Polycystic Ovary Syndrome or Polycystic Ovarian Syndrome (PCOS), also known as Stein-Leventhal Syndrome, is a common endocrine disorder that can affect female fertility severely.
The symptoms of PCOS are varied and often undetectable until the woman visits her doctor because she has been able to get pregnant despite having tried to conceive for a long time. For this reason, some women with PCOS require a fertility treatment to have a baby.
Provided below is an index with the 9 points we are going to expand on in this article.
- 1.
- 2.
- 3.
- 4.
- 5.
- 6.
- 6.1.
- 6.2.
- 6.3.
- 6.4.
- 6.5.
- 7.
- 8.
- 9.
Definition
Polycystic Ovary Syndrome (PCOS) is the most common endocrine disorder in women of childbearing age, affecting 4-8% of them. It is often associated with:1ß
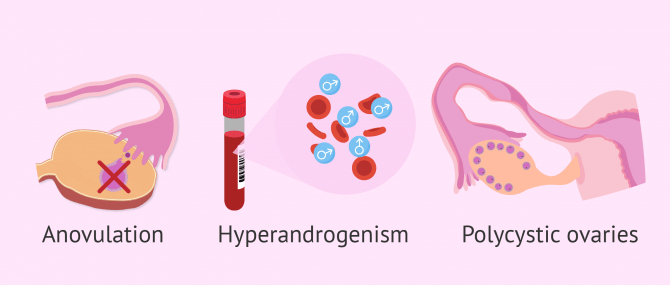
- Anovulation (absent ovulation) and subsequent sterility. In fact, it is the most frequent cause of anovulatory infertility
- Obesity
- Hyperandrogenism (excessive amount of male hormones)
- Insulin resistance
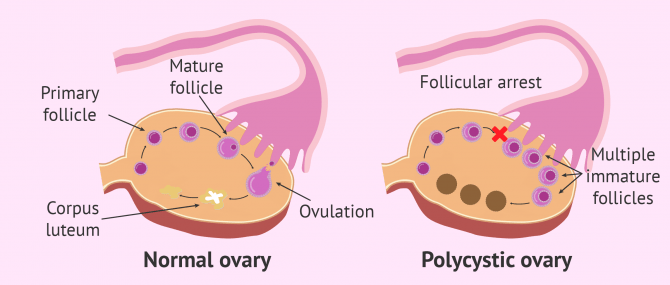
Women with PCOS produce higher amounts of androgens than normal, and therefore the menstrual cycle is not regulated correctly. The ovary fails to release eggs because they do not mature, causing cysts. Due to this absent maturation and egg release process, women with PCOS have infertility problems.
Fertility treatments, like any other medical treatment, require that you trust the fertility specialists that will be by your side during your journey. Logically, each clinic has a different work methodology. Our Fertility Report will offer you a selection of recommended clinics, that is, fertility centers that have passed our rigorous selection process. Moreover, our system is capable of comparing the costs and conditions of each one so that you can make a well-informed decision.
PCOS is due to metabolic causes, and it should not be be confused with polycystic ovaries or PCO, which are due to an alteration within the ovarian function, in which follicles are not fully mature and, therefore, they do not release the egg. Follicles then turn into a cyst within the ovarian cortex, which appears thickened in the ultrasound.
Between 16 and 25 percent of women of childbearing age have polycystic ovaries, which does not mean they have PCOS by default. In other words, having polycystic ovaries does not automatically translate into PCOS.
The causes of PCOS are still unclear, although there seems to have a genetic origin. In fact, some studies suggest the involvement of several genes. Most experts consider that it is due to multiple factors, with influence of both genetic and environmental aspects.
Diagnosis
Ever since PCOS was described for the first time, the diagnostic criteria used have changed as more information on this syndrome have been discovered.
Presently, the Rotterdam criteria are the most commonly used to diagnose a woman with PCOS. According to them, in order for PCOS to be diagnosed, it is necessary for the patient to present at least two of these symptoms after having dismissed other pathologies:
- Oligoovulation or anovluation: the patient ovulates less frequently than normal or ovulation is absent.
- Clinical or biochemical signs of hyperandrogenism
- Ultrasound scan shows polycystic ovaries: twelve or more follicles of between 2 and 9 cm in corona radiata shape or with an enlarged ovarian volume (over 10 ml) in one or both ovaries are found.
You may also enjoy some further information reading this: How Is PCOS Diagnosed?
Symptoms
Women suffering from PCOS usually experience the following clinical signs:
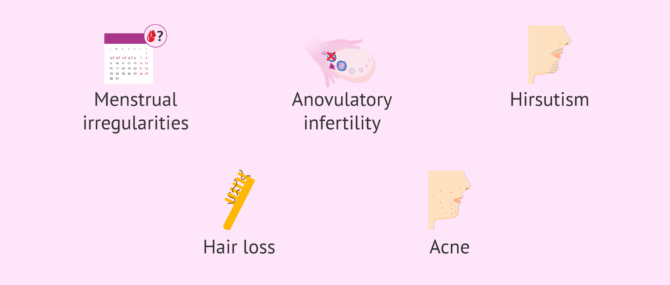
- Menstrual irregularities: oligomenorrhea (less than 9 menses per year) or amenorrhoea (absent menstrual period)
- Anovulatory infertility
- Hirsutism or excessive amounts of dark, course hair
- Alopecia or hair loss
- Acne
- Hormonal disorders: elevated testosterone levels, high LH levels, elevated LH/FSH relationship, elevated δ4-androstendione (androgen) levels, etc.
