A woman's ovarian reserve, egg reserve, is an indicator of her egg count at a particular stage of her life. In other words, it is an indicator of female fertility.
The higher the egg count, the greater the chances of getting pregnant. If the egg count is poor, IVF may need needed to have a baby.
It is also possible to have a large number of eggs available, but they are not of good quality. In this case, acheiving pregnancy naturally with her own eggs can be complicated.
Provided below is an index with the 9 points we are going to expand on in this article.
- 1.
- 2.
- 2.1.
- 3.
- 3.1.
- 3.2.
- 3.3.
- 3.4.
- 3.5.
- 4.
- 5.
- 6.
- 6.1.
- 6.2.
- 6.3.
- 6.4.
- 6.5.
- 6.6.
- 6.7.
- 6.8.
- 7.
- 8.
- 9.
What does 'egg reserve' mean?
Women are born with all the eggs that they will have during their lifetime. On average, their supply of eggs at birth is around 1 million oocytes. At puberty, this amount is reduced to 400,000-500,000. After the first menstrual period, women release an egg every month. It is estimated that only 400-500 will be ovulated during a woman's reproductive years. The rest will degenerate along the way.
The definition of ovarian reserve is the amount of eggs a woman has at her disposal at a specific time and will be decisive in achieving pregnancy, both naturally and through assisted reproduction techniques.
If you need to undergo IVF to become a mother, we recommend that you generate your Fertility Report now. In 3 simple steps, it will show you a list of clinics that fit your preferences and meet our strict quality criteria. Moreover, you will receive a report via email with useful tips to visit a fertility clinic for the first time.
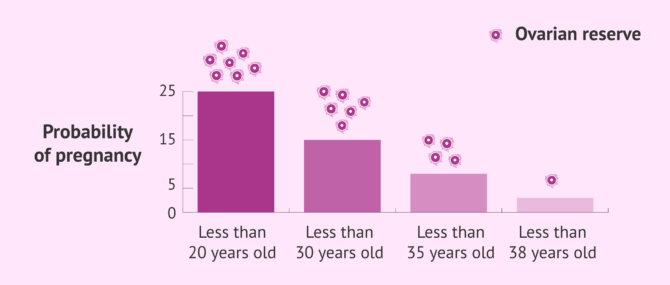
The most fertile period in a woman's life is from ages 16 to 30. At this point, both her egg supply and quality should be excellent. The egg reserve goes through a major decrease from age 35-37.
At age 40, the ovarian reserve is considerably low, and will keep on diminishing until its complete depletion approximately at ages 45-55. This period marks the beginning of a new phase in the woman's reproductive life: menopause.
Unfotunately, in some cases women experience a decrease in the quality and quantity of their eggs earlier than expected. This is known as early or premature menopause. For this reason, women who want to have children after age 35 should have their ovarian reserve tested.
Causes of low egg count
As explained above, age plays a major role when it comes to evaluating the ovarian reserve. As a matter of fact, they are inversely proportional factors: the older the woman, the lower the supply and quality of eggs.
In addition to age, there are other factors that can have a negative impact on the egg reserve and female fertility. These factors can lead to premature menopause or premature ovarian failure (POF), which refers to a situation in which menopause can happen earlier than usual.
Low ovarian reserve risk factors
Below are some of risk factors and conditions that can affect a woman's egg reserve:
- Medical and surgical procedures
- Radiotherapy
- Chemotherapy
- Stress
- Obesity
- Environmental factors
- Being exposed to pesticides or toxic agents
- Unhealthy lifestyle habits
- Certain conditions (e.g. endometriosis or pelvic inflammatory disease)
The speed at which woman's egg reserve diminishes varies on a case-by-case basis. This is the reason why menopause does not start at the same age in all cases.
What is a good ovarian reserve?
Your ovarian reserve can be evaluated thought various tests. The most usual is to do a hormonal analysis and an ultrasound study.
In the following section we detail the most common tests to evaluate the ovarian reserve.
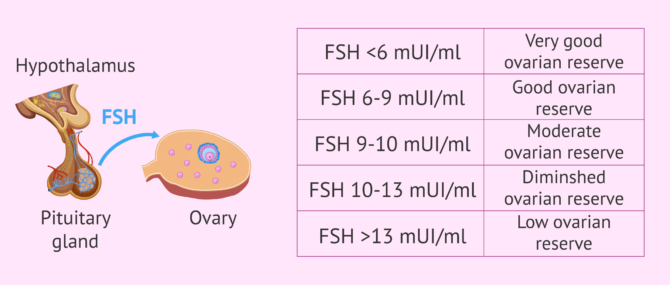
Follicle-stimulating hormone (FSH)
FSH is one of the hormones responsible for regulating the menstrual cycle. It is released by the pituitary gland to trigger the production of eggs. When the number of eggs is low, FSH levels increase to activate the ovary. In other words, high FSH levels translate into low ovarian reserve.
