Women can undergo a series of tests to know if they are infertile or not.
Among the most common fertility tests for women available nowadays, we can find the hysterosalpingography (HSG) or uterosalpingography, as well as other gynecological tests that will be explained below. Commonly, women visit a fertility specialist to have their fertility checked when they start noticing the first signs of not being able to get pregnant.
Once the cause of infertility has been established, it will be possible to apply an appropriate assisted reproduction treatment to achieve pregnancy.
Provided below is an index with the 10 points we are going to expand on in this article.
- 1.
- 2.
- 3.
- 4.
- 5.
- 5.1.
- 5.2.
- 5.3.
- 6.
- 7.
- 7.1.
- 7.2.
- 7.3.
- 7.4.
- 7.5.
- 7.6.
- 7.7.
- 8.
- 9.
- 10.
How is female fertility tested?
Fertility is a two-way thing, and for this reason couples are recommended to visit a fertility specialist in order to have their fertility checked at the same time if pregnancy has not occurred after 12 months trying to conceive without luck. In women over 36, this time period is reduced to 6 months.
If you need to undergo IVF to become a mother, we recommend that you generate your Fertility Report now. In 3 simple steps, it will show you a list of clinics that fit your preferences and meet our strict quality criteria. Moreover, you will receive a report via email with useful tips to visit a fertility clinic for the first time.
For female infertility to be diagnosed, the fertility specialist will first interview the patient, and then run some basic tests:
- Hormonal tests
- Used to check the patient's sex hormones as well as other hormones that play a role in the menstrual cycle.
- Gynecological tests
- To evaluate the anatomy of the uterus and if the ovaries are working properly.
- Hysterosalpingography
- To check tubal patency.
- Chromosome testing (karyotyping)
- To dismiss the possibility for a chromosomal alteration to be present.
Should the results of any of these tests be altered, the doctor can ask you to undergo some additional screening tests, including an endometrial biopsy and a hysteroscopy, which are explained below.
Hormone blood tests
Hormone blood tests for female fertility are used to measure the levels of the main female sex hormones. This way, we can find out the presence of potential endocrine problems that could be affecting your menstrual cycle, and thereby leading to female infertility. The ultimate goal is to evaluate if your ovaries and pituitary gland are working properly.
In short, these are the main hormones evaluated through this blood work:
- Follicle-stimulating hormone (FSH)
- Secreted by the pituitary gland, FSH is responsible for stimulating the ovaries and cause the follicles to grow. The follicles are the structures that contain the eggs.
- Estradiol (E2)
- It is released by the cells that surround the egg as it matures inside the follicle.
- Luteinizing hormone or lutropin (LH)
- It is produced by the pituitary gland as well. Its role is to control the menstrual cycle along with FSH. It increases substantially halfway through the cycle (LH surge) to induce ovulation.
- Progesterone (P4)
- It is secreted by the follicle that remains in the ovary following ovulation in order for the endometrial lining to prepare for embryo implantation after egg fertilization.
- Anti-müllerian hormone (AMH)
- The follicles in the ovaries are responsible for its production. The levels of AMH are proportional to the egg count, and for that reason it is used to measure the ovarian reserve. It is usually measured on day 3-5, although it can be evaluated at any point through the cycle, as its levels do not vary.
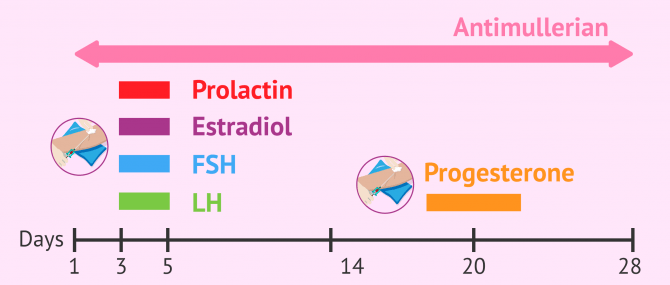
Tests to measure FSH, estradiol, prolactin, and LH should be done between days 3-5 of the cycle, that is, on day three through day 5 of the patient's menstrual period. They are used to measure the values of these hormones on the first days of the cycle.
