Pelvic inflammatory diseases (PID) are inflammatory processes located in the upper part of the female genital tract such as the tubes, ovaries and uterus. In addition, these inflammatory processes can also affect other areas such as the ligaments.
These types of diseases usually occur in women between the ages of 15 and 39 and can be dangerous if not controlled in time. Therefore, an untreated PID can cause damage to the female reproductive organs and lead to various problems.
Provided below is an index with the 11 points we are going to expand on in this article.
- 1.
- 1.1.
- 1.2.
- 1.3.
- 1.4.
- 1.5.
- 2.
- 3.
- 4.
- 4.1.
- 5.
- 5.1.
- 5.2.
- 5.3.
- 6.
- 7.
- 8.
- 8.1.
- 8.2.
- 8.3.
- 8.4.
- 8.5.
- 9.
- 10.
- 11.
What types of PID are there?
Pelvic inflammatory disease (PID) refers to various inflammatory and infectious processes that occur in the upper female genital tract.
Depending on the area affected, PID includes several pathologies detailed below.
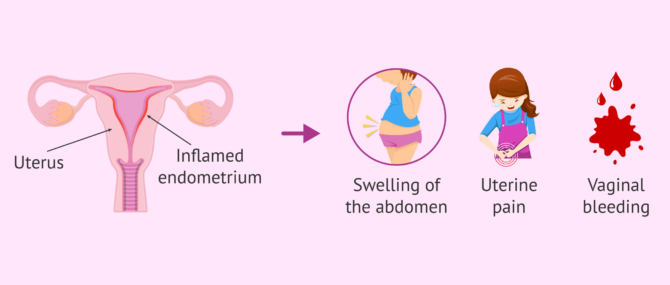
Endometritis
Endometritis is considered PID and consists of an inflammatory process or irritation of the endometrium. May be accompanied by other pelvic infections.
The etiologic agents that cause this disorder may be chlamydia, gonorrhea, tuberculosis, or a combination of normal vaginal bacteria.
Among the most prominent symptoms of endometritis are:
- Abdominal Swelling
- Abnormal vaginal bleeding
- Constipation
- Uterine pain
The condition usually goes away after antibiotics are given. It is also recommended to rest for a while.
Oophoritis
Oophoritis, also called ovaritis, is an inflammation of one or both ovaries. It usually appears between the ages of 25 and 35 and some risk factors are cancer, sexually transmitted infections, abortions, etc...
When the ovaries become inflamed, different symptoms appear, the intensity of which will vary according to each case.
This type of PID is caused by infection with Streptococcus, Staphylococcus, E. coli, and gonococci.
For more information continue reading here: Enlarged Ovaries: Symptoms and Treatment.
Myometritis
This is an infection of the uterine musculature that usually appears secondary to endometritis. It is also known as metritis.
Myometritis is usually associated with infection with the bacterium Arcanobacterium pyogenes. In addition, this infection may appear in combination with other pathogenic microorganisms such as Fusobacterium necrophorum, Bacteroides spp. and Escherichia coli.
Parametritis
Parametritis is considered a pelvic inflammatory disease because it leads to inflammation of the parametrium.
Parametrium is the set of structures that join the uterus to the pelvis. It consists of connective tissue and smooth muscle found within the broad ligament of the uterus.
This disease usually manifests itself after complicated abortions, childbirths, gynecological operations, or diseases of the uterus. It causes various symptoms such as fever, lower abdominal pain, or urinary problems.
Salpingitis
Salpingitis is one of the most common infectious diseases of the female genital organs. It consists of the inflammation of the fallopian tubes, causing sterility due to tubal alterations and increasing the possibilities of ectopic pregnancy.
The most common cause of inflammation of the fallopian tubes is a sexually transmitted infection (STI) in the genital area.
If you want to know more about salpingitis, you can read the following article: What is salpingitis? causes, symptoms, and treatment.
What are the causes of PID?
PID is often caused by the invasion of bacteria that ascend from the vagina and cervix to colonize other upper regions of the female genital tract.
Different physical changes appear in the internal organs and exudate forms that affects the mucous membrane. It is a pathology that can become chronic if adequate treatment is not established.
