When a woman is undergoing fertility treatment, medications must be given to stimulate the ovaries. This is called controlled ovarian stimulation (COS).
Ovarian stimulation drugs contain hormones that act naturally in the menstrual cycle and their function is to cause more than one egg to mature.
Depending on the fertility treatment and the number of eggs required one or two in artificial insemination (AI) and several for in vitro fertilization (IVF), the stimulation should be more or less gentle. This is controlled by adjusting the hormone dose and keeping track by ultrasound.
Provided below is an index with the 8 points we are going to expand on in this article.
- 1.
- 2.
- 2.1.
- 2.2.
- 2.3.
- 3.
- 3.1.
- 3.2.
- 4.
- 5.
- 5.1.
- 5.2.
- 5.3.
- 5.4.
- 5.5.
- 5.6.
- 5.7.
- 5.8.
- 5.9.
- 5.10.
- 5.11.
- 6.
- 7.
- 8.
What is hormonal medication for?
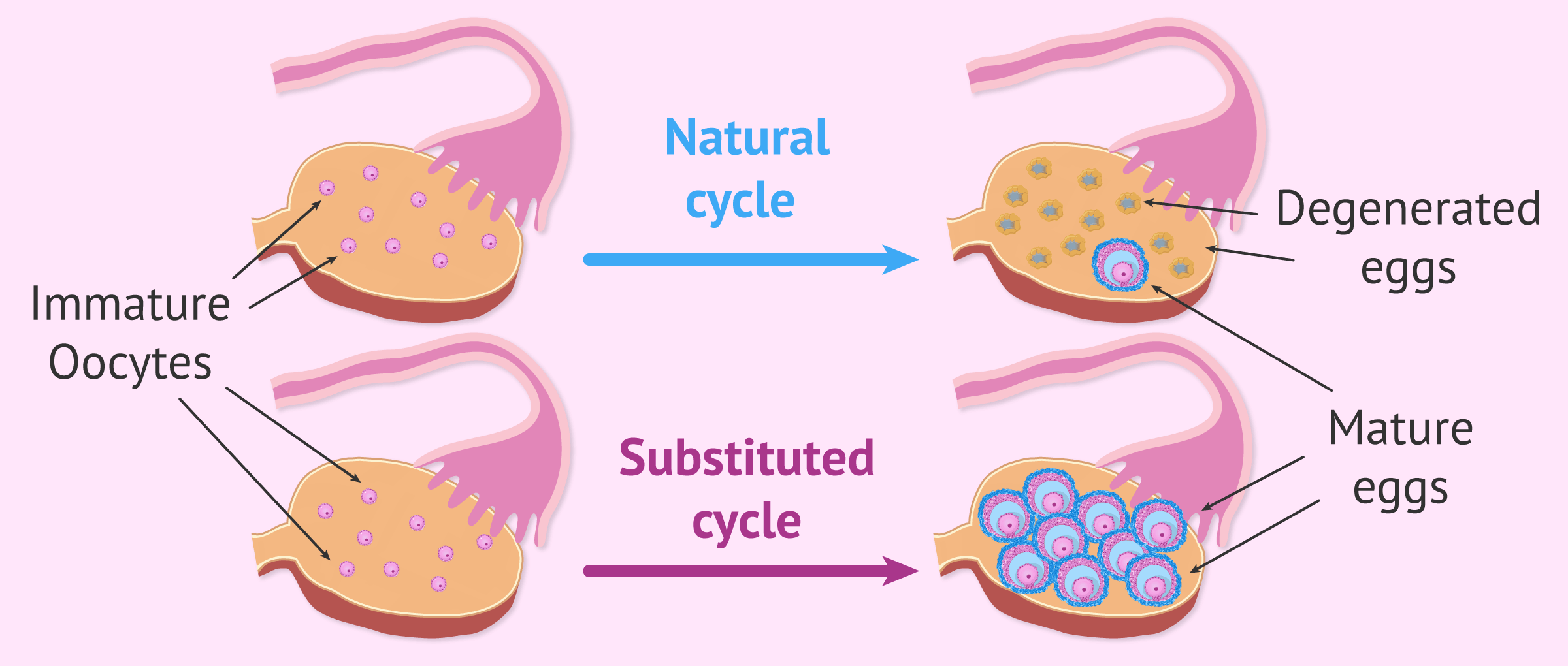
At the beginning of each menstrual cycle, a group of eggs begins to mature in the ovary in sacs filled with liquid: the follicles. This is what is known as follicular cohort.