Blood tests to evaluate hormones such as TSH (thyroid-stimulating hormone), free thyroxine (T4), free triiodothyronine (FT3), prolactin, and total testosterone may also be required. Although these are not sex hormones, if their levels are above or below the average, they can have a negative impact on the hormones that control the menstrual cycle and the ovulation in particular.
To have these hormones checked, two blood tests are required: one at the beginning of the menstrual cycle, and another one at the end.
Also, tests to detect sexually transmitted diseases (STDs) as well as infectious or viral diseases that could damage fertility are strongly recommended.
Female fertility tests at doctor's
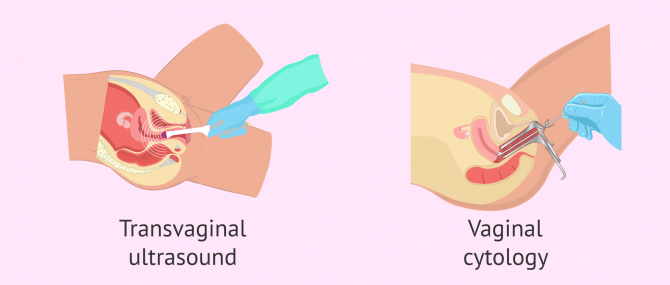
Through a pelvic or transvaginal ultrasound, the gynecologist can see the uterus and the ovaries of the patient. This gynecological test is used for two purposes:
- To check whether there exists a malformation in the uterus or any other uterine anatomical abnormality
- To count the number of antral follicles during the first days of the cycle
To this end, the gynecologist uses a catheter, which is covered with a condom, and inserts it through the vagina with a lubricant gel. The catheter sends sound waves that allow the specialist to see on a screen the structure of the uterus and the ovaries when it touches them. Although the pressure exerted by the catheter can cause certain discomfort, it should be clear that this test is totally painless.
Also, you are likely to undergo a pap smear, pap test, or cytology test. The purpose of this test is to analyze a small amount of cells from the cervix, which are gently scraped with a curette, to look for the presence of infections or cellular alterations that can compromise the woman's fertility.
Hysterosalpingography (HSG)
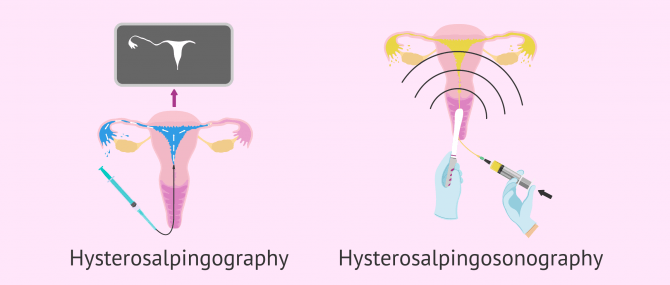
Hysterosalpingography or uterosalpingography is a diagnostic test used to observe the structure of the uterus and the Fallopian tubes, as well as their functionality through X rays (radiography), aided by a fluid that contains a dye.
This is a key diagnostic test when it comes to evaluating a woman's fertility, as lacking tubal patency means that the sperms are unable to go through the tubes, reach the egg, and fertilize it. Also, the existence of an anomaly in the anatomy of the uterus or the tubes can prevent you from getting pregnant.
For a HSG to be done, the woman lies in lithotomy position on an examining table, and a catheter is inserted through her cervix. The catheter contains a radiopaque dye that will pass through her cervix, uterus, and tubes. Unless there exists a blockage, the fluid will exit the pelvic cavity easily.