As for the etiology of PID, it is worth noting:
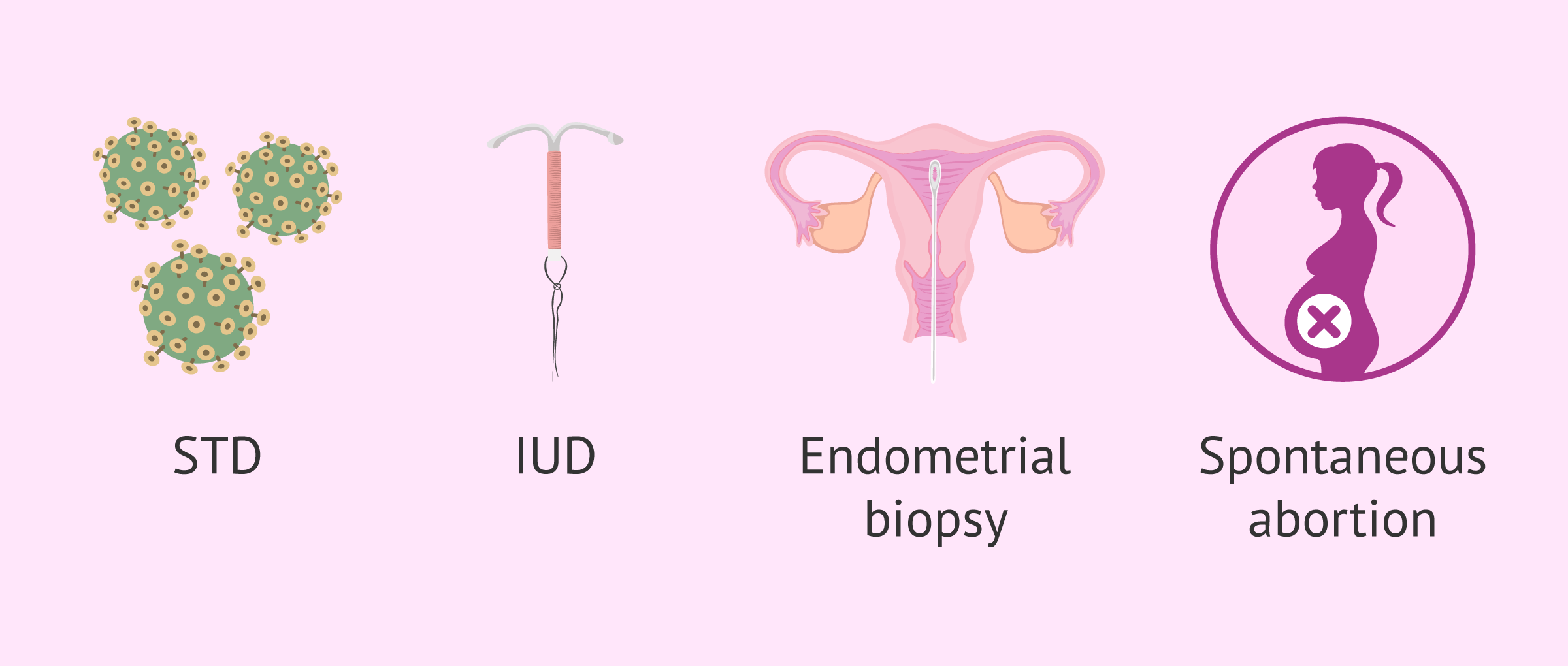
- Having sexual relationships with different partners and being under 25 years
- Sexually transmitted diseases (STDs). It is the most common cause and can occur from Chlamydia trachomatis, Neisseria gonorrhoeae and Mycoplasma hominis. It is therefore referred to as a polymicrobial infection.
- Changes in vaginal flora: alterations in vaginal flora caused by aerobic or anerobic pathogens, and also by the abuse of vaginal douches that damage the flora.
- Insertion of intrauterine devices (IUD), as they favor the presence of Actinomyces. The longer the IUD is used, the greater the risk of infection by this bacterium.
- Endometrial Biopsy, a procedure to obtain a small sample of tissue that surrounds the uterus.
- Voluntary interruption of pregnancy or miscarriage.
- Childbirth.
- Other infections such as those caused by Mycobacterium tuberculosis in relation to salpingitis, viruses, etc.
In addition, 20% of PID patients show no bacterial growth. This percentage corresponds to older women with subacute or chronic pelvic pain.
