The endometrium is the mucous layer that lines the uterus. Its function is to thicken during the menstrual cycle to allow the embryo to implant and pregnancy to occur.
At the beginning of each menstrual cycle, if pregnancy has not occurred, the endometrium sheds with menstruation to proliferate and renew itself again.
The role of the endometrium is very important in female fertility and it is also possible that it undergoes some alterations during the reproductive stage of the woman. Therefore, special care must be taken with all the factors that could affect the endometrium.
Provided below is an index with the 9 points we are going to expand on in this article.
- 1.
- 1.1.
- 2.
- 3.
- 4.
- 4.1.
- 4.2.
- 5.
- 6.
- 6.1.
- 6.2.
- 6.3.
- 6.4.
- 6.5.
- 6.6.
- 6.7.
- 6.8.
- 6.9.
- 6.10.
- 7.
- 8.
- 9.
What is the endometrium?
The endometrium is the innermost layer of the uterus, the most important reproductive organ where gestation takes place for 9 months.
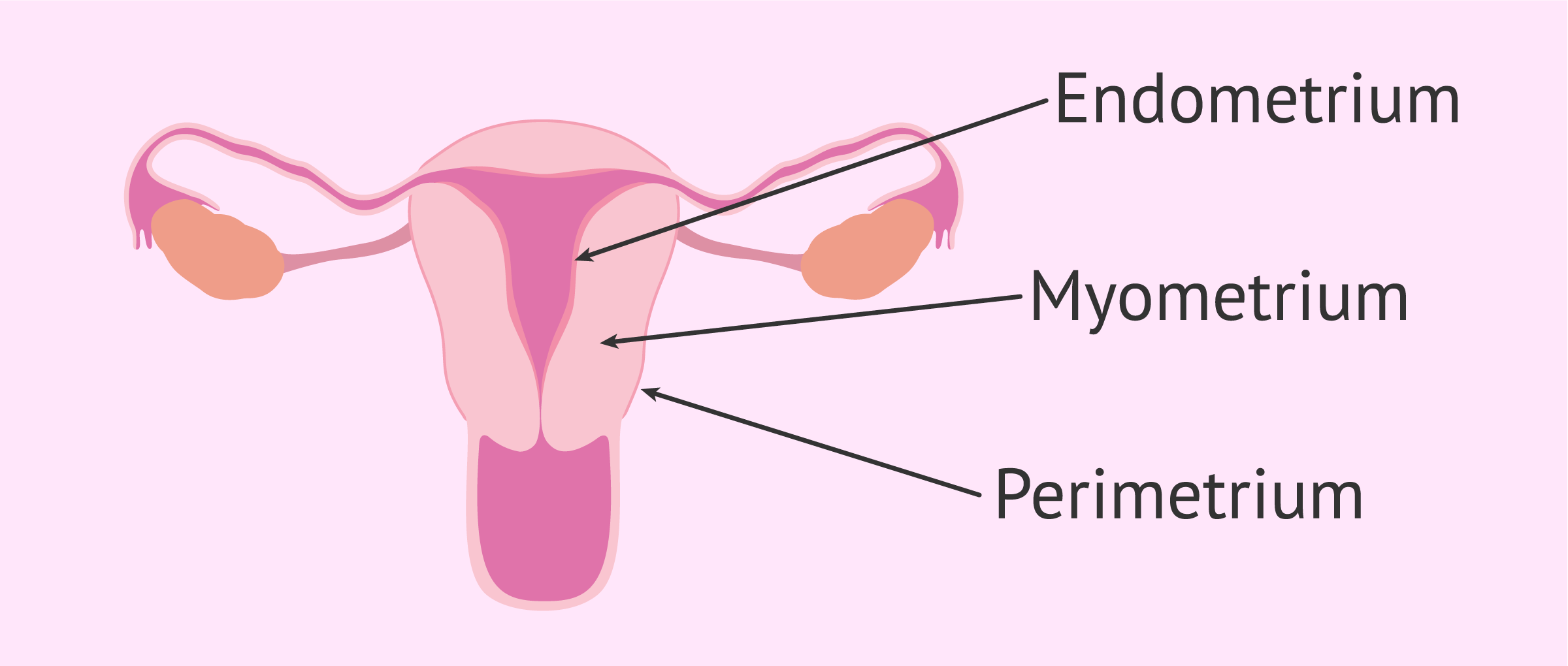
In order to better understand the function of the endometrium, in this section we describe the 3 uterine layers that exist:
- Outer or perimetrial layer
- is a serous layer that partially covers the uterus on the outside.
- Middle layer or myometrium
- is the muscular wall of the uterus. It has the ability to expand during pregnancy, to allow for the growth of the fetus, and to contract so that delivery can take place.
- Middle layer or myometrium
- It is the muscular wall of the uterus.
- Inner lining or endometrium
- is the mucous epithelium that lines the inner part of the uterus.
The main function of the endometrium is to allow the implantation of the embryo, that is, the union in the uterus so that the placenta, the gestational sac, and, finally, the umbilical cord through which the fetus will be connected to the mother can begin to develop.
In the words of Dr. Miguel Dolz:
The endometrium is an envelope that lines the inside of the uterus, which has a fundamental purpose in reproduction and that is to accept or allow the previously fertilized ovum to implant.