In short, this test allows us to diagnose the following problems:
- Structural abnormalities of the uterine wall
- Abnormal formations in the uterus, including myomas, polyps and adhesions
- Pathologies that cause inflammation of the tubes, e.g. salpingitis
- Pathologies that block the tubes, e.g. hydrosalpinx
Also, a hysterosalpingography can also be used to open the Fallopian tubes thanks to the passage of the radiopaque dye. For this reason, some women are able to achieve pregnancy naturally after undergoing a HSG.
Get detailed information about the definition of hysterosalpingography and the steps involved in this diagnostic test here: How is a hysterosalpingography done?
Additional tests
Aside from the diagnostic tests already listed above, there are other fertility tests for women to have their fertility tested. The most relevant ones are explained below:
Chromosome testing (karyotyping)
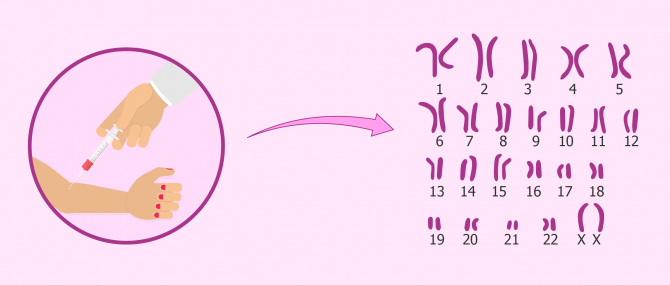
The karyotype is the set of chromosomes contained in each cell. In total, humans have 46 chromosomes, out of which we can find 22 pairs of non-sex chromosomes (autosomal), and 2 sex chromosomes (XX for females, XY for males).
Karyotyping is one of the most important procedures performed in a fertility lab. It is a chromosome analysis used to look for the presence of abnormalities that may be affecting fertility. Such abnormalities can be related to the number of chromosomes (incorrect amount) or to their structure (structural alterations).
Given that all the cells with a nucleus have chromosomes, this test can be done by means of a blood test. The cells to focus on are white blood cells (WBC) or lymphocytes.
Karyotype testing is especially important in cases of repeated miscarriage or implantation failure.
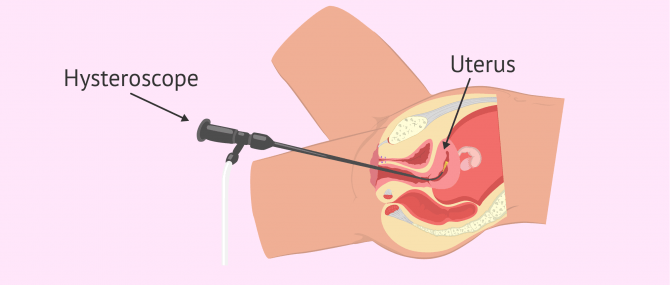
Hysteroscopy
It allows the uterine wall to be observed entirely. This way, the specialist can diagnose potential uterine abnormalities like, polyps, myomas, or lesions of the endometrium that could no be detected accurately by ultrasound or hysterosalpingography.
This gynecological test can be done at the doctor's and involves the insertion of a thin viewing tool called hysteroscope through the vagina and the cervix. By doing this, the doctor is able to observe the patient's uterine cavity.
Moreover, it allows the specialist to see the entrance to the Fallopian tubes, but the hysteroscope cannot be inserted through them due to their reduced diameter.
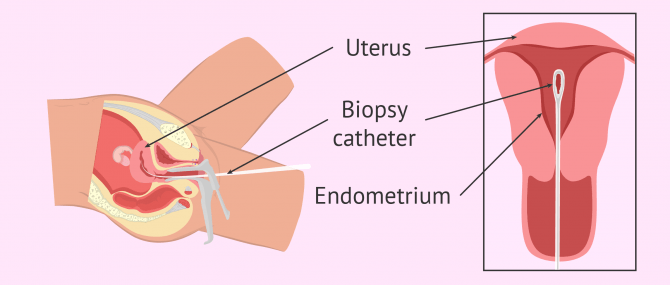
Endometrial biopsy
This diagnostic test involves the removal of a tissue sample from the innermost layer that lines the cavity of the uterus (i.e. endometrium). Then, it is examined under the microscope to look for the existence of an anomaly in its cells.