Normal FSH levels should be below 6 mIU/ml. Nevertheless, if they range between 6 and 9 mIU/ml, we can consider that the woman has a good ovarian reserve as well.
It is considered moderate if the levels of FSH vary from 9 to 10 mIU/ml, and low if they range between 10-13 mIU/ml. FSH levels above 13 mIU/ml indicate low ovarian reserve and therefore, the woman is near menopause.
For FSH levels to be properly measured, a blood test is donde on days 3 to 5 of the menstrual cycle, with the first day of the last menstrual period (LMP) being the first day of the cycle.
Anti-müllerian hormone (AMH)
AMH is released by the ovarian follicles, which are the ovarian structures that are home for the developing eggs. When the levels of AMH are high there is an elevated amount of mature eggs and the levels of AMH decreases with a decreasing number of eggs. For this reason AMH is considered an excellent marker for measuring female fertility.
Levels of AMH that range between 0.7 and 3.5 ng/ml indicate your ovarian reserve is normal. Levels below 0.7 ng/ml are considered an indicator of low ovarian reserve.
The levels of AMH in blood can be measured any day of the cycle. Contrary to FSH, the levels of AMH do not vary throughout the cycle. Therefore, the the results of AMH tests are very reliable as its levels are fairly constant and independent from other factors.
Estradiol (E2)
As the follicles develop, their release of estradiol increases. Therefore, measuring the value of this hormone can be helpful in assessing ovarian reserve. The higher the estradiol concentration, the more eggs are developing in that cycle.
However, high values of this hormone in the first days of the menstrual cycle (days 3-5) can also be an indication of low ovarian reserve. It is considered optimal for the estradiol value to be less than 40 pg/ml during these days.
To know the level of these hormones that measure ovarian reserve, all that is needed is a blood test. If you would like more information about this, please read this article: Can a woman´s egg count be measured with a blood test?
Antral Follicle Count (AFC)
From the moment of puberty a set of follicles develops each month, although only one reaches the ovulatory stage, when a mature egg cell is released. The remaining will degenerate eventually.
We distinguish the following phases of follicle development: primordial, primary, secondary, antral, and preovulatory (also known as Graaf follicle).
Antral follicles are marked by the formation of a fluid-filled cavity called antrum. This allows them to be seen in an ultrasound scan. In short, counting the number of antral follicles can give us an approximate idea of the woman's egg supply status. AFC results are more accurate if donde on days 3 to 5 of the menstrual cycle.
If you are interested in this topic and would like to continue reading then please click here: What is an antral follicle count and what is it for ?
Measurement of other factors
The AFC is the most accurate ultrasound parameter for assessing ovarian reserve, but it is not the only one.
Ovarian volume is also indicative of the number of primordial follicles in the ovary and therefore predictive of a woman's reproductive capacity.
When the ovarian volume is less than 3 ml it is likely that there is low ovarian reserve. If assisted reproduction is used it may happen that there is a low response to ovarian stimulation.
Some studies affirm that the volume of the ovary changes as a woman's age increases. However, this change begins at the age of 35 and not before.
Chances of getting pregnant
For a natural pregnancy to occur, sperm quality and count is a determining factor, but not the only one to keep in mind. Having a good ovarian reserve is key as well.
As the ovarian reserve diminishes with age, so do her chances of getting pregnant naturally. In fact, this is the reason why nowadays there is an increasing number of women who have to turn to fertility treatment to have children due to issues with their egg supply.
As explained above, advanced maternal age does not only affect the egg count, but also their quality. To put it simply, from age 35-37 onwards, getting pregnant can be a hard task.
Low ovarian reserve is one of the most frequent causes in difficulty in getting pregnant, either naturally or by means of IVF.
For this reason, when a woman undergoes fertility tests, evaluating her egg reserve is crucial, since it is an indicator of her response to ovarian stimulation and her prognosis.
Egg donation is the recommended fertility treatment in cases of declining ovarian reserve. It is a type of In Vitro Fertilization (IVF) that involves the use of donor eggs to increase the chances for pregnancy.
Interview of Dr Miguel Dolz about ovarian reserve
According to Dr. Miguel Dolz, it is fundamental to evaluate the ovarian reserve because the quantity of eggs that will be collected during in vitro fertilization treatment will define the reproductive prognosis of the couple.
