Endometriosis is a chronic benign disease that affects 10-15% of women of reproductive age. This gynecological pathology consists of the appearance and growth of endometrial tissue in other locations outside the uterine cavity.
This abnormal growth occurs mainly in the pelvic cavity, both in the peritoneum and in the organs located in this cavity. Primarily, endometrial tissue can appear on a woman's ovaries and cause a type of cysts called endometriomas. Tissue may also be located in the fallopian tubes or in more unusual places such as the intestine.
Endometriosis can cause female infertility, in addition to other discomforts in a woman's daily life. Therefore, women affected by endometriosis are likely to need assisted reproductive treatment when they wish to seek pregnancy.
Provided below is an index with the 11 points we are going to expand on in this article.
- 1.
- 1.1.
- 1.2.
- 2.
- 3.
- 4.
- 4.1.
- 5.
- 6.
- 7.
- 8.
- 8.1.
- 8.2.
- 8.3.
- 8.4.
- 8.5.
- 8.6.
- 8.7.
- 8.8.
- 9.
- 10.
- 11.
Definition of endometriosis
During a woman's menstrual cycle, the inner layer of the uterus, known as the endometrium, is renewed each month to offer the possibility of harboring an embryo and resulting in pregnancy endometrium endometrium, is renewed each month to offer the possibility of harboring an embryo and giving rise to a pregnancy. If this does not occur, the endometrium is shed in the form of menstruation.
Endometriosis is a pathology that derives from the alteration of the endometrium during the menstrual cycle. Instead of growing in the uterus, endometrial tissue develops in other extrauterine sites, which can cause bleeding and severe pain.
Endometriosis is a fairly common gynecological disorder in women of childbearing age. In addition, this uterine pathology usually causes sterility in 30-50% of the women who suffer from it.
Endometriosis is a hormone-dependent disease, that is, it undergoes changes depending on the hormones that act in the woman's menstrual cycle: estrogens and progesterone.
Specifically, estrogen release contributes to a greater degree to the progression of endometriosis. However, cases have also been studied before puberty and in women presenting at menopause.
What types of endometrial plaques are there?
The plaques of endometrial tissue that form outside the uterine cavity can vary in size depending on the severity of the endometriosis.
Therefore, it is important to differentiate between the 3 types that exist in order to assess endometriosis. From least to most severe, the types of endometrial plaques are as follows:
- Implants
- are small and superficial.
- Nodules
- are larger and can be invasive.
- Endometriomas
- when cysts form on the ovaries, also called chocolate cysts or endometriotic cysts.
The course of endometriosis is complicated to predict. Some women have small implants that do not change in size over time. In contrast, other women may have implants that spread and become invasive nodules.
Where is it located?
Endometriosis can appear in different organs of the body. In general, plaques of endometrial tissue will be located in the pelvic cavity, where the genital organs are located, but they can also appear in extragenital areas.
Therefore, we can make the following classification of endometriosis according to its specific location:
- Ovarian endometriosis
- located in the ovaries. It is possible that the endometriotic ovarian cysts discussed above may form.
- Tubal endometriosis
- located in patent fallopian tubes.
- Pelvic endometriosis
- located in the uterine ligaments or the pouch of Douglas (space between the rectum and the vagina), among others.
- Peritoneal endometriosis
- located superficially in the ovaries and the superficial peritoneal area.
- Rectovaginal endometriosis
- located in a tissue that lies between the rectum and the vagina, below the pouch of Douglas.
- Internal endometriosis or adenomyosis
- refers to the invasion of the endometrium into the myometrium, the inner muscular layer of the uterus.
- Other external areas
- for example, endometriosis found in the abdominal area or in other organs that are not part of the reproductive system, such as the bladder, ureters, bowel, rectum, or lungs.
Endometriosis may not only be limited to the surface but may also affect the interior of the organ. This would be a more severe type of endometriosis, known as deep infiltrative endometriosis deep infiltrative endometriosis which could prevent the correct functioning of the organ.