Symptoms and signs
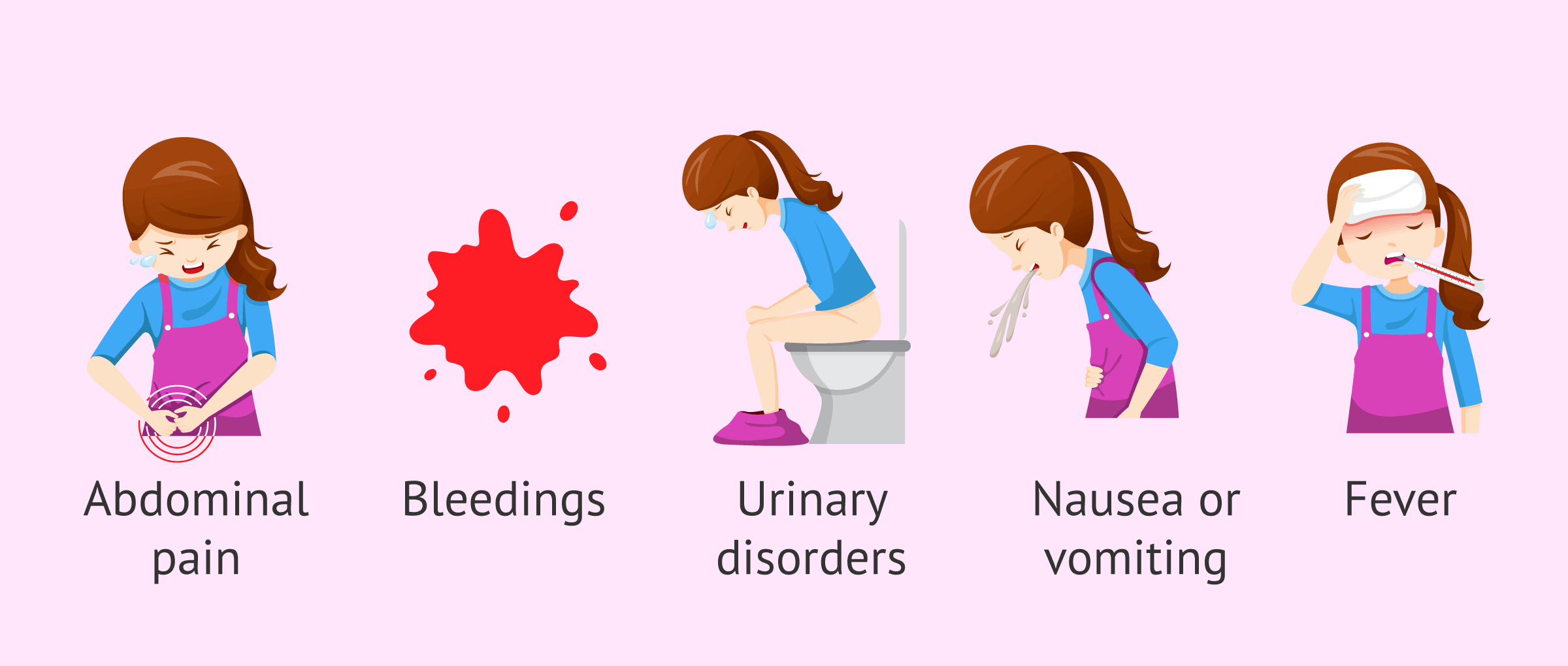
The way in which a PID can be presented is very varied. It appears from an asymptomatic process to even produce important alterations. Therefore, some of the common symptoms shown by patients with this disease are the following:
- Abdominal pain. It is the most common symptom in 95% of cases and usually appears in the lower part, in the hypogastrium.
- A change in vaginal discharge that causes an unpleasant color, consistency, or odor.
- Abnormal bleeding after sexual intercourse, intermenstrual bleeding, etc.
- Urinary disturbances such as pain when urinating or constant urge to urinate.
- Nausea and vomiting
- Other symptoms such as loss of appetite, tiredness, chills, etc.
On the other hand, the signs that define pelvic inflammatory disease and can be perceived by the doctor are:
- Pain on mobilization of the cervix.
- Excess vaginal discharge or leucorrhoea.
- Fever
- Tubal abscesses.
- Inflammation of the peritoneum or peritonitis.
The peritoneum is a connective tissue membrane that surrounds the abdominal viscera. It provides mobility to the organs located in the abdominal cavity, protects these organs from microorganisms, and acts as a thermal insulator.
How is PID diagnosed?
The diagnosis of PID is not very sensitive and specific. There is no single test to diagnose PID, but rather a fundamentally clinical diagnosis will be carried out, which will be complemented by various laboratory tests and other more specialized studies.
The most common tests for the diagnosis of PID are:
- Examination of the pelvis for signs of possible pelvic inflammatory disease.
- Blood count from a blood test that, if PID is present, shows elevated levels of leukocytes.
- Pelvic ultrasound to look for other possible causes of symptoms such as pregnancy or even appendicitis. Inflammation of the tubes and ovaries is also looked for.
- Cell culture to confirm the presence of harmful microorganisms on the cervix.