- Increased AMG (anti Müllerian hormone) levels
- Insulin resistance
- Polycystic ovaries
- Breast and uterine hypoplasia
- Obesity.
- Acanthosis nigricans: dark patches of skin which usually appear on the neck or the armpits.
The signs and symptoms of PCOS are often aggravated in women with a higher than normal body mass index (BMI).
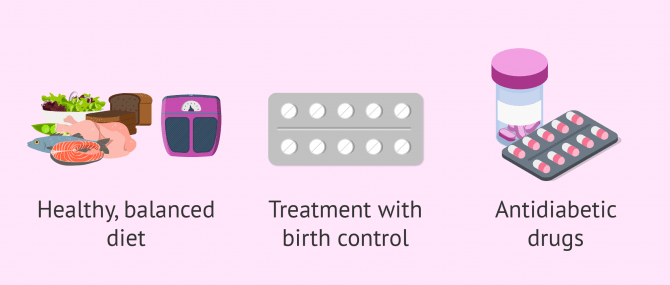
Treatment
In cases of predisposition to develop PCOS, changing your lifestyle and following a balanced diet are essential steps against it. Having a BMI-number below 25 and taking contraceptives and antidiabetic drugs is highly advisable, too. It is not only fundamental to avoid obesity but rather a sedentary lifestyle.
Metformin, an antidiabetic drug, has been widely used for the desensitization of the ovaries towards excess insulin, this way promoting follicular development.
In case these women wish to have children, especially in obese women, the first step to making this dream come true will be to establish healthier lifestyle habits. If this is not enough, or if losing weight is not necessary, ovulation will be induced artificially with fertility drugs such as Clomid.
When these strategies fail, patients have no alternative but to turn to Assisted Reproductive Technology (ART). In some cases, undergoing just an IUI works, but in other cases, the patient might require In Vitro Fertilization (IVF) to achieve pregnancy.
Related content: Treatment Options for PCOS.
Effects
As Dr. Miguel Ángel Vincenti Bosco explains, PCOS is one of the most common endocrine disorders in females. In fact, it is present in 4 to 8 percent of women who visit a fertility clinic. PCOS disease has important consequences on the woman affected from the obstetric, metabolic, and psychological viewpoints.
From the obstetric point of view, it increases the number of risks during pregnancy. For example, these patients are more likely to have recurrent miscarriage or develop a disease such as toxemia of pregnancy (gestosis), diabetes or high blood pressure during pregnancy, Dr. Vincenti Bosco states.
As for the metabolic effects, PCOS patients are usually women with a BMI that is higher than normal, in some cases with morbid obesity. Also, these women typically have hirsutism, increased body hair in places that are more common in males, insulin resistance, and hyperandrogenism.
FAQs from users
What are my chances of getting pregnant with IUI if I have PCOS?
The success rates of Intrauterine Insemination (IUI) depend on the type of insemination (by husband or by donor), the age of the woman, and the problem she has. On average, success rates range from 14% to 20% per cycle.
Can PCOS be cured?
The fact that there are genetic factors involved makes it more difficult for this disorder to be cured. However, it can be prevented or its symptoms diminished if the woman leads a healthy lifestyle and controls her diet.
Can metformin help you get pregnant with PCOS?
Metformin can help to resume ovulation cycles, achieving normal cycles in obese patients with insulin resistance. Nonetheless, if this is the only drug administered, the clinical success rates do not seem to increase. Metformin just seems to provide a series of benefits for women with PCOS who are trying to get pregnant and are using clomiphene citrate as well, such as Clomid.
Does PCOS run in the family?
No. Polycystic ovary syndrome (PCOS) is an endocrine disorder whose cause is unknown. It is true that there is a genetic predisposition and there are several genes involved,
However, according to the latest studies, PCOS has a multifactorial origin where both genetic and environmental factors intervene.
What treatment options can help you get pregnant with PCOS?
The best treatment option depends on the results of your hormone analyses and the gynecological examination. Firstly, you can try with a change in lifestyle habits, which can be helpful to regulate the menstrual cycle. If this does not work to overcome anovulation, you may be prescribed a series of drugs to induce ovulation. Finally, if none of these treatment options work, you may be required to undergo a fertility treatment, such as IUI or IVF, if needed.
Suggested for you
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
Adams Hillard PJ. Oral contraceptives and the management of hyperandrogenism - polycystic ovary syndrome in adolescents. Endocrinol Metab Clin N Am 2005; 34:677-705.