Composition of the endometrium
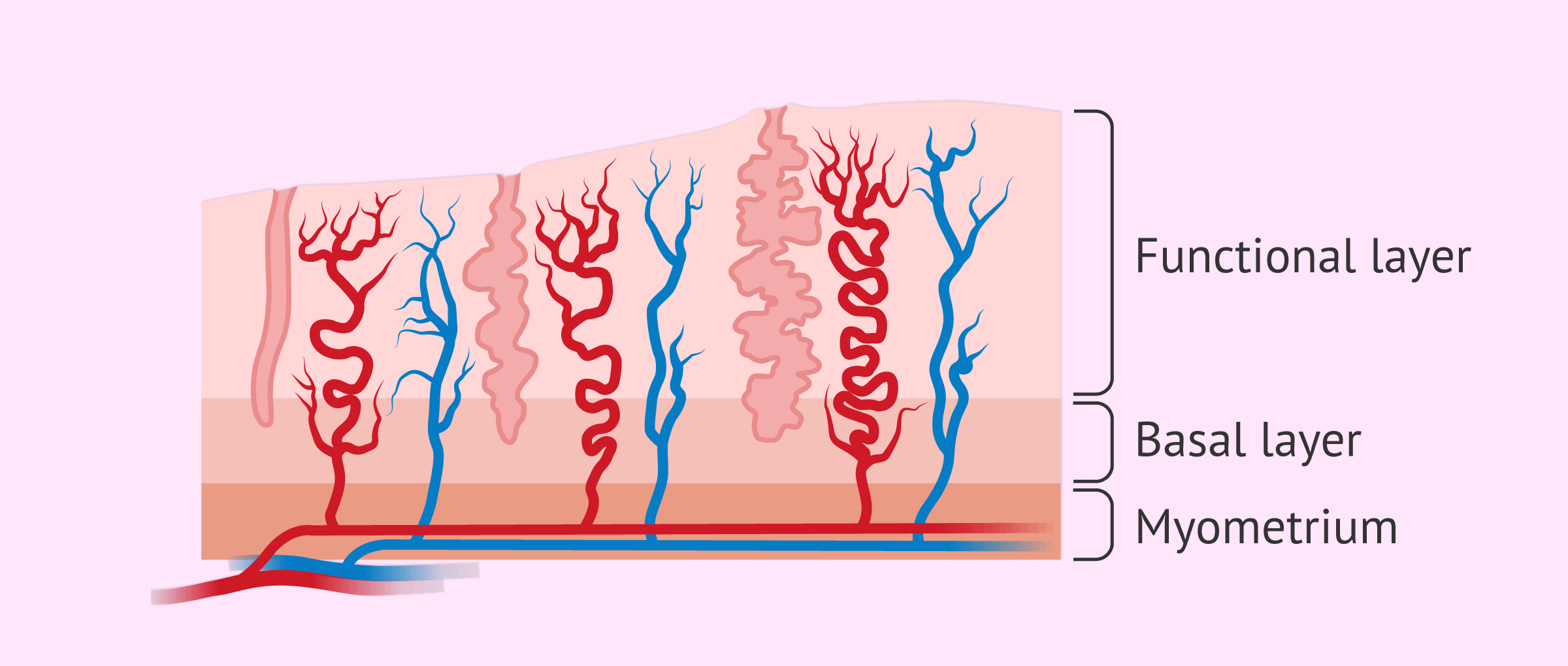
The endometrium is a highly vascularized tissue, regenerative in nature, which is made up of a multitude of blood vessels and glands that are formed and destroyed in each menstrual cycle.
The endometrium is also divided into two layers:
- Basal layer
- in it are the blood vessels and stem cells that generate the functional layer.
- Functional layer
- corresponds to the part of the endometrium that grows during the menstrual cycle and is eventually shed and expelled to the outside at menstruation.
If the egg is not fertilized or there is no implantation of the embryo in the uterus, the functional layer of the endometrium necroses and flakes off at the end of the menstrual cycle producing the bleeding known as menstruation.
This bleeding marks the beginning of a new menstrual cycle, in which the functional layer of the endometrium proliferates again thanks to the cells that exist in the basal layer.
Throughout the menstrual cycle, the endometrium undergoes both morphological and functional modifications, thanks to the function exerted by the sex hormones secreted by the ovaries. These hormones are estrogens and progesterone.