- Laparoscopy. This is the diagnostic test par excellence, although it has some limitations. It is very useful but the risks and the cost of its implementation must be taken into account.
- Endometrial biopsy that shows the presence of plasma cells and is indicative of PID.
If you want to become pregnant after PID, ultrasound and laparoscopy can help you find out if your fallopian tubes are blocked. The need for in vitro fertilization (IVF) or surgery to unblock the tubes will be assessed.
Classification
Depending on the diagnosis based on clinical features, PID can be classified into three different grades:
- Grade 1
- when the disease is not in a complicated phase and there are no signs of irritation and inflammation of the peritoneum.
- Grade 2
- the disease is already complicated and there are masses or abscesses in the ovaries and/or fallopian tubes. In addition, inflammation may be seen in the peritoneum.
- Grade 3
- spread of the infection to other structures outside the pelvis generating a systemic response.
Treatment for PIDs
The longer it takes to start PID treatment, the more injuries it can cause and the greater the likelihood of complications. In relation to this type of ailment, it is vitally important to go to a specialist doctor and make a good diagnosis that allows the most appropriate treatment to be established.
The objectives of treatment for PID are:
- To Eliminate infection.
- To relieve symptoms.
- To prevent complications
Treatment for milder PID will begin with a series of antibiotics. If the patient's medication doesn't go well or the treatment fails, intravenous treatment is given after hospitalization. In more severe cases of PID, surgery is used, although this is not common.
Antimicrobial
This type of outpatient treatment is indicated when uncomplicated or mild PID (grade I) is suspected. It consists of the administration of various antibiotics such as amoxicillin, cefotetan, quinolones, cephalosporin, and doxycycline.
The use of antibiotics eliminates the infection that causes inflammation in the upper part of the female reproductive system. Along with the administration of these drugs, it is advisable to follow prophylactic measures such as sexual hygiene measures or the use of condoms during sexual intercourse.
Hospitalization
When there is a failure, cannot be initiated or there is a poor tolerance to outpatient antibiotic treatment, the patient must be hospitalized. She will be given a series of intravenous antibiotics, as well as antipyretics for fever and pain relievers.
If she has an intrauterine device (IUD) implanted, her doctor will remove it once antibiotic treatment has begun.
Other cases of PID that also require hospitalization are shown below:
- Pregnant women.
- Women with grade II or III PID.
- Uncertain diagnosis between PID, ectopic pregnancy or appendicitis.
- History of uterine alterations.
In any case, it will be up to the specialist to determine whether it is necessary to admit the woman to the hospital or not.
Surgery
Surgical treatment is only indicated when all previous medical treatments have failed or serious complications occur. It is very rare for women with PID to require surgery.
However, if there is a risk that an abscess will rupture, her doctor will perform a drainage. A small needle is inserted through an incision in the skin and is performed under ultrasound control.
Complications arising from PID
The time to establish a treatment for PID is crucial to avoid sequela. However, there are a number of complications that can threaten the health of people with PID:
- Chronic pelvic pain.
- Infertility is one of the most important effects. It will make it difficult to get pregnant or causing difficulties during pregnancy.
- Ectopic pregnancy: alteration in the physiology of the fallopian tubes may interfere with the embryo's path to the uterus and may cause it to implant in an inappropriate location
- Recurrent infections.
- Increased preterm births and neonatal complications.
- Others such as Reiter's syndrome, reactive arthritis, etc.
The worst outcome of this pathology would be death, although it is not common. Antibiotics are usually given long before this point is reached.
Prevention
Measures to prevent PID are similar to those taken to prevent STDs. These measures are intended to prevent infection and its spread, as well as the possible sequela it may generate. However, it should be noted that this disease is not always caused by a sexually transmitted infection.
Primary prevention seeks to promote safe sex through sex education.
The use of barrier contraceptive methods (condoms), delaying the age at which sexual relations begin, reducing the number of partners, etc. should be promoted so that there is no risk of STD transmission.
Once PID is diagnosed in a woman, early treatment is established to prevent sequela and their spread. This would constitute secondary prevention.
Additionally, Douching kills bacteria that are normally found in the vagina. Their function is to prevent infections in the vagina. In addition, this practice encourages bacteria to travel to other areas of the female reproductive tract and may cause infections. For these reasons, douching is not recommended.
FAQs from users
Is it possible to become a mother after pelvic inflammatory disease (PID)?
Yes, however, the tubal disease can occur as a result of PID. This can make natural pregnancy more difficult and can also increase the risk of ectopic pregnancy.
Read more
How is pelvic inflammatory disease diagnosed?