Asunción M, Calvo RM, San Millán JM, Sancho J, Ávila S, Escobar-Morreale HF. Prospective study of the prevalence of the polycystic ovary syndrome in unselected Caucasian women from Spain. J Clin Endocrinol Metab. 2000;85: 2434-8.
Bajares de Lilue M, Pizzi R, Velázquez Maldonado E. Tratamiento del síndrome de ovario poliquístico. Manejo dermatológico. Caracas: Editorial Ateproca. 2007: 67-71; 80-84.
Checa Vizcaíno, M.A., Espinós Gómez, J.J., Matorras Weining, R. (2005). Síndrome del ovario poliquístico. Buenos Aires; Madrid: Médica Panamericana. Sociedad Española de Fertilidad (SEF). ISBN 84-7903-599-4
ESHRE/ASRM Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome. Fertil Steril 2004; 81:19-25
Griesinger G. y col. (2006). GnRH-antagonists in ovarian stimulation for IVF in patients with poor response to gonadotropins, polycystic ovary syndrome, and risk of ovarian hyperstimulation: a meta-analysis. Reproductive BioMedicine Online; 13: 628-638.
Huddelston HG (2013). Biomarkers of ovarian reserve in women with polycystic ovary syndrome. Semin Reprod Med.
Moll E, van der Veen F, van Welly M. The role of metformin in polycystic ovary syndrome: a systematic review. Hum Reprod Update 2007; 13(6):527-37.
Reproducción Asistida ORG. Video: Sindrome del Ovario Poliquístico (Polycystic ovary syndrome), by Miguel Ángel Vincenti Bosco, MD, Jun 27, 2013. [See original video in Spanish].
Thessaloniki ESHRE/ASRM-Sponsored PCOS Consensus Workshop Group. Consensus on infertility treatment related to polycystic ovary syndrome. Hum Reprod 2008; 23(3):462-77
Zawadski JK, Dunaif A. Diagnostic criteria for polycystic ovary syndrome: towards a rational approach. En: Dunaif A, Givens JR, Haseltine FP, Merriam GR (eds.). Polycystic ovary syndrome. Boston: Blackwell Scientific Publications. 1992:377-384.
FAQs from users: 'What are my chances of getting pregnant with IUI if I have PCOS?', 'Can PCOS be cured?', 'Can metformin help you get pregnant with PCOS?', 'Does PCOS run in the family?' and 'What treatment options can help you get pregnant with PCOS?'.
Authors and contributors






Hi!
I’m 28 years old and have been trying for 5 years to get pregnant. I went to lots of specialists and they all tell my I have polycystic ovaries and they gave me different types of treatments which didn’t help me at all. Then, they also told me to lose weight so I went from 60kgs to 50 but nothing happened. I don’t know what to do anymore, I want to become a mother so desperately and I am so frustrated about it.
Someone could tell me if the diane serves to regularize my menstruation, I have polycystic ovaries and some horrible months of bleeding, I’m taking diane but I don’t see results.
Hi Tina,
Diane are birth control pills and therefore serve to regulate menstruation. However, if this method is not working for you, you should go to your gynecologist for another treatment.
Hope this helps you,
all the best.
Hello, everyone. After two surgeries I was diagnosed with polycystic ovary. I was prescribed diane for a year and metformin two tablets a day. After that time I stopped the treatment and was prescribed dexamethasone one tablet daily, omifin 100 mg on the fifth sixth and seventh day of my period, in that cycle I did not get pregnant. The next month I was prescribed dexamethasone, 1500 mg metformin daily, and 150 mg omifin on the fifth, sixth, and seventh days. And that month I got pregnant. I have a beautiful, healthy son, he is already 3 years old and I am trying again. Cheer up, I also went from doctor to doctor, not to mention the exhausting studies.
Hi!
I’m 28 years old and have been trying for 5 years to get pregnant. I went to lots of specialists and they all tell my I have polycystic ovaries and they gave me different types of treatments which didn’t help me at all. Then, they also told me to lose weight so I went from 60kgs to 50 but nothing happened. I don’t know what to do anymore, I want to become a mother so desperately and I am so frustrated about it.
Hey! I was diagnosed with PCOS a few months ago and my obstetrician recommended me to quit milk and dairy foods but now I’m suffering from calcium so how do you usually get calcium rich nutrition? Please, help me.
Hello,
As you said, dairy foods are inflammatory for PCOS, that’s why they are not recommended. But there are several alternatives to cow’s milk such as soyamilk, a very healthy alternative. Apart from that, there are plenty of non-dairy foods containing calcium. I give you a list hereunder:
– Collard greens
– Broccoli
– Kale
– Broccoli rabe
– Edamame
– Figs
– Oranges
– White beans
– Tofu
– Almonds
Hope this helps improve your calcium rich nutrition!
Sorry… I was diagnosed with PCOS 4 years ago and I’ve been struggling so hard ever since against this illness. I find natural remedies powerful but they only last a few hours… I mean, the following day you’ll have to continue dealing with your misery. Sorry, there’s no mercy for us!