Thickening in the menstrual cycle
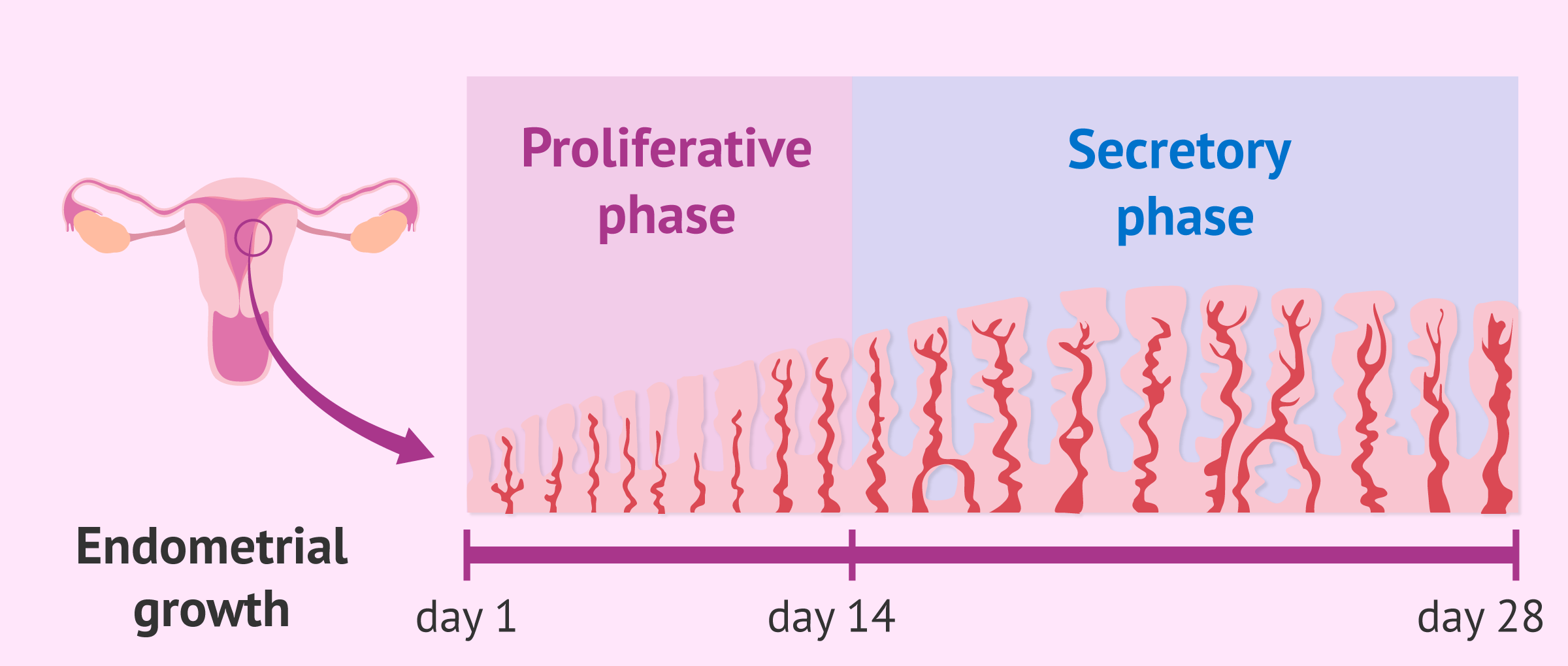
Two main types of endometrium can be distinguished according to the timing of the menstrual cycle:
- Proliferative endometrium
- Thanks to estrogen production, the functional layer of the endometrium begins to grow by multiplication of the cells of the basal layer. More blood vessels and endometrial glands appear. The proliferative phase spans from the first day of the menstrual cycle until ovulation.
- Secretory endometrium
- After ovulation, the corpus luteum remaining in the ovary produces progesterone, which causes the endometrium to mature, causing it to thicken. The endometrial glands increase in size and begin to secrete mucus and a substance rich in glycogen. Thus, the ideal environment for implantation is created.
At the end of the secretory phase of the menstrual cycle, around days 26-28, endometrial shedding occurs if implantation has not occurred, which causes the period to drop.
Parallel to menstruation, a new endometrium is regenerating for the next ovulation. This is why menstruation coincides with the beginning of the proliferative phase of a new menstrual cycle.
If you want to know in more detail the phases of the menstrual cycle in women, we recommend you visit the following post: Phases of the menstrual cycle.
Implantation in the endometrium
Nesting of the embryo in the endometrium occurs when about 6 to 7 days have passed since fertilization and the embryo is at the blastocyst stage.
For this to occur, there must be a perfect synchronization between the embryo and the endometrium, that is, there must be endometrial receptivity.
The endometrium is receptive during the phase known as implantation window, which lasts approximately 4 days.
