In most European counties, sperm donation is an anonymous and altruistic act. Therefore the donor will be selected for you by the clinic, from an anonymous donor.
Fertilization can be performed by conventional IVF or by ICSI (intracytoplasmic sperm injection). The choice of one method or another for fertilization will depend on the characteristics of each patient, age, the quality of the eggs, etc.
Following this stpe, eggs that have been correctly fertilized (already considered embryos) are selected and left in culture for 3 to 6 days. During this time, the laboratory monitors the growth of the embryos to ensure they develop correctly.
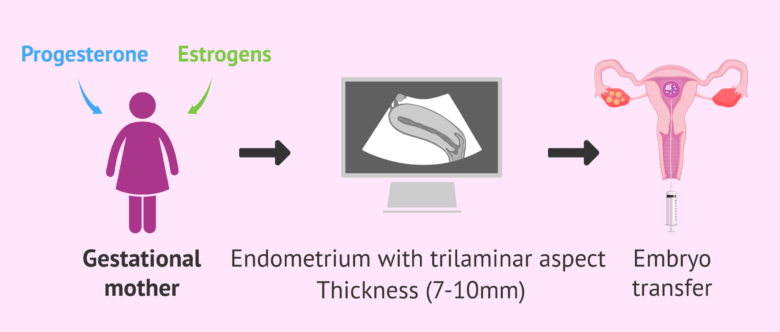
Endometrial preparation and embryo transfer
The woman who is going to carry the pregnancy to term, the gestational mother, receives a different hormonal treatment to her partner. The gestational mother will take estrogens and progesterone vaginally, orally, or in patches. This treatment favors the growth of the endometrium and allows it to acquire the correct aspect and thickness for embryo implantation.
Specifically, the embryo transfer will be scheduled when the endometrium of the gestational mother is 7-9 mm thick and has a trilateral aspect. However, these endometrial characteristics do not guarantee 100% that the embryos will implant, since other factors also play a part.
Embryo transfer consists of placing the highest quality embryo(s) into the uterine cavity. This is a painless and quick process that does not require anesthesia or special care.
Finally, it should be clarified that the current tendency is to transfer a single embryo, although in certain cases two embryos are transferred.
According to guidelines of the American Society for Reproductive Medicine (ASRM), it is recommended not to transfer more than three embryos due to the risk of multiple pregnancy. In many European countries such as the UK and Spain, the transfer of a maximum of three embryos is regulated by law.
For this reason, the viable embryos that are not transferred initially will be cryopreserved for a new attempt (if the first one has failed) or in case the couple wants to try for more children in the future.
Pregnancy testing
About 10-12 days after the embryo transfer, the gestational mothern will have a beta-hCG test done to confirm if she is pregnant. This period is known as two-week wait or the beta wait. It can be very emotionally challenging. However, specialists advise continuing with the daily routine (without over straining or stress) and trying not to think about whether fertility treatment has been successful or not.
We advise not performing the pregnancy test before the date indicated, as this could lead to an erroneous and unreliable result.
Medical requirements for each mother for ROPA IVF
As mentioned earlier, reciprocal IVF is a type of IVF tailored exclusively for lesbian couples who want to have a child. The decision on the role assigned to each mother-to-be is up to them although you should take the advice of your doctor in consideration.
Genetic mother
Usually, it is recommended that the youngest woman provides the eggs, since the quality of the eggs decreases with age (especially after 35 years of age). It is also essential that this woman has a good ovarian reserve.
Furthermore, it is recommended that the egg donor undergo genetic analysis such as karyotyping.
By taking these requirements into account, it is possible to obtain a greater number of embryos of better quality. In this way, the probability of pregnancy in the gestational mother will be increased.
Gestational mother
For her part, the woman who will carry the pregnancy in reciprocal IVF should have a normal, healthy uterus, without alterations that could hinder gestation and embryonic development.
It is also advisable that the gestational mother does not have any dieases that could impair her ability to carry the pregancy to completion. For example, thrombophilias or autoimmune diseases. In such cases, the success of the treatment could be compromised.
Legal considerations
As with all assisted reproductive techniques, the legal aspects of the treatment need to be considered first. With reciprocal IVF, the genetic mother is technically an egg donor, and in some countries egg donation is strictly anonymous.
Below we take a brief look at the situation in a the US, UK and in Spain. However this information is for guidance only and we recommend investigating the laws in your country of treatment thoroughly before starting any treatment.
Reciprocal IVF in the United States of America
In the US, the legal issues vary from state to state. As the law allows for you to choose your egg and/or sperm donor the problems may arise when applying for parental rights and parentage. It may be useful to consult professional legal advice.