Symptoms and consequences
Endometriosis does not cause symptoms in most women who suffer from it, unless it is severe endometriosis.
However, some women with endometriosis do have some discomfort, the most common being pain during menstruation.
As mentioned above, endometrial implants respond to hormonal changes. Therefore, when menstrual bleeding occurs, these implants also bleed, causing bleeding that cannot flow out.
The blood from the endometrial plates that cannot be evacuated to the outside causes inflammation of the tissues where they are located and the formation of scars, giving rise to what is known as endometrial adhesions.
Other symptoms may also appear more or less frequently. Below, we will discuss all these possible symptoms of endometriosis in women:
- Pelvic, abdominal and lower back pain, usually associated with menstruation.
- Dyspaurenia: pain during or after sexual intercourse.
- Metrorrhagia: premenstrual bleeding or bleeding between periods.
- More abundant and long-lasting menses.
- Hematuria: pain and bleeding when urinating or defecating, especially if constipation is present.
- Tiredness, fatigue and low back pain.
- Psychological symptoms in the most severe cases, preventing the patient from leading a normal lifestyle.
It should be noted that the intensity of these symptoms does not depend on the degree of endometriosis. If the woman has symptoms with endometriosis, they are just as noticeable whether the endometriosis is mild, moderate, or severe. What does appear to exist is a direct relationship between difficulty conceiving and the type of lesions.
Degrees of endometriosis
Endometriosis can be classified into levels or grades depending on the lesions caused and their severity, although there is no generalized way to do this.
The classification most commonly used today is the one recommended by the American Society for Reproductive Medicine (ASRM):
- Endometriosis grade 1 (minimal)
- isolated implants appear without adhesions.
- Endometriosis grade 2 (mild)
- endometriosis plaques are superficial and smaller than 5 cm. There may be adhesions to the surface of the peritoneum and ovary, but without affecting other organs.
- Endometriosis grade 3 (moderate)
- there are multiple endometrial nodules and most of them are invasive. In addition, there may be adhesions in the tubes or ovary as well.
- Endometriosis grade 4 (severe)
- endometrial plaques are multiple, superficial and deep. They form large cysts of endometrial tissue in the ovary that fill with blood (chocolate cysts).