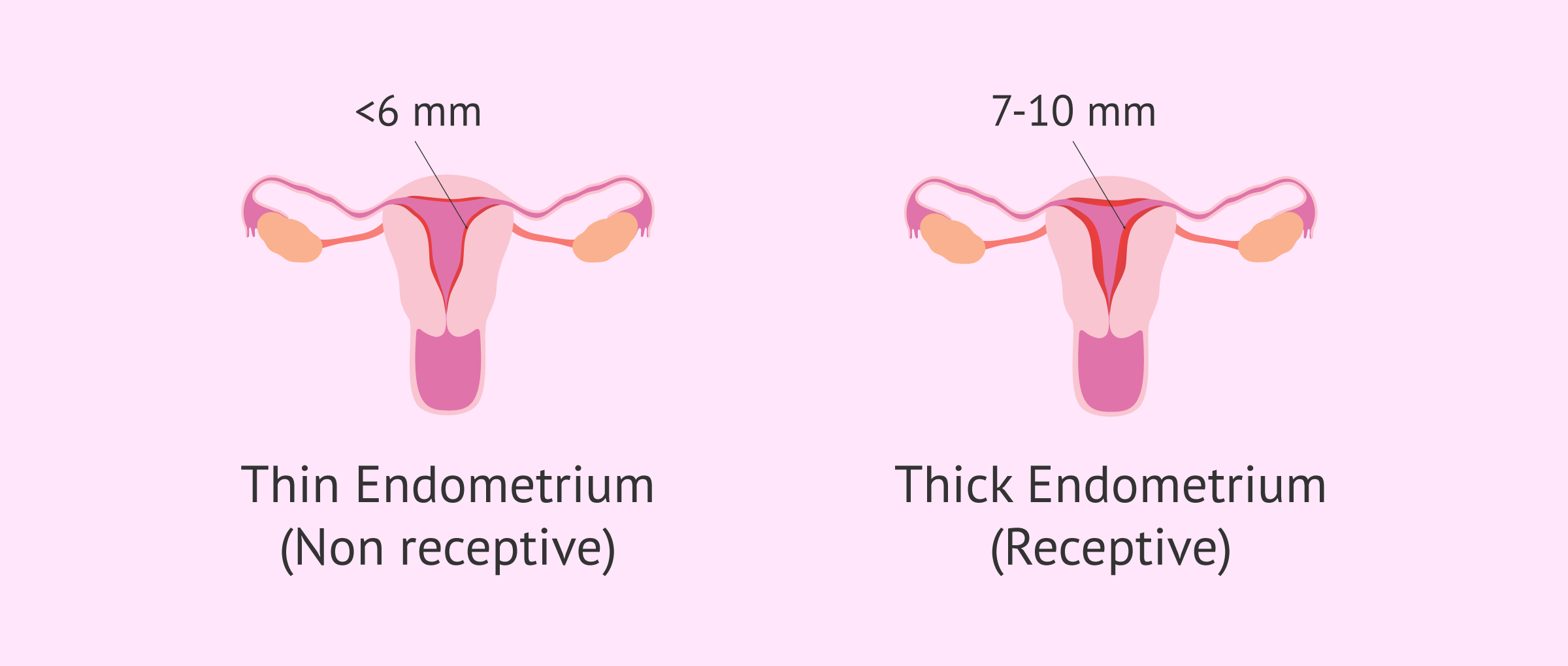
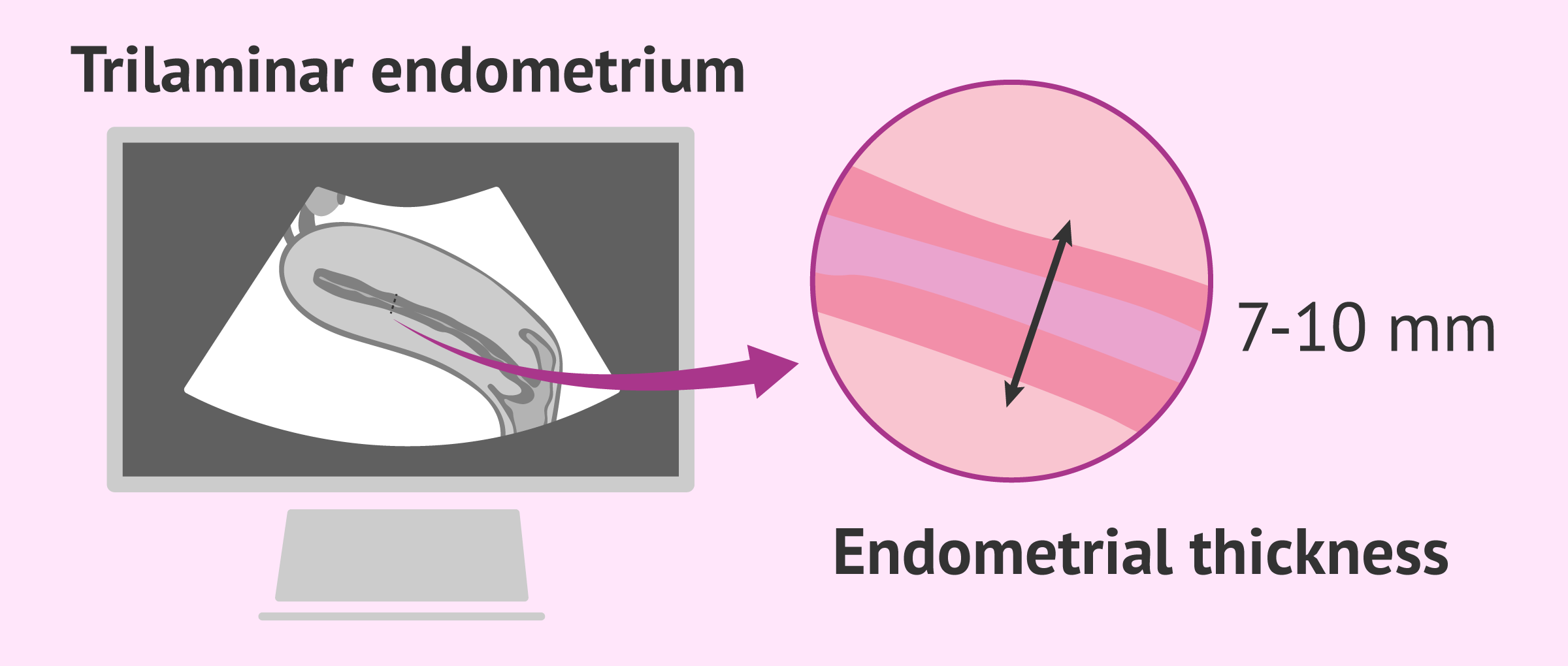
Numerous studies in patients have concluded that the optimal endometrial thickness for implantation to take place should be between 7-10 mm thick. An endometrium of less than 6 mm does not usually allow embryos to implant.