Due to the hormonal flow between the hypothalamus, the pituitary gland and the ovaries, finally only one of these follicles is able to develop completely and become a preovulatory follicle. The rest of the follicles degenerate and the eggs inside them are lost.
The FSH and LH hormones secreted by the pituitary gland are responsible for regulating all follicular development and allowing the ovulation of a follicle towards the middle of the menstrual cycle.
Since in assisted reproduction it is necessary to obtain several mature follicles to increase the chances of pregnancy, it is essential to administer specific hormonal medication to the woman during a menstrual cycle.
These drugs are intended to "trick the ovaries" to allow the maturation of the entire follicular cohort. In this way, the ovarian follicles that were destined to degenerate manage to grow at the same time and give rise to mature eggs that can be fertilized.
Different types of hormonal drugs
There are several hormone-controlled medications available to perform controlled ovarian stimulation, but in general they can be grouped into two groups: GnRH analogues and gonadotropins.
Both types of medication have different functions and are essential for any artificial insemination or in vitro fertilization treatment, although there are exceptions such as, for example, IVF in the natural cycle.
In the following section, we are going to discuss the drugs that are included within each type and the function they perform during an assisted reproductive cycle.
GnRH analogues
These medications serve to annul all the internal hormones that act in a woman's menstrual cycle with two objectives: to allow ovarian stimulation to begin in a coordinated manner with the growth of all the eggs at the same time and also to avoid natural ovulation.
Here, we are going to explain its mechanism of action in detail.
GnRH is a hormone secreted by the hypothalamus whose function is to regulate hormone secretion by the pituitary gland. Both hypothalamus and pituitary glands are found in the brain and are very important in the reproductive system.
With GnRH analog drugs, the intention is to mimic the function of the natural hormone, but in such a way that the pituitary gland is blocked and cannot secrete the hormones FSH and LH.
This results in a state of pituitary suppression in which the hormonal flow between the brain and the ovaries is inhibited and the menstrual cycle is stopped.
Due to their structure and their way of acting, two types of GnRH analogues are differentiated:
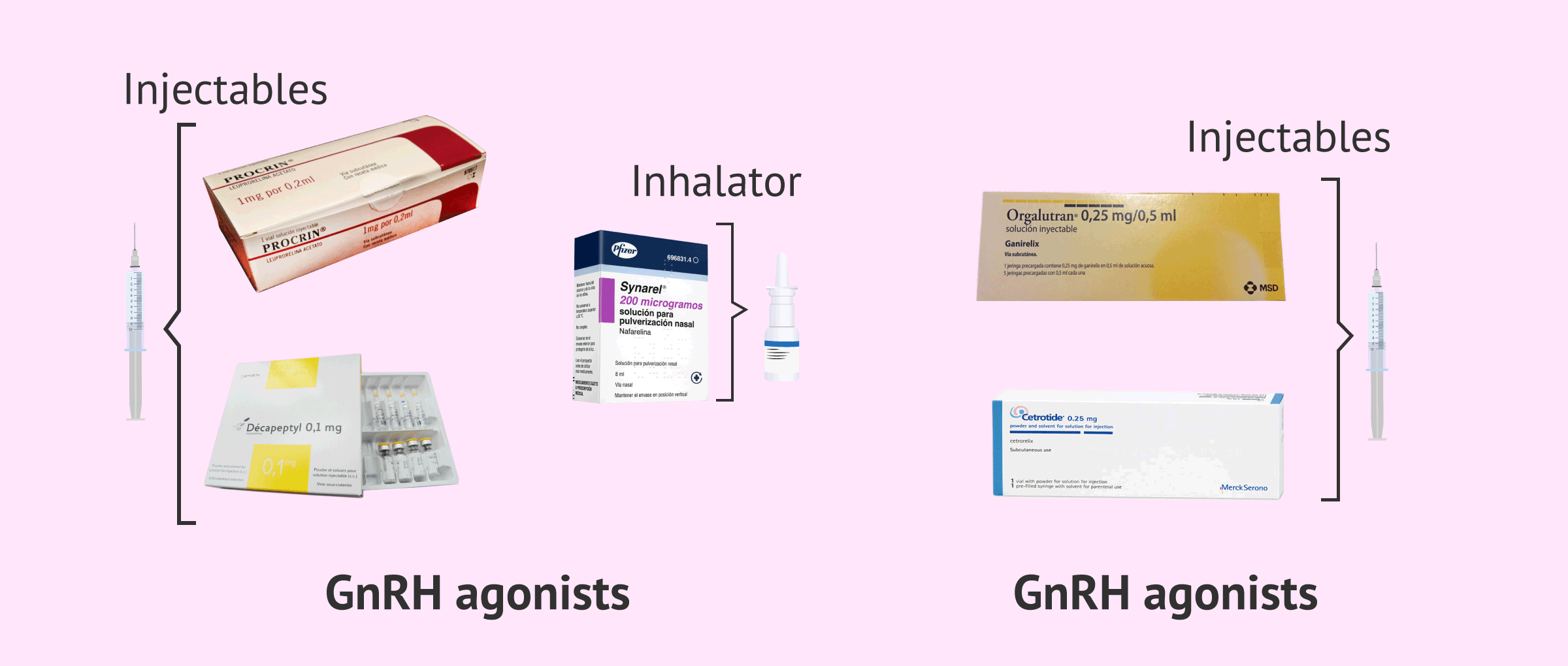
- GnRH Agonists
- bind to the GnRH receptor in the pituitary gland and, in the first place, cause an abrupt release of gonadotropins (flare-up effect). However, after several days of continuous administration, GnRH receptors are blocked. The trade names of these GnRH agonist drugs are Decapeptyl, Procrin and Synarel. The first two are administered by injection, but Synarel consists of a nasal inhaler that is easy to apply.