In the most severe cases of grade IV endometriosis, surrogacy or surrogate gestation, commonly known as surrogate motherhood, may be the only option to have a child.
Causes of endometriosis
Currently, the exact origin of endometriosis is not known. However, there are several theories that explain its possible formation.
The following is a list of the most widely accepted possible causes of endometriosis today:
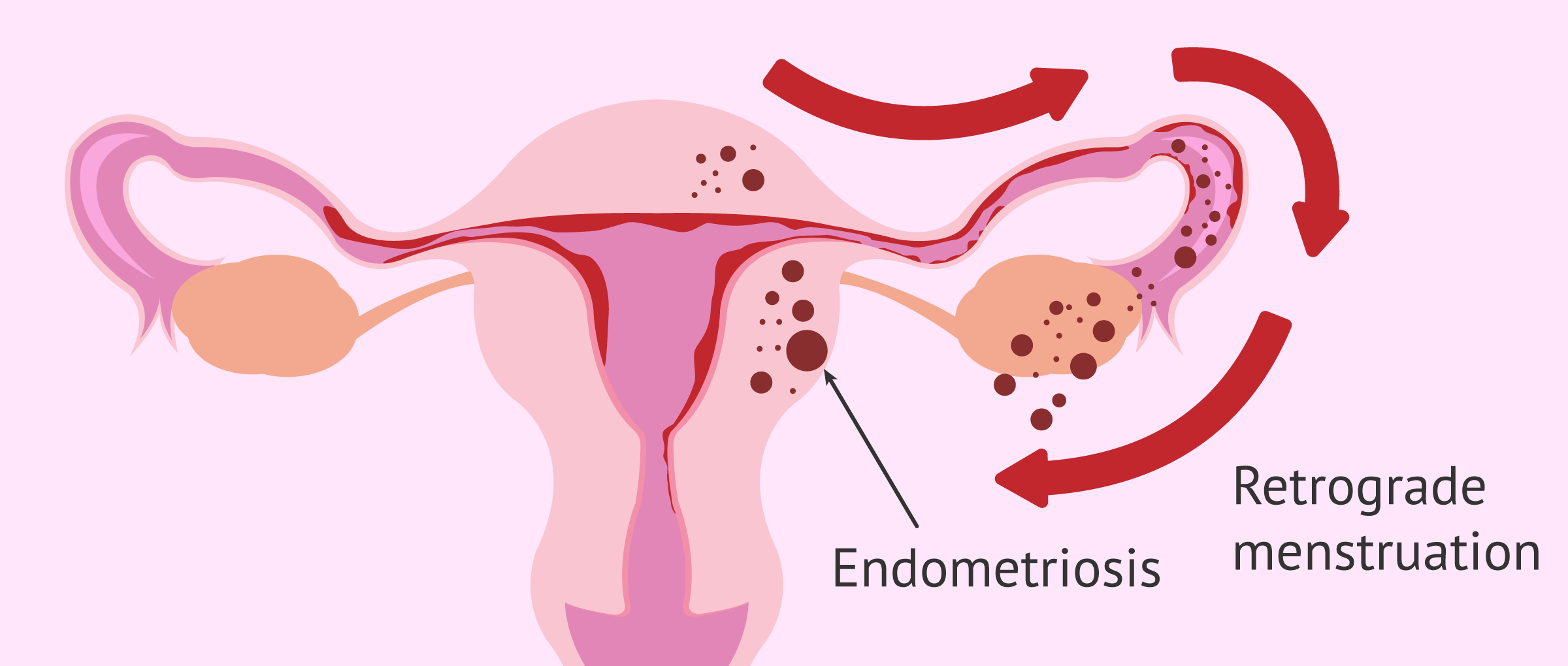
- Retrograde menstruation
- the endometrium is not completely eliminated during menstruation and, as a consequence, some endometrial fragments flow backwards through the fallopian tubes, which means that they can be deposited on the pelvic organs.
- Immune system disorders
- this theory is based on the inability of the female body to destroy the endometrial implants located outside the uterine cavity.
- Metaplasia
- transformation of tissues outside the uterus into endometrial tissues in response to genetic or environmental factors.
- Vascular transplantation
- it is possible that some fragments of endometrium may travel through the blood or lymphatic vessels and implant in distant areas.
Most likely there is a multifactorial mechanism that explains endometriosis. All these possible theories about the formation of endometriosis are detailed in the following post: The causes of endometriosis.
Once we have managed to find out the etiology of this disease, it will be possible to find more effective therapies to cure endometriosis definitively.
What are the risk factors?
It has been shown that there are some risk factors that may favor the appearance of endometriosis in women, although this is not always the case. Some of them are as follows:
- Having a mother or sister with endometriosis, as it could be hereditary.
- Onset of menstruation at an early age.
- Not having had children yet.
- Having short menstrual cycles, i.e., having more frequent periods (polymenorrhea).
- Heavy bleeding (hypermenorrhea) and long duration of menstruation (7 days or more).
- Have a closed hymen that prevents the outflow of menstruation.
- Having undergone surgery of the uterus, for example, after cesarean section or curettage.
It should be noted that the women most affected by endometriosis are those between 30 and 50 years of age, with the average age of onset being 37. However, adolescent women can also be affected by endometriosis. In fact, there are exceptional cases in girls between 12 and 15 years of age.
On the other hand, pelvic endometriotic foci have also been described in menopausal age, although their occurrence is rarer.
What is the diagnosis of endometriosis like?