UK guidelines for RIVF
In June 2021, the UK governing bosdy the HFEA, introduced consent so that a woman may donate her eggs to her partner if in a same sex relationship, without needing to be registered as a donor. The appropriate consent form, the WPT, must be signed.
The legality of who the parents are on the birth certificate must also be considered, as the gestational mother will be the named parent. Being married or having a civil partnership greatly helps the process.
The ROPA method in Spain
In order to carry out the ROPA method, a fundamental requirement exists: marriage. It is not sufficient to be a common-law partner to initiate a ROPA method.
If the women are not married, the ROPA method would be considered an open egg donation, something totally forbidden in Spain, since gamete donation must be anonymous.
How much does reciprocal IVF cost?
The costs of co-IVF are similar to those associated with conventional IVF.
For more detail about how much it costs in the USA we have an article dedicated to the question: Cost of IVF in the USA. In summary, you can expect to pay between $10,000 - $15,000 depending on the clinic and individual treatment.
In the UK the price is around £5,000 per cycle and in Canada starts from approximately $7,000 CAD. You can find more information concerning these countries in this article: In vitro fertilization.
In Spain The ROPA method has an approximate cost of between €3,500 and €6,000. In addition, hormonal medication for ovarian stimulation and endometrial preparation is not usually included in the initial price of the treatment.
Are you interested in undergoing Reciprocal IVF to become mothers? Then we recommend that you get your Fertility Report now. It will provide you with a selection of clinics that have passed our rigorous selection process, and subsequently we consider top clinics for our readers. We will send you a report with information on the fees and conditions of each clinic for this particular treatment option.
Video about reciprocal IVF
Michelle, biochemist at inviTRA, tells us in this video about all the aspects related to the ROPA method or reciprocal IVF:
Co-IVF or reciprocal IVF is an in vitro fertilization treatment aimed at same-sex female couples. In this treatment, one of the women is chosen to be the genetic mother and will provide the genetic load of the baby in the form of her egg cells.
FAQs from users
Can leftover embryos from reciprocal IVF be transferred to the woman who donated her eggs?
Of course. The embryos belong to both women. If they wish so, the embryos can be transferred to either of the couple.
In treatments using the ROPA method, is the sperm donor chosen according to the physical characteristics of the genetic mother or the pregnant woman?
In the semen request, the characteristics of both women are collected. Normally, the sperm is chosen according to the woman who is going to gestate the pregnancy because the other member of the couple already provides her genetic material in the oocyte she gives to her partner.
How does reciprocal or co-IVF work?
Reciprocal or co-IVF is a type of IVF with ICSI that has been created exclusively for lesbian couples with a desire to start a family. Moreover, both of them can participate actively in the pregnancy—one contributes the egg, while the others carries the baby until birth.
In particular, the treatment is made up of two parts, each woman participating in one:
- Woman who contributes the genetic material
- She undergoes IVF ovarian stimulation and goes through follicular puncture (egg retrieval).
- Woman who bears the pregnancy
- She receives the resulting embryos after fertilization in the lab using donor sperm, and carries the baby until birth.
Both women have to take hormonal medications: woman A for ovarian stimulation, and woman B for endometrial preparation.
Is reciprocal IVF covered by insurance?
No, it isn't. Unfortunately, insurance providers don't cover IVF when one partner carriers the pregnancy and the other provides eggs unless it is required for medical reasons. However, diagnostic testing and doctor visits for the pregnant woman may be covered. Our advice is that you verify it with your provider, as coverage varies by provider.
The UK NHS does not currently cover reciprocal IVF treatments.
What is the difference between the ROPA method and donor IUI?
The fundamental difference between these two assisted reproduction techniques lies in the participation of the pregnancy. In the case of the ROPA method, both women participate in the process. One woman of the couple provides the eggs that will be fertilized with the donor sperm, while the other woman will be in charge of carrying the pregnancy to term.
In contrast, in artificial insemination with donor sperm (Donor IUI) only one woman participates, who is administered hormonal medication to stimulate the ovary and produce 1-2 follicles.
Reciprocal IVF vs. donor insemination, what's better?
It is not a matter of choosing one over the other, but about considering the pros and cons of each option. Usually, women in a lesbian relationship are recommended to start with IUI and after 3-6 failed cycles, they are recommended to move to IVF, as higher success rates are expected to be reached.
However, a couple may wish to undergo this process in order for both women to participate in the pregnancy actively. It is their choice.
Is IVF for lesbian couples available on the NHS?