Pelvic inflammatory disease is a pathology that is diagnosed by the presence of clinical compatible with it: fever, pelvic pain and the finding in the cervical culture or culture of endometrial aspirate bacteria that produce this pathology, such as gonococcus or chlamydia, among other things.
The most sensitive diagnostic test is laparoscopy, but in the vast majority of cases the diagnosis of pelvic inflammatory disease is made without having to resort to it. Blood tests are performed to determine the degree of infection, leukocytosis, as well as cultures with swabbing to detect bacteria that may cause this disease.
Is pelvic inflammatory disease the same as salpingitis?
Pelvic inflammatory disease (PID) refers to a group of infections and inflammations that occur in the upper area of a woman's genital tract.
Salpingitis is considered a type of chronic inflammatory disease because it is due to inflammation of the fallopian tubes.
Can I have sexual intercourse when diagnosed with PID?
Any sexual contact, even with a condom, should be avoided until the treatment is complete and does not show any sign of the pathology. This will prevent re-infection.
Who can get PID?
To some extent, any woman is vulnerable to PID. However, there are a number of risk factors that increase the likelihood.
Having sex with many people, sexually transmitted diseases, IUD insertion, miscarriages, endometrial biopsy, etc. are some of these risk factors.
Recommended readings
If you want more information about diseases that cause female infertility, you can read more here: Diseases that cause female infertility.
We also discussed sexually transmitted diseases throughout the article. For more information on STD's, have a look at: Sexually Transmitted Diseases (STDs) in men and women.
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
Brun, JL, Castan, B, Cazanave, C, Charvériat, A, Faure, K, Mignot, S, Verdon, R, Fritel, X, Graesslin O. [Pelvic Inflammatory Diseases: Updated Guidelines for Clinical Practice - Short version]. Gynecol Obstet Fertil Senol. 2019 Mar 14. pii: S2468-7189(19)30115-1. doi: 10.1016/j.gofs.2019.03.012. (see)
Cazanave, C, de Barbeyrac, B. [Pelvic inflammatory diseases: Microbiologic diagnosis - CNGOF and SPILF Pelvic Inflammatory Diseases Guidelines].Gynecol Obstet Fertil Senol. 2019 Mar 13. pii: S2468-7189(19)30110-2. doi: 10.1016/j.gofs.2019.03.007. (see)
Gremeau, AS, Girard, A, Lambert, C, Chauvet, P, Bourdel, N, Canis, M, Pouly, JL. Benefits of second-look laparoscopy in the management of pelvic inflammatory disease. J Gynecol Obstet Hum Reprod. 2019 Mar 22. pii: S2468-7847(18)30513-0. doi: 10.1016/j.jogoh.2019.03.020. (see)
Hernández, D, Diaz O. Enfermedad inflamatoria pélvica. Rev Cubana Obstet Ginecol v.36 n.4 oct.-dic. 2010. (see)
Martín-Lagos, A, Gallart, T, Porcel, MDC. Pelvic inflammatory disease: An unusual cause of acute intestinal obstruction.Gastroenterol Hepatol. 2019 Apr 11. pii: S0210-5705(19)30051-2. doi: 10.1016.
(see)
López A. Enfermedad Inflamatoria Pélvica: Tratamiento medico y quirúrgico. Revista Peruana de Ginecología y Obstetricia 2007; 53:240-247. (see)
Okong, P, Biryahwaho, B, Bergström, S. Post-abortion endometritis-myometritis and HIV infection. Int J STD AIDS. 2002 Nov;13(11):729-32. PMID: 12437891 DOI: 10.1258/095646202320753664 (see)
Verdon, R. [Treatment of uncomplicated pelvic inflammatory disease: CNGOF and SPILF Pelvic Inflammatory Diseases Guidelines]. Gynecol Obstet Fertil Senol. 2019 Mar 13. pii: S2468-7189(19)30111-4. doi: 10.1016/j.gofs.2019.03.008.
FAQs from users: 'Is it possible to become a mother after pelvic inflammatory disease (PID)?', 'How is pelvic inflammatory disease diagnosed?', 'Is pelvic inflammatory disease the same as salpingitis?', 'Can I have sexual intercourse when diagnosed with PID?' and 'Who can get PID?'.
Authors and contributors

More information about Cristina Algarra Goosman











What kind of specialist should be consulted? We had undergone an ICSI and it was unsuccessful. My wife started suffering cramps, pain in uterus, back pain, nausea… She spent about a month in hospital and had discharge with PID as a result after ICSI. Now what should I do? She has extreme pain in back and legs and has difficulty in walking.