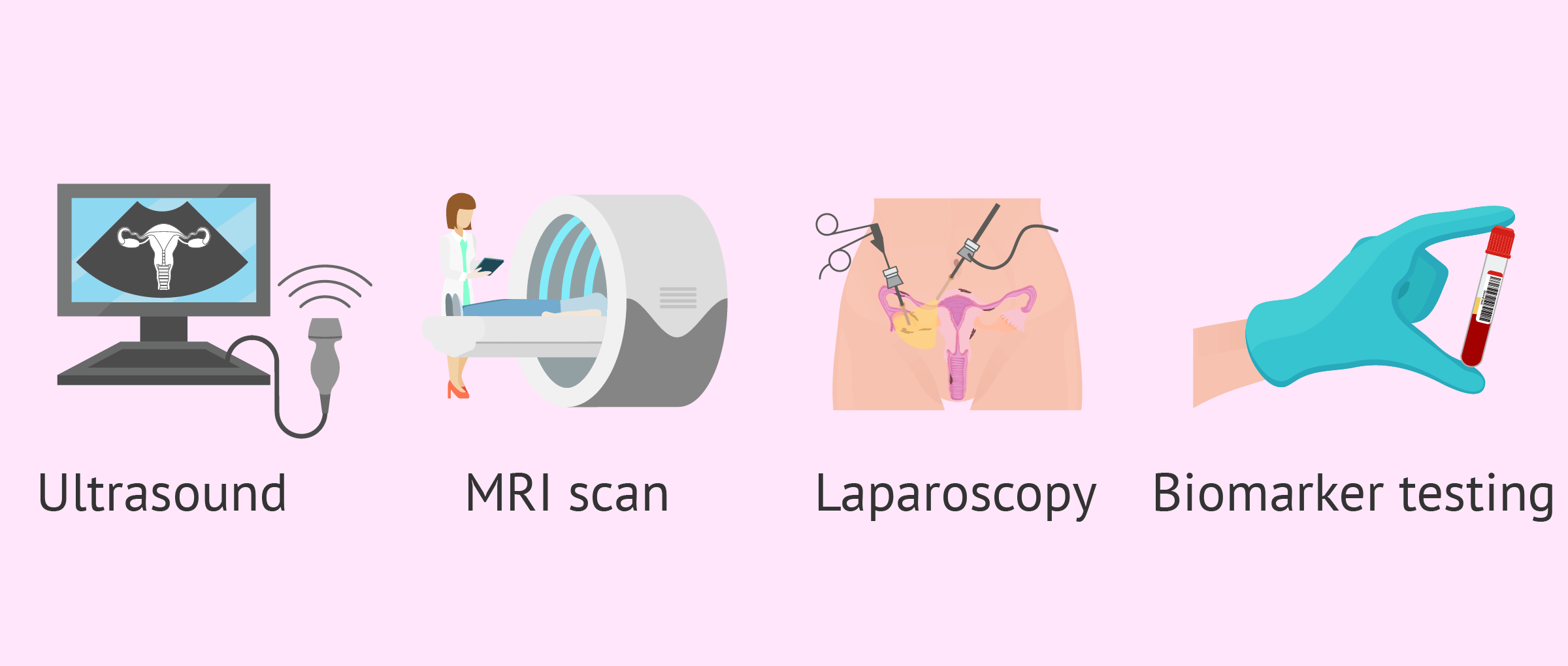
The first warning sign of possible endometriosis is acute pain during menstruation. In this case, the gynecologist should perform a thorough physical examination of the patient, especially examining the pelvic area.
A transvaginal ultrasound can help visualize endometriotic cysts in the ovary or deep nodules in other areas. However, for an accurate and safe diagnosis, surgery will be necessary to visualize the lesions caused by endometriosis.
Magnetic resonance imaging(MRI) may also be used in those patients in whom the diagnosis by ultrasound is not clear or before surgery, to determine the exact location and depth of the lesions.
The gynecologist will only be sure of the diagnosis when performing a laparoscopy, which is a minor surgery under general anesthesia in which, through a tube equipped with a lens and a light, the inside of the abdominal cavity can be observed. However, because it is a costly procedure and because of the risks it poses to the patient, attempts are made to avoid performing it.
The latest research attempts to find biomarkers of endometriosis that provide a diagnosis by performing a simple blood test or urine analysis. These markers would be substances created by our body in response to the disease or created by the disease itself.