- GnRH Antagonists
- their inhibitory effect is more immediate, so they manage to block the pituitary gland within a few hours of administration. This advantage makes the number of punctures needed for the COS much lower, which is more comfortable for the woman. The trade names of these GnRH agonist drugs are Decapeptyl, Procrin and Synarel. Both are administered by subcutaneous injections.
In short, although both drugs act differently, their purpose is the same: to block brain control of the ovarian cycle in order to control the development of the entire follicular cohort at the same rate.
Gonadotropins
In a normal menstrual cycle, gonadotropins are the hormones that make it possible for a single follicle to grow in one of a woman's ovaries, which will expel a mature egg into the fallopian tube so that natural fertilization can occur.
The drugs used in ovarian stimulation contain gonadotropins to perform this same function, but on a large scale. The functions of each of the gonadotropins are detailed below:
- Drugs with FSH
- it's the follicle-stimulating hormone. These drugs induce multiple follicular development in which several eggs mature at the same time in the ovaries. The trade names of the drugs containing FSH are Gonal-f, Puregon, Ovaleap, Bemfola, Fostipur, Rekovelle and Elonva. All are administered by subcutaneous injections.
- Drugs with LH
- is the luteinizing hormone, which can be used in addition to FSH to try to reproduce the conditions of the natural menstrual cycle as much as possible. Drugs containing LH, in addition to FSH, are Menopur, Meriofert, HMG-lepori, and Pergoveris. All are administered by subcutaneous injections.
- Drugs with hCG
- This is the human chorionic gonadotropin hormone. It is injected 32-36 hours before follicular puncture in order to induce final maturation of the eggs. The best known medicine containing hCG is Ovitrelle and consists of a single subcutaneous injection.
Since hCG causes ovulation approximately 36 hours after administration, it is necessary to collect eggs from the ovary before they are naturally released into the fallopian tube and lost.
This is the main reason why it is so important to inject the hormonal medication at the exact time indicated by the in assisted reproduction specialized gynecologist.
Many women who have medication errors have had to cancel the COS cycle because of a poor response or spontaneous ovulation.
Another thing for assisted reproductive patients to keep in mind is that the gynecologist may prescribe two different medications to be given together during stimulation. For example, Gonal-f and Menopur.