For successful implantation, not only must there be adequate hormonal preparation of the endometrium, but there must also be a reciprocal dialogue between the blastocyst tissues and the uterine mucosa. For this, various growth factors and cytokines must act.
If fertilization of the egg and implantation of the embryo has finally taken place, the secretory endometrium becomes a more specialized endometrium thanks to the effect of estrogens and progesterone: this is known as decidualization.
The decidual or decidualized endometrium consists of a specialized structure that will give rise to the placenta during gestation and will participate in the exchange of gases and nutrients between the mother and the embryo.
To learn more about embryo implantation, you can access this article: What is embryo implantation?
Endometrial assessment
Endometrial thickness is a prognostic factor in predicting embryo implantation.
In addition, measuring endometrial thickness can also provide information about some pathologies or alterations in the endometrium.
The following tests are useful for measuring endometrial thickness, as well as endometrial receptivity:
Transvaginal ultrasound
Endometrial thickness is a marker of the phases of the menstrual cycle.
To consider whether the endometrium is normal, it must have a specific thickness depending on the day of the menstrual cycle in which the woman is.
To measure endometrial thickness, gynecologists perform a transvaginal ultrasound. Subsequently, they must assess whether this thickness coincides with the date of the last menstrual period (LMP) indicated by the patient.
With ultrasonography, it is possible to differentiate the following types of the endometrium:
- Type 0 endometrium
- during the menstrual phase, the endometrium is hyperechogenic, i.e., it is seen as a thin, faint white line <5 mm.
- Type I endometrium
- presents a trilamellar pattern, that is, the appearance of three lines parallel to each other, although the inner line is not well distinguishable. It is observed in the proliferative phase.
- Type II endometrium
- the endometrium is clearly trilaminar, the three lines are perfectly distinguishable. The endometrium can measure between 7 and 10 mm. It is observed in the proliferative phase shortly before ovulation, due to the strong influence of estrogens.
- Type III endometrium
- It is seen in the luteal phase of the cycle, so the endometrium is in the secretory phase under the influence of progesterone, and is ecorefringent (homogeneous). The endometrium is thickened, has fluid content and glycoprotein material in the endometrial glands.
Additional techniques
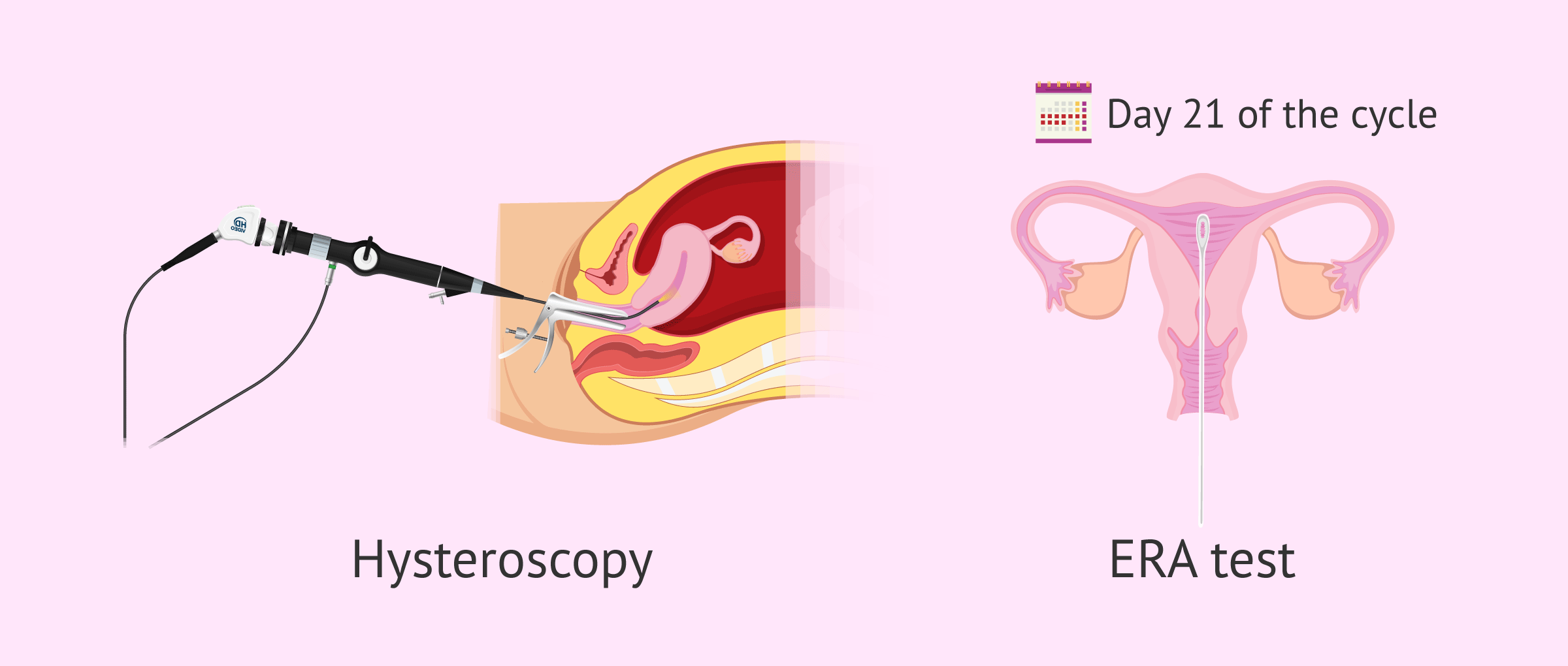
If transvaginal ultrasound is not sufficient to assess endometrial structure and thickness, or if further analysis is necessary in order to determine endometrial receptivity, the following techniques may be used:
- Hysteroscopy
- to assess endometrial quality and act on pathology, if present.