Endometriosis markers have already been found to be present in the endometrial fluid, such as the tumor marker CA-125, and their analysis would allow detection of the disease. However, to date, its diagnostic value is limited.
For more information on this topic, you can continue reading here: Diagnosis of endometriosis.
Treatment for endometriosis
There is currently no pharmacological treatment that definitively cures endometriosis, but there are different approaches to try to make the disease as bearable as possible.
Endometriosis, being hormonally regulated, will be present throughout a woman's fertile life. Occasionally, it may extend beyond menopause.
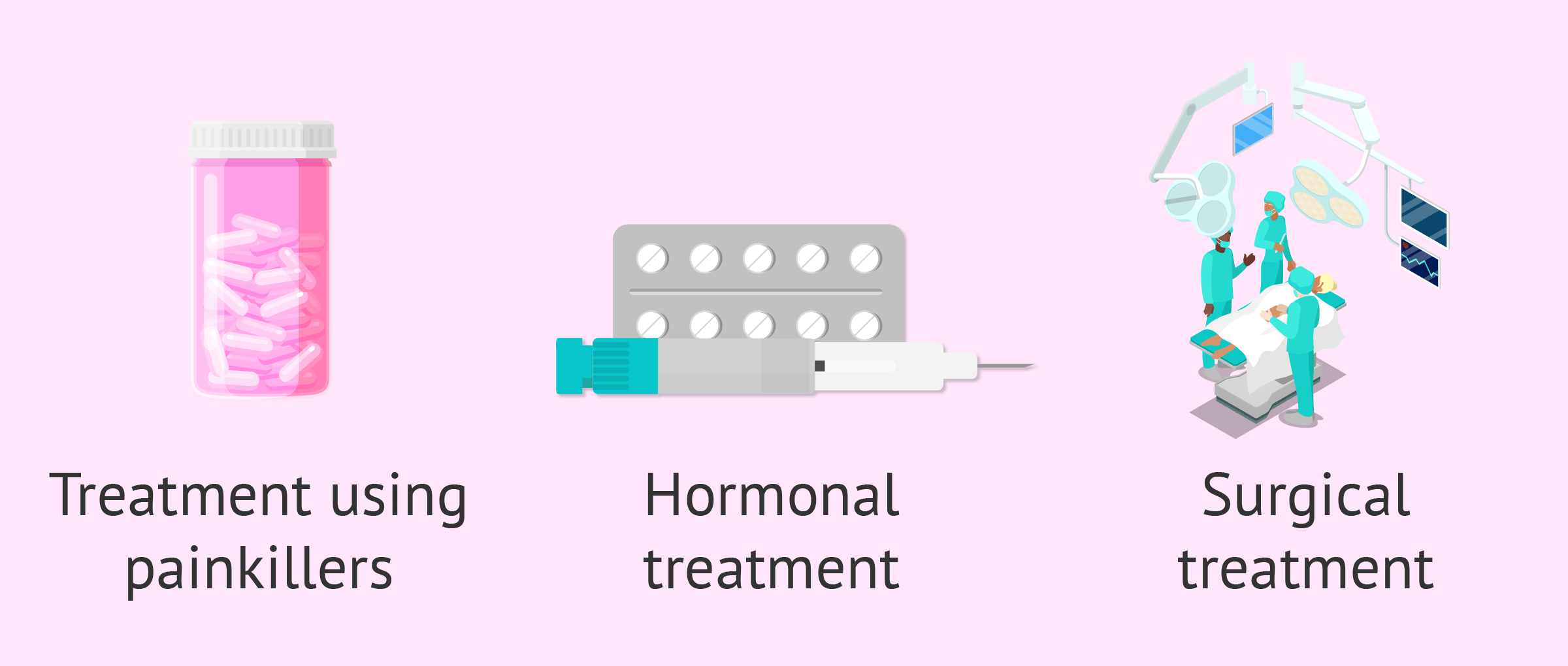
Depending on the severity of the patient's symptoms, her age, and reproductive desire, the following treatments can be performed:
- Analgesics
- in cases of mild endometriosis, pain medication may be sufficient. However, this medication is not sufficient for all patients.