The optimal ovarian reserve should be adjusted to the patient's age. In general, the standard value is 10 antral follicles and the FSH hormone level should be less than 10. In this case, the ovarian reserve is considered to be quite normal.
FAQs from users
Is there a relation between ovarian reserve and egg quality?
Ovarian reserve is a measure of the quantity and quality of the eggs; it is best measured by a combination of chronological age, antral follicle count (AFR) on ultrasound, and anti-mullerian hormone (AMH).
An AFR of less than 11 reflects diminished ovarian reserve and less than 6 is severe. AMH levels below 1.6 have been shown to reduce the number of eggs retrieved with IVF and may predict pregnancy outcome. Levels below 0.4 are severe.
Read more
Can low ovarian reserve be prevented?
The ovarian reserve physiologically decreases with age, this is the first cause to take into account and, unfortunately, it cannot be avoided.
There are other less proven factors, which are toxic substances. Toxins can condition fertility, although it is not known whether they directly affect the ovarian reserve or whether they act more on the quality. Smoking, for example, is one of these factors that can increase oxidative stress at the ovarian level.
Read more
How does low ovarian reserve affect IVF success rates?
We know as ovarian reserve or egg count the amount of eggs a woman carries at a particular stage of her lifetime. It is an indicator of her fertility at that point.
Measuring a woman's ovarian reserve allows us to determine the ability for her ovaries to produce eggs with fertility potential, that is, able to result in viable embryos, able to attach to her endometrial lining.
Moreover, as the egg reserve diminishes, so does the quality. This translates into a higher number of complications to achieve pregnancy, as well as to an increased miscarriage rate.
For all these reasons, the supply of eggs of females is a key factor to getting pregnant naturally as well as by means of IVF. The success rates of IVF are lower in women with a decreased egg supply.
Recommended for you: What Is a Good Number of Eggs Retrieved for IVF?
Is anti-Müllerian hormone (AMH) or antral follicle count (AFC) more reliable for assessing ovarian reserve?
There is no one test to assess ovarian reserve better than another, there are several methods. In addition, there are no tests to predict the pregnancy rate as such.
Read more
Is there any home method to measure ovarian reserve and fertility?
The methods mentioned above (measuring FSH, AMH, estradiol and AFC) are the most reliable for evaluating ovarian reserve. There is no way to measure ovarian reserve at home, although there do exist a series of tests you can do at home to get more information about your fertlity level.
These are the basal temperature test, the vaginal secretion test and the study of the position of the cervix. If you want to know the basics and the operation of each of them, we recommend you consult this article: Fertility signs in women
Is there any treatment for low ovarian reserve that allows pregnancy?
Achieving pregnancy with low ovarian reserve is complicated. There is no treatment to increase ovarian reserve, but there is a treatment to allow a woman with low ovarian reserve to achieve pregnancy.
This is in vitro fertilization (IVF), which is preceded by ovarian stimulation treatment. If even with this treatment pregnancy is not achieved, ovodonation is the way to choose to try to achieve gestation.
How can I know what my ovarian reserve is?
The ovarian reserve is the amount of eggs available in a woman at a given time, since this amount is reduced as time goes by.
The measurement of ovarian reserve in women is usually carried out through a blood test where the concentration of various hormones is determined: FSH, LH, estradiol and antimullerian hormone. In addition, this hormonal profile can be completed with a count of antral follicles by transvaginal ultrasound.
If a woman's ovarian reserve is low, she will most likely have to resort to assisted reproductive techniques to achieve pregnancy.
How many eggs does a woman release on Clomid?
Clomid, Clomifene or Clomiphene is a medication used for IVF ovarian stimulation. The purpose is to produce more than one egg per cycle (i.e. superovulation). The particular number of eggs a woman will be able to release on Clomid depends on each IVF patient and the response of her ovaries to IVF meds.
Recommended reading
If you would like to know more about howthe ovarian reserve is measured and the interpretation of the results, the following article may be of interest: Ovarian reserve test: What are the normal values?
If you are interested in more details anout the antimüllerian hormone then please click here: What is the function of antimüllerian hormone (AMH)?
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
Broekmans FJ, Kwee J, Hendricks DJ, Mol BW, Lambalk CB. A systematic review of tests predicting ovarian reserve and IVF outcome. Hum Reprod Update 2006
Broer SL, Broekmans FJ, Laven JS, Fauser BC. Anti-Müllerian hormone: ovarian reserve testing and its potential clinical implications. Hum Reprod Update 2014
Broer SL, van Disseldorp J, Broeze KA, Dolleman M, Opmeer BC, Bossuyt P, Eijkemans MJ, Mol BW, Broekmans FJ. Added value of ovarian reserve testing on patient characteristics in the prediction of the ovarian response and ongoing pregnancy: an individual patient data approach. Hum Reprod Update 2013
Depmann M, Faddy MJ, van der Schouw YT, Peeters PH, Broer SL, Kelsey TW, Nelson SM, Broekmans FJ. The relation between variation in size of the primordial follicle pool and age at natural menopause. J Clin Endocrinol Metab 2015.