The specialist inserts a small tube inside the uterus to take a small sample of endometrial lining. This outpatient procedure can be done using local anesthesia or not at the doctor's office.
Endometrial biopsy is usually indicated in cases of repeated implantation failure, in order to study endometrial receptivity.
Interview with Dr. Sergio Rogel
The gynaecologist Sergio Rogel, the medical director of IVF Spain, explains in detail all the diagnostic tests that are usually performed on women who come to a fertility clinic to study their fertility. As the doctor tells us:
Infertility is defined as the impossibility of having children for a year, once it is assumed that the couple does not use contraception and has sexual intercourse. From that moment on, the situation is no longer normal and a doctor should be consulted. Of course, there are exceptional situations where you should also see a doctor even before one year has passed.
FAQs from users
What are the main female infertility tests?
The main female infertility tests include:
- Blood test – Day FSH and E2, Anti mullerian hormone (AMH), TSH, Prolactin
- Tube test – Hysterosalpingogram
- Pelvic ultrasound with antral follicle count
How is a Hysterosalpingogram performed?
A HSG is a type of x-ray examination that aims to examine the presence of pathologies in the uterine cavity, and well as tubal patency. It is recommended to evaluate potential causes of primary sterility. It involves inserting a cannula until the entrance of the uterus, through which a special radio-opaque contrast material dye is inserted. The contrast material dye will fill in the cavity and the tubes. Then, a series of x-rays will be done to detect potential abnormalities or blockages in the different structures. It is a simple procedure that is typically done in the first 10 days of the cycle. During its performance, the woman may feel period-like symptoms. Hospitalization is not required, and its duration ranges between 15 and 30 minutes approximately.
How much does a female fertility test cost?
It depends on the tests required and the location where they are performed, but in general the cost of a basic female fertility study can range from $150 to $500 on average.
A hysterosalpingography can cost up to $800-3,000. As for a pelvic ultrasound, a pap smear, and a gynecological exam, the price can be $200 in total, and hormone blood tests can cost up to $50-200 each.
How do you know if you are infertile?
You should visit your doctor to undergo fertility testing. If you and your partner have just started trying to conceive, being checked is unnecessary yet—a basic gynecological exam which includes a pelvic ultrasound to dismiss the possibility of having some kind of uterine abnormality may be enough. Conversely, if you have been trying to conceive for 1 year without success, it is important for both of you to have your fertility checked.
Your gynecologist can answer all the questions you may have regarding female fertility, so our advice is that you do not hesitate to ask.
Is there a DIY female fertility test to check if I am fertile or not?
No, fertility tests for women can only be done in a gynecological clinic. There is only one over-the-counter test that can be done at home to predict the moment of ovulation: an Ovulation Predictor Kit (OPK). It should be clear that this test measures the LH surge that occurs when ovulation is about to happen. Yet, there is no possible way for you to make sure whether ovulation is occurring as it should or not unless you visit a fertility specialist.
What are signs of not being able to get pregnant?
Sometimes, infertility cannot be seen or felt through physical symptoms or signs. However, there are certain conditions that can lead to infertility and can be considered signs of female infertility, including but not limited to, endometriosis (which can cause tubal blockages), ovulation problems, painful periods, deep pain during intercourse, painful bowel motions, chronic pelvic pain, etc.
Nevertheless, the most obvious sign that a woman may be infertile is in fact the inability to get pregnant.
Check this post to learn more: Female infertility: definition, causes, signs and treatment.
Is the study of female fertility the same for all women?
Normally, the tests to assess female fertility are similar for most women. The first step is a gynaecological examination to assess the state of the ovaries and uterus, followed by a hormone analysis.