- Hormonal
- by administering hormones involved in the menstrual cycle, it is possible to slow down the development of endometrial tissue. Examples of these treatments are found with oral contraceptives.
- Surgical
- in the most severe cases, surgical treatment of endometriosis may be chosen. Depending on the location and extent of the tissue, one surgical technique or another will be used.
As we can see, the treatment can be analgesic, hormonal or surgical depending on the endometriosis involvement. In milder cases, treatment will consist of analgesics for pain. In more severe cases, involving chronic pain, surgery may be the solution.
The patient should be informed of the advantages and disadvantages of each treatment, since some, such as hormonal treatment, may be incompatible with the desire to have children.
You can get more detailed information about this in the following article: Treatment of endometriosis.
Is pregnancy possible with endometriosis?
As we have said, not all women with endometriosis will suffer infertility. However, endometriosis itself causes problems in conceiving in 40% of cases, being the third reason for gynecological consultation for female infertility.
First, endometriosis affects the ovarian reserve, both the quantity and quality of the eggs. The progression of endometriosis causes the loss of healthy ovarian tissue, which is replaced by endometrial tissue. In fact, the surgery itself to remove endometriomas from the ovary may contribute to this decrease in ovarian reserve.
On the other hand, endometriosis can also affect the fallopian tubes. On the one hand, endometrial implants can obstruct the fallopian tubes, which prevents the egg and sperm from meeting and fertilizing. The functionality of the fallopian tubes may also be affected and prevent the correct transport of the embryo to the uterus even if fertilization occurs.
Considering seeing a fertility specialist? Don't forget that, in the field of Reproductive Medicine, as in any other medical area, it is crucial that patients rely on the doctors and staff that will help them through their treatment cycle. Logically, conditions vary from clinic to clinic. For this reason, we recommend that you generate your Fertility Report now. It will offer you a list of clinics that have passed our rigorous selection process successfully. Furthermore, the system will make a comparison between the fees and conditions of each clinic so that you can make a better-informed decision.
In conclusion, it is likely that women with endometriosis will need to resort to assisted reproduction in order to have children. Depending on the severity, the treatments used are as follows:
- Artificial insemination (AI).
- In vitro fertilization (IVF).
- Ovodonation.
Interestingly, once pregnancy is achieved, it has a protective effect on the development of endometriosis. The ovaries remain at rest and, therefore, there is no estrogen release to promote the development of endometriomas.
For more information about fertility treatments to achieve pregnancy, we invite you to visit the following article: Pregnancy with endometriosis.
FAQs from users
What types of endometriosis are there?
Endometriosis can occur in different locations, such as the ovaries, fallopian tubes, behind the uterus, in the uterine ligaments, in the pelvic cavity and, more rarely, in areas such as the bladder or lungs.
Depending on where the endometrial tissue develops, we distinguish:
- Ovarian endometriosis
- Tubal or fallopian tube endometriosis
- Pelvic endometriosis
- Rectal endometriosis
- Intestinal endometriosis
- Peritoneal endometriosis
What are your reproductive options if you have stage IV endometriosis?
Endometriosis affects 10-15% of all women. Of women with endometriosis, 30-50% are estimated to have infertility; of women with infertility, 25-50% are estimated to have severe endometriosis. A hallmark of endometriosis is inflammation and subsequent formation of adhesions in the pelvis. These adhesions distort the pelvic anatomy and impacts the woman in a variety of ways. The most direct consequence of adhesions can be a disruption of the anatomical relationship between the ovaries and fallopian tubes. In advanced cases of endometriosis, tubal blockage may occur to the point of a hydrosalpinx which may require removal before any fertility treatment.
The most appropriate treatment for each couple will depend on a number of factors including the woman’s age, the duration of infertility, her ovarian reserve, the sperm analysis, a history of past surgery for endometriosis and its severity.