- ERA (endometrial receptivity array)
- to detect the presence of genes involved in endometrial receptivity, which allows knowing if the endometrium is receptive at a particular time and if it is able to implant embryos.
The ERA test is used especially in in-vitro fertilization (IVF) patients with implantation failure, which allows knowing if there is a displacement in the window of implantation.
The solution to this problem is to vitrify the embryos and then transfer them to the uterus when the endometrium is receptive.
Assisted procreation, as any other medical treatment, requires that you rely on the professionalism of the doctors and staff of the clinic you choose. Obviously, each clinic is different. Get now your Fertility Report, which will select several clinics for you out of the pool of clinics that meet our strict quality criteria. Moreover, it will offer you a comparison between the fees and conditions each clinic offers in order for you to make a well informed choice.
If you are interested in receiving more information on this topic, you can continue reading in the following post: Endometrial receptivity test.
Endometrial pathologies and diseases
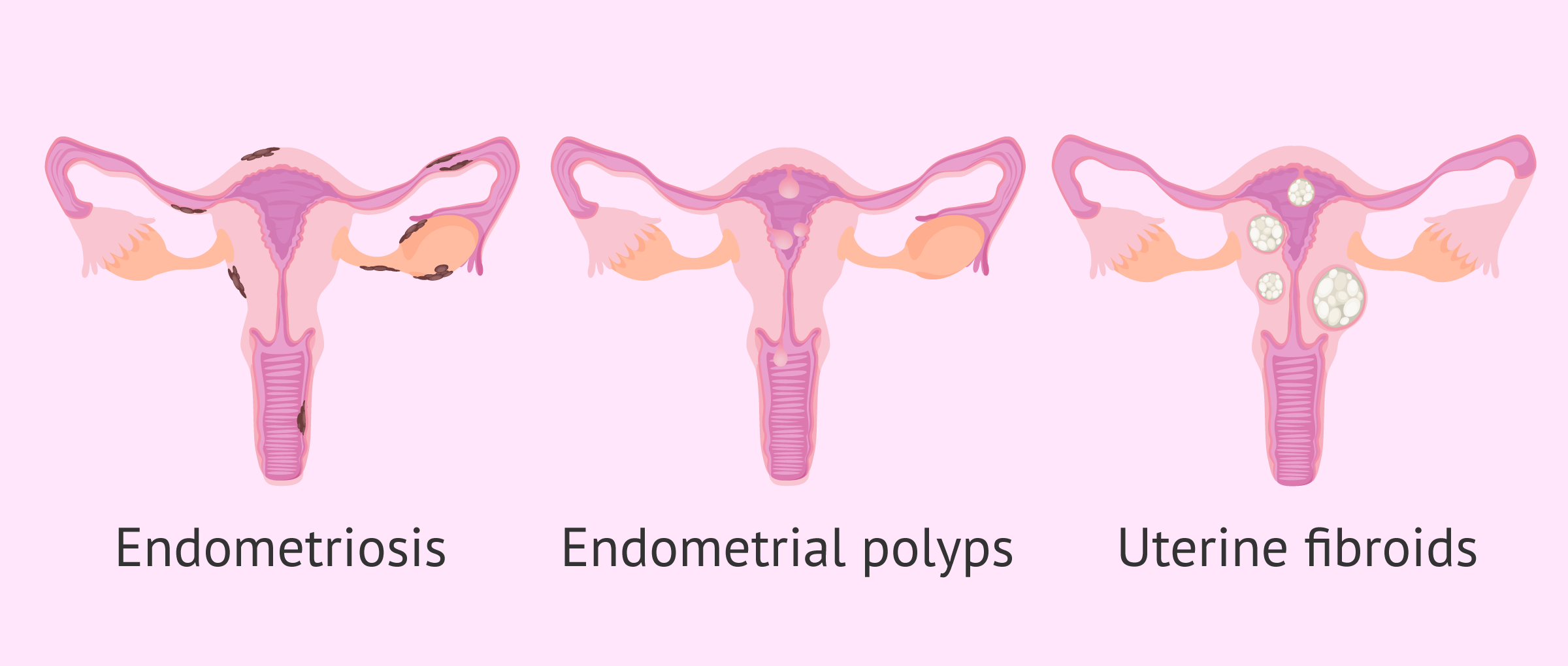
Endometrial disorders can affect embryo implantation and menstrual bleeding in women.
Therefore, any abnormal sign during the period may lead a woman to suspect one of the following endometrial pathologies:
- Endometriosis
- growth of endometrial tissue outside the uterine cavity, such as in the ovaries, fallopian tubes, pelvic cavity or even in the bladder. It usually causes a lot of pain during menstruation and affects fertility.