Drugs for preparing the endometrium
Although not part of ovarian stimulation, women undergoing an assisted reproductive cycle should also be medicated for endometrial preparation.
The drugs used to do this are mainly composed of sex hormones that naturally secrete the ovary (estrogen and progesterone) and begin to be administered just after follicular puncture.
The following medications are used to prepare the endometrium:
- Estrogen drugs
- its function is to provoke the growth of the endometrium so that little by little its thickness increases. Normally, estrogen medications are usually given in substituted cycles for the transfer of frozen embryos or from egg donation. Some trade names for estrogen drugs are Evopad, Meriestra, and Progynova. It is usually administered in transdermal patches or oral tablets.
- Drugs with progesterone
- its function is to cause endometrial cells to mature so that the endometrium becomes receptive and the embryos can implant. Progesterone is naturally synthesized by the corpus luteum of the ovary after ovulation occurs. However, progesterone drugs in fertility treatments offer good results in supporting the luteal phase. Some trade names are Utrogestan, Progeffik, Crinone and Prolutex. Progesterone is most commonly given by vaginal ova, although it can also be given orally, with injections, or as a gel.
The thickness of the endometrium plays a very important role in embryo implantation, so good endometrial preparation is essential to finally achieve gestation.
As Dr. Miguel Dolz confirms:
There are various strategies for attempting to improve endometrial receptivity or uterine receptivity in those patients who have poor receptivity.
Ovarian stimulation protocols
Currently, there are two protocols or methods for the administration of hormonal drugs during COS: the long protocol and the short protocol.
The main differences between the two are their duration and the number of injections to administer.
The doctor responsible for the treatment must decide which of the two protocols to follow and the dose of medication needed in each woman, always adapting to their characteristics and with the aim of achieving the greatest possible success.
Long protocol
It begins with the administration of a GnRH agonist drug in the previous menstrual cycle, on the 21st day of the cycle. About 10-14 days later, the woman will have monthly bleeding.
At this very moment, ovarian stimulation with gonadotropins can begin. Between the first and third days of the period, the doctor will indicate the daily hormonal dose of FSH drugs that the woman should take.
When ultrasound shows that the ovarian follicles have reached the appropriate size (between 18 and 20 mm) and estradiol levels are also optimal, the doctor will indicate to the woman that they have to inject hCG to cause final maturation.
Follicular puncture must be performed before 36 hours to avoid spontaneous ovulation.
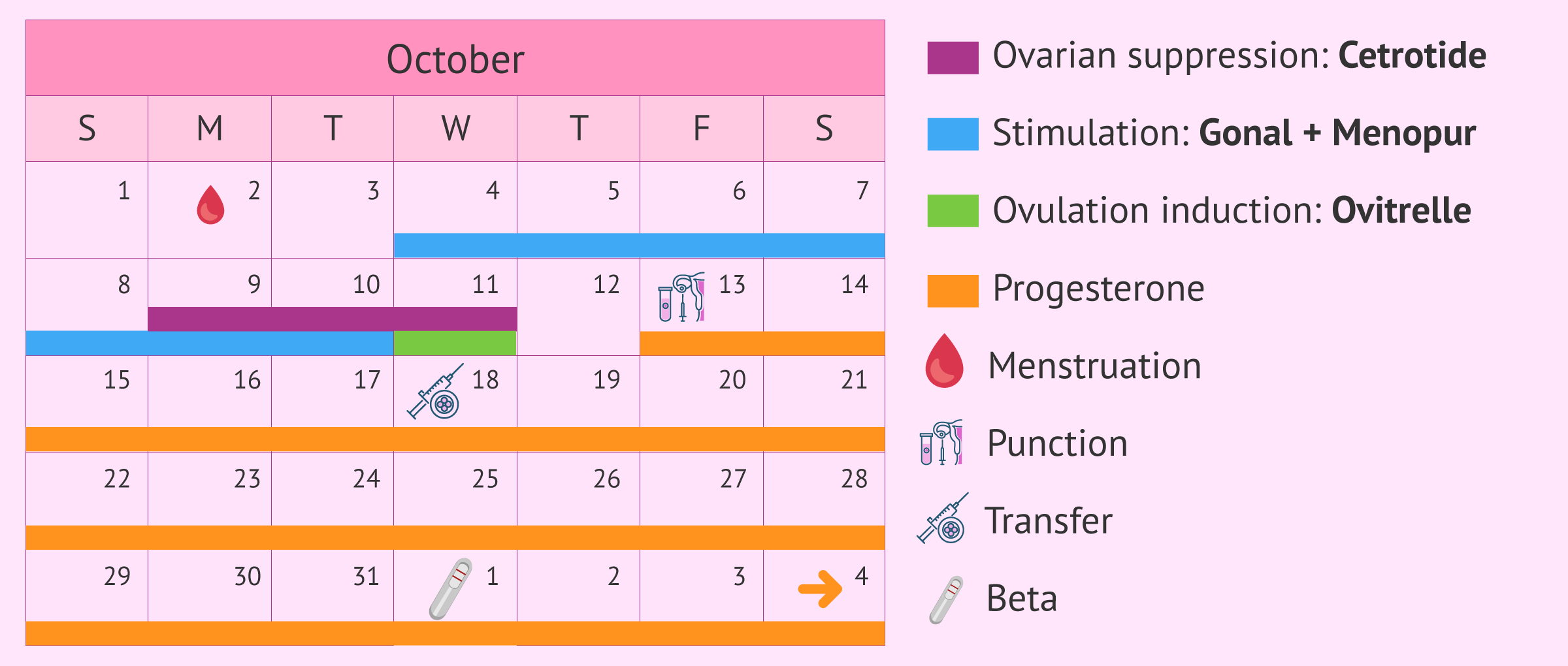