In this analysis the values of the hormones FSH, LH, oestradiol, AMH, prolactin and progesterone will be determined. It should be noted that the hormone analysis should be done on day 3-5 of the menstrual cycle, except for progesterone, which will be evaluated on day 21.
It is increasingly common to request a karyotype at the first consultation to assess whether there are genetic alterations that may be influencing the desired pregnancy.
Occasionally, it is necessary to perform additional tests such as hysterosalpingography to assess the patency of the fallopian tubes and hysteroscopy. There are also women who should undergo an endometrial biopsy if they have had previous unsuccessful cycles.
Suggested for you
If you want to learn more about fertility in men and women, we recommend that you have a look at the following guide: Male and female fertility.
On the other hand, if you are a woman, do not miss this: Guide to female fertility.
Also, this post gives you a complete overview on the most common fertility tests performed in couples when they visit the fertility specialist after 1 year trying to conceive without success. Want to learn more? Check this out: What fertility tests will I go through?
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
Al-Badawi IA, Fluker MR, Bebbington MW. Diagnostic laparoscopy in infertile women with normal hysterosalpingograms. J Reprod Med 1999; 44:953-7
Broekmans FJ, Kwee J, Hendriks DJ, Mol BW, Lambalk CB (2006). A systematic review of tests predicting ovarian reserve and IVF outcome. Hum Reprod Update; 12:685-718.
Bruna I, Sánchez de Rivera MD, Collado O. Protocolo de diagnóstico básico de la disfunción reproductiva. En: Diagnóstico y prevención de la disfunción reproductiva. Documentos de consenso SEGO, 2011, pp 71-89.
Crosignani PG, Rubin BL. ESHRE Capri Workshop Group. Optimal use of infertility diagnostic tests and treatments. Hum Reprod 2000; 15: 723-732.
Grupo de Interés de Centros de Reproducción Humana Asistida del Sistema Nacional de Salud (2002). Criterios para la utilización de los recursos del Sistema Nacional de Salud Español en técnicas de reproducción humana asistida Rev Iberoam Fertil; 19(1): 5-31.
Mol BW, Collins JA, Burrows EA, van der Veen F, Bossuyt PM. Comparison of hysterosalpingography and laparoscopy in predicting fertility outcome. Hum Reprod 1999;14:1237-42.
National Collaborating Center for Women’s and Children’s Health. Fertility: assessment and treatment for people with fertility problems. Clinical Guideline February 2004.
Pellerito JS, McCarthy SM, Doyle MB, Glickman MG, DeCherney AH. Diagnosis of uterine anomalies: relative accuracy of MR imaging, endovaginal sonography, and hysterosalpingography. Radiology 1992; 183:795-800.
Romero Guadix B, Martínez Navarro L, Arribas Mir L. Esterilidad: manejo desde la
consulta del médico de familia. AMF. 2002; 8 (6): 304-311.
Swart P, Mol BW, van der Veen F, van Beurden M, Redekop WK, Bossuyt PM. The accuracy of hysterosalpingography in the diagnosis of tubal pathology: a meta-analysis. Fertil Steril 1995;64: 486-91.
FAQs from users: 'What are the main female infertility tests?', 'How is a Hysterosalpingogram performed?', 'How much does a female fertility test cost?', 'How do you know if you are infertile?', 'Is there a DIY female fertility test to check if I am fertile or not?', 'What are signs of not being able to get pregnant?' and 'Is the study of female fertility the same for all women?'.
Authors and contributors





Hello, what fertility test for woman measures egg count? Is it done at doctor’s? I am interested in knowing this because i’m 35 already and planning to have a baby alone…
Dear muse,
A woman’s ovarian reserve, egg supply or egg count can be evaluated by assessing the levels of AMH (anti-müllerian hormone). This is done along with the analysis of other hormones, such as FSH, LH, progesterone, estradiol, etc. through a blood test. You can find all of them explained above.
Learn more about it here: Ovarian reserve test.
I hope I have been able to help,
Best wishes