For women younger 35 years of age with low stage disease, a trial of Fertility treatment with intrauterine insemination (IUI) is recommended. However, for women greater than or equal to 35 years of age with advanced stages of endometriosis (stages III and IV), IVF is recommended due to the higher pregnancy rate. Of note, advanced endometriosis, compared to other diagnoses, may reduce the pregnancy rate with in vitro fertilization.
What are the solutions for women with fertility problems resulting from endometriosis?
Endometriosis is indeed a very important problem in the western world and one of the main causes of infertility. The solutions that Assisted Reproduction can provide to this problem will depend on the degree of severity of the endometriosis (mild cases usually benefit from simple treatments, while more severe cases may require In Vitro Fertilization). In addition, nowadays, with the possibility of freezing the patient's eggs, it is possible to make this fertility "reserve" in women with severe cases that may end up with the loss of both ovaries.
Has progress been made in the treatment of endometriosis, as well as in the knowledge of its origin?
There is increasing evidence that it is closely related to immunological factors that cause in certain women, something that occurs normally, such as part of the menstruation passing from the uterus to the abdominal cavity through the tubes without further complications, causing the creation of cysts in the ovaries and implants in the peritoneum that can be very harmful to the patient.
As regards treatment, drugs are being tested to reduce the development of the disease, although ideally in the future it will be possible to prevent the disease from its origin.
Is endometriosis contagious?
Endometriosis is not a sexually transmitted disease and therefore is not contagious. Although the cause is unknown, it is known that there is no risk of contagion.
Is endometriosis hereditary?
Genetic factors are suspected to be involved in this pathology, since cases have been detected of women within the same family suffering from it.
Women whose mother or sister suffers from endometriosis are 6 times more likely to develop this disease than the rest of the general population.
Are endometriosis and endometritis the same?
No. Endometritis refers to inflammation or irritation of the endometrium inside the uterus, possibly due to a bacterial infection.
Endometriosis, on the other hand, means invasion of the endometrium into other tissues outside the uterus, the causes of which are not yet confirmed.
Does treatment cure endometriosis?
Drugs and natural therapies can only partially or completely relieve symptoms. On the other hand, surgery can help improve the health status of women with endometriosis to a great extent after removal of all endometrial plaques. However, these solutions are not definitive, as endometriosis returns over time. The only way to completely eliminate endometriosis is to perform a hysterectomy, i.e. the removal of the uterus.
Recommended readings
Endometriosis can affect a woman's fertility by several mechanisms in a more or less severe way. If you want to learn more about this topic, you can continue reading at the following link: Fertility and endometriosis.
On the other hand, if you want to know about other diseases related to the uterus and female fertility, you can access the following post: Female infertility due to a uterine factor.
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
ADAEC. Endometriosis: Documento de consenso S.E.G.O. La voz digital [periódico digital] 2007.
Adamson GD, et al. Creating solutions in endometriosis: global collaboration through the World Endometriosis Research Foundation. J of Endometriosis 2010;2(1):3-6.
Allen C, Hopewell S, Prentice A. Non-steroidal anti-inflammatory drugs for pain in women with endometriosis. Cochrane Database of Systematic Reviews 2005, Issue 4.
American College of Obstetricians and Gynecologists (ACOG). Medical management of endometriosis. Washington (DC): American College of Obstetricians and Gynecologists (ACOG); 1999 Dec. 14 p. (ACOG practice bulletin; no. 11).
ASRM American Society for Reproductive Medicine. Endometriosis. Guía para pacientes. En: Serie de Información para pacientes. Revisado en 2013. Birmingham, Alabama.
Clement PB. The pathology of endometriosis: a survey of the many faces of a common disease emphasizing diagnostic pitfalls and unusual and newly appreciated aspects. Adv Anat Pathol. 2007; 14(4):241-60
Davis L, Kennedy SS, Moore J, Prentice A. Modern combined oral contraceptives for pain associated with endometriosis. Cochrane Database of Systematic Reviews: Reviews 2007, Issue 3.
Di W, Guo SW. Curr Opin Obstet Gynecol. The search for genetic variants predisposing women to endometriosis. 2007; 19(4):395-401.