The following image shows a medication schedule of a patient who followed a long stimulation protocol, which lasted 22 days between the first day and the day of follicular puncture.
Short protocol
In this case, ovarian stimulation begins with the administration of gonadotropins at the beginning of the menstrual cycle, between the first and third day after the beginning of menstruation. In the previous menstrual cycle, it is common for a woman to receive birth control pills to coordinate the cycle.
After about 5 days of stimulation and follicle development, it is necessary to administer a GnRH antagonist drug to avoid the endogenous LH peak that would trigger ovulation.
Injections of the antagonist medication should be administered daily until the follicular puncture is scheduled. At that time, the doctor will order the patient to stop all medication and inject an ovulation inducer which, in this case, there are two options:
- Administer Ovitrelle with the hormone hCG.
- Administer a GnRH agonist, such as Decapeptyl, to take advantage of the flare up effect and induce the internal release of LH.
Follicular puncture will also have to be performed before 36 hours so that mature eggs are not lost. The following image shows a medication schedule of a patient who followed a long stimulation protocol, which lasted 10 days between the first day and the day of follicular puncture.
Get more information about this stimulation protocol here: Short stimulation protocol in IVF with GnRH antagonists.
The duration of a short stimulation protocol is about 8-12 days, while in a long protocol it is necessary to add about 10-15 more days of previous preparation.
Personalized ovarian stimulation
Depending on the assisted reproductive treatment indicated to the patient, more or fewer eggs will be needed to achieve success:
- Artificial insemination 1 or 2 eggs
- IVF: 6 to 18 eggs
Therefore, the type of ovarian stimulation and, above all, the dose of hormonal drugs administered will depend on the number of eggs needed to obtain.
However, there are other factors related to the patient that are determinant when it comes to determining the dose of hormonal medication and the stimulation protocol:
- Age
- Body Mass Index (BMI)
- FSH baseline
- Antral follicle count
- Ovarian response in previous treatments
- Pathologies or conditions affecting the ovaries, such as endometriosis or polycystic ovaries
This is why it is said that ovarian stimulation is personalized, that is, adapted to each patient, their characteristics and their needs. You have more information on this topic in the following article: What is ovarian stimulation?
If you need to undergo IVF to become a mother, we recommend that you generate your Fertility Report now. In 3 simple steps, it will show you a list of clinics that fit your preferences and meet our strict quality criteria. Moreover, you will receive a report via email with useful tips to visit a fertility clinic for the first time.