Dewailly D, Andersen CY, Balen A, Broekmans F, Dilaver N, Fanchin R, et al. The physiology and clinical utility of antimüllerian hormone in women. Hum Reprod Update 2014.
Dunlop CE, Anderson RA. Uses of anti-Müllerian hormone (AMH) measurement before and after cancer treatment in women. Maturitas 2015.
Ferraretti AP, La Marca A, Fauser BC, Tarlatzis B, Nargund G, Gianaroli L. ESHRE working group on Poor Ovarian Response Definition. ESHRE consensus on the definition of ‘poor response’ to ovarian stimulation for in vitro fertilization: the Bologna criteria. Hum Reprod. 2011.
Huddelston HG. Biomarkers of ovarian reserve in women with polycystic ovary syndrome. Semin Reprod Med 2013.
Iwase A, Nakamura T, Nahakara T, Goto M, Kikkawa F. Assessment of ovarian reserve using anti-Müllerian hormone levels in benign gynecologic conditions and surgical interventions: a systematic narrative review. Reprod Biol Endocrinol 2014.
Practice Committee of the American Society for Reproductive Medicine. Testing and interpreting measures of ovarian reserve: a committee opinión. Fertil Steril 2015.
Raffi F, Metwally M, Amer S. The impact of excision of ovarian endometrioma on ovarian reserve: a systematic review and meta-analysis. J Clin Endoc Metab 2012.
Somigliana E, Berlanda N, Benaglia L, Vigano P, Vercellini P, Fedele L. Surgical excision of endometriomas and ovarian reserve: a systematic review on serum antimüllerian hormone level modifications. Fertil Steril 2012.
Uncu G, Kasapoglu I, Ozerkan K, Seyhan A, Yilmaztepe AO, Ata B. Prospective assessment of the impact of endometriomas and their removal on ovarian reserve and determinants of the rate of decline in ovarian reserve. Hum Reprod 2013.
Video ReproducciónAsistida.Org - Entrevista sobre la Reserva ovárica - by Dr. Miguel Dolz, on November, 2th 2017. [See original video in Spanish here]
FAQs from users: 'Why is age such an important factor in a woman's fertility?', 'Is there a relation between ovarian reserve and egg quality?', 'Can low ovarian reserve be prevented?', 'How does low ovarian reserve affect IVF success rates?', 'Is anti-Müllerian hormone (AMH) or antral follicle count (AFC) more reliable for assessing ovarian reserve?', 'Can a woman produce more eggs?', 'Is there any home method to measure ovarian reserve and fertility?', 'Can eggs come out during period?', 'Is there any treatment for low ovarian reserve that allows pregnancy?', 'How do I know how many eggs I have left?', 'Is ovarian reserve related to blood type?', 'How can I know what my ovarian reserve is?', 'How many eggs does a woman drop during ovulation?' and 'How many eggs does a woman release on Clomid?'.
Authors and contributors

More information about Michelle Lorraine Embleton













Hi
I have read several of your articles and I wonder what your opinion would be about my case. I am a young woman, 26 years old, single and I have been to several Assisted Reproduction clinics. My antimüllerian is 2.17, my FSH is 9.12 and the antral follicle count is 6-7 in each ovary and the hysterosalpingography is correct.
The opinion of several gynecologists is that the results do not correspond to my age, and that is why they do not agree between trying an AID cycle or an IVF cycle. I would like to know your disinterested opinion, what treatment would you recommend, what pregnancy rate would I have with an AID?
Thanks in advance for any advice or opinions
Orla
Hi OrlaZ
Since you are young and your AMH has come back with normal values it could be a good idea to try the artificial insemination first as it is a simpler and cheaper procedure and you have a chance of getting pregnant this way.
The success rate of AID (measured by birth rate) is about 20%. You can get more information about this here: Sucess rates in assisted reproduction.
I hope my answer is helpful and wish you the best.
Hi,
I conceived my baby girl at 38! I was told my ovarian reserve wasn´t bad for my age but that it would be more dificult to get pregnnat naturally.
WE DID IT! After 8 months of TTC we got that BFP. We both followed the advice of healthy lifestyle and timing our sexlife around ovulation, which was a bit weird to start with but it meant we did it more!
Good luck all.