According to the National Institute for Health and Clinical Excellence (NICE) guidelines, NHS-funded IVF should be offered up to the age of 42 in certain circumstances, though the IVF age limit is 39. It states that same-sex couples should be offered NHS-funded fertility treatment.
Intrauterine insemination is offered to lesbian couples and, after 6 unsuccessful cycles of IUI, they should move to IVF. This applies to heterosexual couples having difficulty conceiving as well.
Recommended reading
Lesbian couples can also use other assisted reproduction techniques to become mothers. In this article we discuss the different options: Baby options for lesbian couples
If you are interested in finding out about IUI with donor sperm, we recommend reading this page: IUI with donor sperm.
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
Ballesteros A, Castilla JA, Nadal J, Ruiz, M. Manifiesto de la SEF sobre la donación de gametos en España. Publicado a través de la Sociedad Española de Fertilidad (SEF).
Comisión Nacional de Reproducción Humana Asistida (CNRHA) (2015). Aspectos legales y éticos de la donación. En: Registro Nacional de Donantes de Gametos y Preembriones. Ministerio de Sanidad, Consumo y Bienestar Social de España.
Grupo de trabajo conjunto de la Sociedad Española de Fertilidad (SEF) y la Asociación para el Estudio de la Biología de la Reproducción (ASEBIR). Recomendaciones para la aplicación del RD 1301/2006- Diciembre 2012.
Ley 14/2006, de 26 de mayo, sobre técnicas de reproducción humana asistida. Jefatura del Estado «BOE» núm. 126, de 27 de mayo de 2006 Referencia: BOE-A-2006-9292
Marina S, Marina D, Marina F, Fosas N, Galiana N, Jové I. Sharing motherhood: biological lesbian co-mothers, a new IVF indication. Human Reprod. 2010; 25(4): 938-41.
Pennings G. Having a child together in lesbian families: combining gestation and genetics. J Med Ethics. 2016; 42(4): 253-5.
Saus-Ortega C. La maternidad biológica compartida en parejas lesbianas. La técnica de fertilización «in vitro» con el método de recepción de ovocitos de la pareja (ROPA): revisión de la literatura. Matronas Prof. 2018; 19(2): 64-70.
Sociedad Española de Fertilidad (SEF) (2011). Manual de Andrología. Coordinador: Mario Brassesco. EdikaMed, S.L. ISBN: 978-84-7877.
Vitule C, Couto MT, Machin R. Same-sex couples and parenthood: a look at the use of reproductive technologies. Interface-Comunicação, Saúde, Educação. 2015; 19(55): 1.169-80.
Yeshua A, Lee JA, Witkin G, Copperman AB. Female couples undergoing IVF with partner eggs (co-IVF): pathways to parenthood. LGBT Health. 2015; 2(2): 135-9.
Zeiler K, Malmquist A. Lesbian shared biological motherhood: the ethics of IVF with reception of oocytes from partner. Medicine, Health Care and Philosophy. 2014; 17(3): 347-55.
FAQs from users: 'Can leftover embryos from reciprocal IVF be transferred to the woman who donated her eggs?', 'In treatments using the ROPA method, is the sperm donor chosen according to the physical characteristics of the genetic mother or the pregnant woman?', 'How does reciprocal or co-IVF work?', 'What is co-IVF?', 'Is reciprocal IVF covered by insurance?', 'What are the steps of reciprocal IVF?', 'What is the difference between the ROPA method and donor IUI?', 'What medical requirements are there for co-IVF?', 'Reciprocal IVF vs. donor insemination, what's better?', 'Is IVF for lesbian couples available on the NHS?', 'What legal considerations are there for co-IVF?', 'How much does reciprocal IVF cost?', 'Can leftover embryos from co-IVF be transferred to either woman?' and 'How is the sperm donor chosen for co-IVF?'.
Authors and contributors

More information about Michelle Lorraine Embleton











Hi, we have just had the embryo transfer and are currently in the dreaded 2WW. Anyone got any tips to help us through?
Hi ClaireandShayla
I sympathise with the stress of the wait and wish all the best for a positive outcome. In the meantime you can have a look at our tips and information in the following article: The two week wait
I hope this helps!
Hi
My wife Caitlynn and I had our baby girl in June last year. It took us two attempts but we are over the moon with baby Catherine . I was the pregnant one and it was an amazing feeling to know I was carrying Caitlynns child. We opted to use my brother as the sperm donor to make our babies more like us! Good luck to anyone trying and lots of baby dust!
Hey darlings, my wife and I are ttc and are pretty sure we want to give RIVF a try! We’ve been saving for a year and well we think we may be ready for now (may, not sure). Any advice or experiences????