FAQs from users
What can happen if hCG is administered too late?
HCG is a hormone that is administered 36 hours before egg collection. In some cases, a GnRH analog is administered instead.
These hormones are responsible for facilitating the final process of oocyte maturation and ovulation. It is crucial to administer these hormones at the time indicated by your assisted reproduction specialist, as doing so too early could cause premature ovulation, therefore preventing oocytes recovery when performing the egg collection.
Administering the trigger injection too late could lead to a lack of maturation of the oocytes, which leads to a lower oocyte recovery rate (because part of these cumulus-oocyte complexes will still be adhered to the follicle wall, and therefore will not be recovered in the egg collection) and that the collected oocytes will probably be immature and not suitable thus to be used for the treatment.
Can there be any complications with the use of the Puregon Pen?
The use of the Puregon Pen carries no greater risk than any other gonadotropin.
For how many days do I have to administer the medication for ovarian stimulation?
The treatment for ovarian stimulation usually lasts 8-11 days but it depends on each patient and the response to the medication. The important thing is to carry out control ultrasounds to keep the medication for the indicated time and in this way achieve the best possible response for each patient.
Can I use pills for ovulation induction instead of subcutaneous injections?
No, medications for ovarian stimulation are administered subcutaneously with injections, generally into the abdomen area. There exists a nasal spray, but is rather uncommon. Although they are administered with a needle, it is a simple and painless procedure.
What are the main side effects of ovulation induction medications?
Ovarian stimulation is done with hormone medications, which can cause some side effects. They are not painful or specially severe, though. By no means they are symptoms that could hinder the donor from continuing with her everyday routine.
Commonly, headache, bloating, tiredness, etc. are the most common symptoms during the days leading up to egg retrieval.
In case the donor develops OHSS (Ovarian Hyperstimulation Syndrome), the symptoms derived from it can be moderate to severe. The good news is that only a small percentage of women develop OHSS, and it can be often prevented through ultrasound monitoring. You can get more information about it here: Ovarian Hyperstimulation Syndrome.
Do fertility drugs lead to gain or lose weight?
Ovulation induction protocols last around 10 days, so appreciating a weight gain or loss after that is rather unlikely. However, donors can develop a mild water retention as a side effect of hormone therapy, but it occurs rarely.
Can fertility drugs cause early menopause?
No, ovarian stimulation does not affect the donor's fertility, as eggs that would have degenerated end up developing fully, so it does not reduce the number of eggs which would have grown naturally, which is to say, the chances of getting pregnant naturally in the future do not diminish.
What are the main reasons for poor response to fertility drugs?
Women requiring larger doses of stimulation drugs are commonly called "poor responders". Although there is no clear definition for what can be considered a low response to IVF drugs, many authors use a cut-off of less than 4 mature eggs at the time of hCG shots or an estradiol level of less than 500.
Low response is detected through ovarian reserve testing, including basal FSH levels. Ultrasound assessment of the ovaries and the antral follicle number are also good predictors of poor responders to stimulation drugs.
A cycle can be cancelled if less than 4 mature eggs are produced or if no response is obtained at all.
What types of IVF protocols can be found?
Even though the purpose of taking fertility drugs is always the same, different protocols, ways to induce ovulation and prepare the endometrial lining can be found.
Depending on each woman's situation, the medications to take and the dose that best fits her need are determined. This is the reason why fertility testing is necessary prior to IVF treatment. Monitoring the response to medications and changing the type of drug or dose is crucial, too.
Are fertility drugs harmful or dangerous?
The associations between IVF drugs and the risk of ovarian or breast cancer are weak, and conclusive studies are scarce to date. There is no convincing evidence that they raise a woman's risk of developing any of these types of cancer.
Can you travel by plane with fertility meds?
Experts recommend not to travel abroad by plane while on fertility treatment. Instead, you are encouraged to look for ways to relax and postpone your journey if possible.
Suggested for you
There are many female hormones involved in the process of reproduction, which is secreted by various organs such as the pituitary or ovary. If you are interested in this topic, you can continue reading in the next post: Sex hormones- Definition and Functions.
The hormones LH and FSH control a woman's menstrual cycle and its different phases. If you want to read more about this, click here: The different phases of the menstrual cycle.