- Edometrial polyps
- tissue protruding from the endometrium and containing abundant blood vessels and endometrial glands. They can cause metrorrhagia and affect embryo implantation.
- Uterine myoma
- Benign tumor arising from the myometrium. Submucosal fibroids grow into the uterine cavity and affect the endometrium. Although submucosal fibroids are the least common, they cause increased bleeding and are at risk of becoming malignant.
- Adenomyosis
- invasion of endometrial tissue into the muscular layer of the uterus, the myometrium. Adenomyosis causes alterations in bleeding and pain.
- Edometrial hyperplasia
- proliferation of glands in the endometrial mucosa.
- Edometrial hypertrophy
- excessive thickening or increase in endometrial thickness.
- Edometrial cancer, endometrial neoplasia or adenocarcinoma
- growth of malignant cells in the endometrial tissue. It is the most common type of uterine cancer.
When we encounter symptoms such as abnormal uterine bleeding, it can be any of these alterations: myomas, endometrial polyps, adenomyosis, endometrial hyperplasia, or endometrial cancer.
To diagnose diseases affecting the endometrium, ultrasound may not be sufficient. The gynecologist may request complementary tests such as the following: a uterine bleeding, an endometrial biopsy, a sonohysterography or a hysteroscopy depending on the pathology suspected.
FAQs from users
What are the consequences of refractory endometrium?
We speak of refractory endometrium when, in spite of a correct endometrial preparation, this endometrium does not acquire the size and thickness necessary to have a good guarantee of pregnancy.
In these cases the implantation rate, the clinical gestation rate and the live birth rate are reduced. An increase in the rate of miscarriage has not been observed.
When faced with a woman with a refractory endometrium, we must take two approaches. First, perform a hysteroscopy to try to find the cause of the endometrium not growing sufficiently and correct it.
On the other hand, changing the endometrial preparation strategy can also be of great help. Not all endometria respond equally to all estrogens. Some endometrium responds better to a different route of administration (for example, changing the patches for pills), or to a higher dose of estrogens (increasing the dose always within the safe doses), or to the estrogens specific to the woman's cycle (using the natural ovarian cycle instead of giving estrogens externally), etc.
Which uterine layer corresponds to the endometrium?
The endometrium is a mucous layer that lines the inside of the uterus. It is the layer that is shed with each menstrual period in the different cycles and is the layer that embraces the embryo when gestation occurs.
What is the optimal size of the endometrium for pregnancy to occur?
Optimal endometrial size is assessed by measuring endometrial thickness, which is the most commonly evaluated parameter. The imaging method of choice is transvaginal ultrasound.
The optimal endometrium prior to embryo transfer is the so-called trilaminar, triple line or "coffee bean" endometrium, typical of the advanced follicular phase. It is formed by two outer hyperechogenic lines that represent the junction between the basal endometrium and the myometrium; two hypoechoic bands that are the functional layer of the endometrium; and, finally, a central hyperechogenic line, the lumen of the cavity.
The literature suggests that the normal range of endometrial thickness would be 6 mm at the lower limit and 20 mm at the upper limit. Implantation is unlikely outside these ranges. A thickness between 7 and 9 mm at periovulatory time is considered ideal in the literature; however, reasonable pregnancy rates are also achieved with endometrial thicknesses of 6 mm.
If the endometrium is thickened, is there pregnancy or is it because menstruation is coming?
The endometrium thickens so that implantation and pregnancy can take place. If there is no fertilization and implantation, even if the endometrium is thickened, there will be no pregnancy and menstruation will occur.
If the endometrium is still thick after some time or if it is excessively thick in the secretory phase, it may be endometrial hyperplasia and the doctor may prescribe hormonal treatment for the woman.
How thick does the endometrium have to be to become pregnant?
The normal thickness of the endometrium after ovulation, when implantation takes place, is 7-10 mm. If the endometrium is too thin or too thick, implantation may be hindered or prevented, as the endometrium is not receptive and therefore pregnancy may not occur.
What causes the endometrium to be thick?
The endometrium thickens naturally due to the action of estrogen and progesterone, two hormones produced by a woman's ovaries during the menstrual cycle.
An excessively thick endometrium may be due to endometrial hyperplasia. This abnormality is usually caused by an excessive production of estrogen but hardly any progesterone is produced. If this condition is present, the physician may administer hormone therapy.
With a thin endometrium can pregnancy be achieved? How can it be thickened?
If the endometrium measures less than 6 mm, it will be difficult to achieve pregnancy. In such a case, the doctor may prescribe a hormonal medication based on estrogen and progesterone to stimulate the growth of the endometrium.
There are also natural therapies and strategies that women can use on a daily basis to improve their endometrial thickness.
Is it normal to have a thick endometrium in menopause?
Generally, with the onset of menopause there is endometrial atrophy, i.e. a thinning of the endometrium due to the natural decrease in estrogen levels. At menopause estrogens are no longer produced and therefore there is no menstrual cycle.
If, on the other hand, the endometrium is thick, the physician must determine whether it is endometrial hyperplasia or another pathology.
What is endometrial carcinoma and what are its symptoms?
Endometrial carcinoma is a common type of cancer in women, especially in those who have entered menopause. It consists of the growth of malignant cells in the endometrial tissue of the uterus. The most frequent symptoms are abnormal vaginal bleeding not associated with menstruation, pelvic pain, and discomfort when urinating or having sexual intercourse.