Dra. MA. Martínez Zamora. (2013). Actualización sobre la etiopatogenia de la endometriosis. Hospital Clínic Universitari de Barcelona. Acadèmia de Ciències Mèdiques i de la Salut de Catalunya i de Balears, Societat Catalana d’Obstetricia i Ginecologia
European Society for Human reproduction (ESHRE). Guideline for the diagnosis and treatment of endometriosis. Human Reproduction, 2005; 20(10):2698-2704.
Giudice LC. Endometriosis. Clinical Practice. N Engl J Med 2010;362(25):2389-98.
Guo S-W, et al. Reassessing the evidence for the link between dioxin and endometriosis: from molecular biology to clinical epidemiology. Mol Hum Reprod 2009;15(10):609-24.
Hughes E, Fedorkow D, Collins J, Vandekerckhove P. Ovulation suppression for endometriosis. Cochrane Database of Systematic Reviews 2003, Issue 3.
Husby GK1, Haugen RS, Moen MH. Diagnostic delay in women with pain and endometriosis. Acta Obstet Gynecol Scand. 2003 Jul;82(7):649-53.
Moen MH and Magnus P. The familial risk of endometriosis. Acta Obstet Gynecol Scand 1993;72(7):560-4.
Nnoaham KE, et al. Impact of endometriosis on quality of life and work productivity: a multicenter study across ten countries. Fertil Steril 2011;96(2):366-373.
Rogers PA, et al. Priorities for endometriosis research: recommendations from an international consensus workshop. Reprod Sci 2009;16(4):335-46.; Adamson GD, et al. Creating solutions in endometriosis: global collaboration through the World Endometriosis Research Foundation. J of Endometriosis 2010;2(1):3-6.
Royal College of Obstetricians and Gynaecologists. The investigation and management of endometriosis. London: RCOG; 2006. Green-top Guideline No. 24.
Simoens S, Hummelshoj L, D'Hooghe T. Endometriosis: cost estimates and methodological perspective. Hum Reprod Update. 2007; 13(4):395-404.
Society of Obstetricians and Gynaecologists of Canada. Consensus guidelines for the management of chronic pelvic pain. Ottawa: SOGC; 2005. SOGC Clinical Practice Guidelines No 164.
Vigano P, et al. The relationship of endometriosis and ovarian malignancy: a review. Fertil Steril 2008;90(5):1559-70.
Vigano P, Somigliana E, Vignali M, Busacca M, Blasio AM. Genetics of endometriosis: current status and prospects. Front Biosci. 2007; 12:3247-55.
Wieser F, Cohen M, Gaeddert A, Yu J, Burks-Wicks C, Berga SL, Taylor RN. Evolution of medical treatment for endometriosis: back to the roots? Hum Reprod Update. 2007; 13(5):487-99.
FAQs from users: 'What types of endometriosis are there?', 'What are your reproductive options if you have stage IV endometriosis?', 'What are the solutions for women with fertility problems resulting from endometriosis?', 'Has progress been made in the treatment of endometriosis, as well as in the knowledge of its origin?', 'Can endometriosis lead to cancer?', 'Is endometriosis contagious?', 'Is endometriosis hereditary?', 'Are endometriosis and endometritis the same?' and 'Does treatment cure endometriosis?'.
Authors and contributors
More information about Cristina Algarra Goosman














Hello, I have constant pain in my uterus and I don’t know what the reason is, in the ultrasound they didn’t see anything wrong. I would like to know if there is still a chance of having endometriosis.
Hi Vanessa,
Continued pain along with painful periods as well as pain in other areas around the pelvic area may be indicators of endometriosis.
These adhesions cannot necessarily be seen in ultrasound so it would be necessary to do an exploratory intervention such as laparoscopy as you will be able to obtain a sample of tissue to analyze and indicate whether it is endometrial tissue or not.
I leave you the following article so you can read about the diagnosis of endometriosis: Diagnosis of endometriosis.
I hope I have helped you,
Best regards