If you want more information about fertility treatments, we recommend you read the following article: Assisted Reproduction Techniques
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
Allegra A, Marino A, Coffaro F, Scaglione P, Sammartano F, Rizza G, Volpes A (2007). GnRH antagonist-induced inhibition of the premature LH surge increases pregnancy rates in IUI-stimulated cycles. A prospective randomized trial. Hum Reprod; 22: 101 – 108.
Arici A, Byrd W, Bradshaw K, Kutteh WH, Marshburn P, Carr BR (1994). Evaluation of clomiphene citrate and human chorionic gonadotropin treatment: a prospective, randomized, crossover study during intrauterine insemination cycles. Fertil Steril;61:314 – 318.
Balasch J, Ballescà JL, Pimentel C, Creus M, Fàbregues F, Vanrell JA (1994). Late low-dose pure follicle stimulating hormone for ovarian stimulation in intrauterine insemination cycles. Hum. Reprod.; 9: 1863– 1866.
Bhattacharya S, Harrild K, Mollison J, Wordsworth S, Tay CCK, Harrold A, McQueen D, Lyall H, Johnston L, Burrage J et al. (2008). Clomifene citrate or unstimulated intrauterine insemination compared with expectant management for unexplained infertility: pragmatic randomised controlled trial. BMJ;337:716 – 723.
Coroleu B, Devesa M, y Alvarez M. Guía 18. Estimulación ovárica para FIV-ICSI en los ciclos con presunción de baja respuesta. Servicio de Medicina de la Reproducción Departamento de Obstetricia, Ginecología y Reproducción Hospital Universitario Quirón Dexeus, Barcelona. Sociedad Española de Fertilidad (SEF) y Sociedad Española de Ginecología y Obstetricia (SEGO)
Ferraretti AP et al. (2011). ESHRE consensus on definition of poor response to ovarian stimulation for in vitro fertilization: the Bologna criteria. Hum Reprod; 26: 1616-24.
Griesinger G. y col. (2006). GnRH-antagonists in ovarian stimulation for IVF in patients with poor response to gonadotropins, polycystic ovary syndrome, and risk of ovarian hyperstimulation: a meta-analysis. Reproductive BioMedicine Online; 13: 628-638.
Hamdine O. et al. (2015). Ovarian response prediction in GnRH antagonist treatment for IVF using anti-Müllerian hormone. Hum. Reprod.; 39: 170-8.
Lehert P, Kolibianakis EM, Venetis CA. y col. (2014). Recombinant human follicle-stimulating hormone (r-FSH) plus recombinant luteinizing hormone versus r-FSH alone for ovarian stimulation during assisted reproductive technology: a systematic review and meta-analysis. Reproductive Biology and Endocrinology; 12: article 17.
Nelson SM (2013). Biomarkers of ovarian response: current and future applications. Fertil. Steril.; 99: 963-9.
Rodríguez Gálvez, I., Tocino Díaz, A., Fernández Sánchez, M. Fármacos en la estimulación ovárica: clomifeno, gonadotropinas, análogos GnRH, hCG. En: Unidad 06, Bloque I: Esterilidad femenina. Máster en Reproducción Humana de la Universidad Rey Juan Carlos y el Instituto Valenciano de Infertilidad (IVI).
FAQs from users: 'What can happen if hCG is administered too late?', 'Can there be any complications with the use of the Puregon Pen?', 'For how many days do I have to administer the medication for ovarian stimulation?', 'Can I use pills for ovulation induction instead of subcutaneous injections?', 'What are the main side effects of ovulation induction medications?', 'Do fertility drugs lead to gain or lose weight?', 'Can fertility drugs cause early menopause?', 'What are the main reasons for poor response to fertility drugs?', 'What types of IVF protocols can be found?', 'Are fertility drugs harmful or dangerous?' and 'Can you travel by plane with fertility meds?'.
Authors and contributors










Do you know how many eggs are retrieved during egg retrieval in the case of healthy donors? Thnx
Hello Lucy,
As explained above, the average is 10-15 eggs per cycle, although egg donors can produce 16 or even more oocytes.
Regards