As in all types of tumors, a rapid diagnosis of endometrial cancer is essential for its treatment to be effective and for there to be no invasion of other parts of the body.
What is endometrial atrophy?
Endometrial atrophy consists of thinning of the endometrium. The endometrium becomes thinner and more fragile. This usually occurs once menopause is reached as a result of a decrease in estrogen levels in women.
However, the onset of menopause is not the only cause of endometrial atrophy. Some patients may also have a thin endometrium due to medical induction or the presence of certain pathologies such as polycystic ovarian syndrome, pituitary alterations, etc.
One of the problems that can be caused by endometrial atrophy is the difficulty in achieving pregnancy in women of childbearing potential. This is due to the fact that if the endometrium does not acquire adequate thickness, the embryo will not be able to implant and, therefore, gestation will not take place.
Recommended reading
A displacement of the implantation window in the endometrium is a cause of embryo implantation failure. If you want to know other factors that can affect implantation, you can continue reading in the following article: Repeated embryo implantation failures.
There are more pathologies related to the uterus, in addition to those affecting the endometrium. You can learn more about this in the following post: Female infertility due to uterine factor.
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
Dody Houston Billhaq, Sang-Hee Lee, Seunghyung Lee. The potential function of endometrial-secreted factors for endometrium remodeling during the estrous cycle. Anim Sci J. Jan-Dec 2020;91(1):e13333. doi: 10.1111/asj.13333 (View)
Giuseppe Benagiano, Ivo Brosens. The endometrium in adenomyosis. Womens Health (Lond). 2012 May;8(3):301-12. doi: 10.2217/whe.12.8 (View)
Levent M Senturk, C Tamer Erel. Thin endometrium in assisted reproductive technology. Curr Opin Obstet Gynecol. 2008 Jun;20(3):221-8. doi: 10.1097/GCO.0b013e328302143c (View)
M K Oehler 1, M C Rees, R Bicknell. Steroids and the endometrium. Curr Med Chem. 2000 May;7(5):543-60. doi: 10.2174/0929867003374958 (View)
Murat Ulukus, Hakan Cakmak, Aydin Arici. The role of endometrium in endometriosis. J Soc Gynecol Investig. 2006 Oct;13(7):467-76. doi: 10.1016/j.jsgi.2006.07.005 (View)
Nehalennia van Hanegem, Marileen M C Prins, Marlies Y Bongers, Brent C Opmeer, Daljit Singh Sahota, Ben Willem J Mol, Anne Timmermans. The accuracy of endometrial sampling in women with postmenopausal bleeding: a systematic review and meta-analysis. Eur J Obstet Gynecol Reprod Biol. 2016 Feb;197:147-55. doi: 10.1016/j.ejogrb.2015.12.008 (View)
Ting Jiang, Qing Yuan, Qin Zhou, Yiping Zhu, Siji Lv, Yanling Cao, Qin Wang, Kunming Li, Dong Zhao. Do endometrial lesions require removal? A retrospective study. BMC Womens Health. 2019 May 6;19(1):61. doi: 10.1186/s12905-019-0756-8 (View)
Wendy Wolfman, Nicholas Leyland, Mark Heywood, Sukhbir S Singh, David Allan Rittenberg, Renée Soucy, Catherine Allaire, Alaa Awadalla, Carolyn Best, Sheila Dunn, Nathalie Leroux, Frank Potestio, Vyta Senikas, Sarah Wallace, Rebecca Menzies, Society of Obstetricians and Gynaecologists of Canada. Asymptomatic endometrial thickening. J Obstet Gynaecol Can. 2010 Oct;32(10):990-9 (View)
FAQs from users: 'What are the consequences of refractory endometrium?', 'Which uterine layer corresponds to the endometrium?', 'What is the optimal size of the endometrium for pregnancy to occur?', 'If the endometrium is thickened, is there pregnancy or is it because menstruation is coming?', 'How thick does the endometrium have to be to become pregnant?', 'What causes the endometrium to be thick?', 'With a thin endometrium can pregnancy be achieved? How can it be thickened?', 'Is it normal to have a thick endometrium in menopause?', 'What is endometrial carcinoma and what are its symptoms?' and 'What is endometrial atrophy?'.
Authors and contributors

More information about Cristina Algarra Goosman






Hi, I am waiting to have IVF done but the doctor has told me that my endometrium measures 20mm and that we should wait for the next cycle, it measures much more than what you explain in the article as normal. I am worried that it is not within the parameters, what can I do?
Hi sarah435,
Indeed the thickness of your endometrium is much higher than average or recommended for good implantation after the transfer. If the doctor has recommended that you wait until the next cycle, it is because the endometrium changes, sheds and thickens again cycle after cycle.
I recommend that you wait to see how thick the endometrium becomes towards the middle of your cycle and that your doctor assesses whether it has decreased or if any treatment such as curettage is necessary.
I hope I have helped you.
Best regards.
Oh my goodness! Incredible article dude! Thank you so much, However I am experiencing troubles with your RSS. I don’t understand why I am unable to join it. Is there anyone else getting identical RSS problems? Anyone who knows the answer can you kindly respond? Thanks!!