The incidence rate of poor responders (PORs) to stimulation in IVF cycles ranges currently from 7 to 24%. This percentage is even higher in patients aged 38 years or older. The main causes are ovarian aging and having a low ovarian reserve.
However, it is important not to confuse low ovarian response to hormonal drugs with low ovarian reserve, as these are different terms. A woman may have a low ovarian reserve, but have a good response to hormonal stimulation.
Provided below is an index with the 11 points we are going to expand on in this article.
- 1.
- 2.
- 3.
- 4.
- 5.
- 6.
- 6.1.
- 6.2.
- 6.3.
- 6.4.
- 6.5.
- 7.
- 8.
- 8.1.
- 8.2.
- 8.3.
- 8.4.
- 8.5.
- 8.6.
- 8.7.
- 8.8.
- 9.
- 10.
- 11.
What is low ovarian response?
Low ovarian response refers to the low yield of mature eggs after follicular puncture in IVF treatment. However, there is no general agreement among specialists to define low response to ovarian stimulation.
For this reason, it is necessary to evaluate a set of factors to determine that there is a low response in a woman:
- Number of follicles in the ovary
- 5 or less follicles are seen through transvaginal ultrasound in the ovaries.
- Number of eggs retrieved
- If only 3 to 5 eggs have been retrieved. However, organizations such as the Spanish Fertility Society (SEF) consider that a woman is a poor responder if 3 or less eggs are retrieved.
- Stimulation protocol
- When a low number of eggs is collected in spite of having administered a dose of FSH below 3,000 IU.
- Estradiol (E2) levels
- A peak E2 level of <500 pg/ml after a cycle of ovarian stimulation.
The prevalence of low response to stimulation in fertility treatments is variable, but it is estimated to occur in 7-24% of women. In addition, it should be noted that low ovarian response to hormonal drugs can be caused by factors such as age, genetic factors, pelvic infections, etc.
Low female responder
A woman is considered a low responder when, after undergoing two cycles of ovarian stimulation, she obtains 3 or fewer follicles in each cycle and serum estradiol levels below 500 pg/ml on the day of the hCG injection.
These types of women need continuous emotional support, as there is a greater chance of canceling the cycle and repeating the stimulation treatment a greater number of times. In addition, it would be important to apply a personalized stimulation treatment in each patient's IVF cycle.
The ovarian age does not always match the biological age. Some women are born with an increased number of eggs in their reserve, while others are capable of developing a higher number in each cycle.
Therefore, it is necessary that fertility treatment, as well as ovarian stimulation, be personalized from the beginning.
How to predict a low response?
Cases of low response are confirmed after ovarian stimulation. However, there is evidence for early diagnosis to guide the assisted reproduction treatment protocol.
Some of the factors that can predict low ovarian response in the patient are the following:
- Age
- Less than 5 primordial follicles seen on ultrasound
- Anti-Müllerian hormone (AMH) below 1 ng/ml
- Basal FSH levels above 10 mIU/ml
- Basal estradiol levels
- LH/FSH ratio
- Inhibin B: levels under 45 pg/ml confirm the existence of a declining ovarian reserve
- Others: clomiphene testing, ovarian volume...
- Diagnosis of POR in previous cycles
High FSH (Follicle-Stimulating Hormone) levels not only indicate POR but also help predict poor egg quality, which reduces the pregnancy success rate, while at the same time increasing the miscarriage rate.
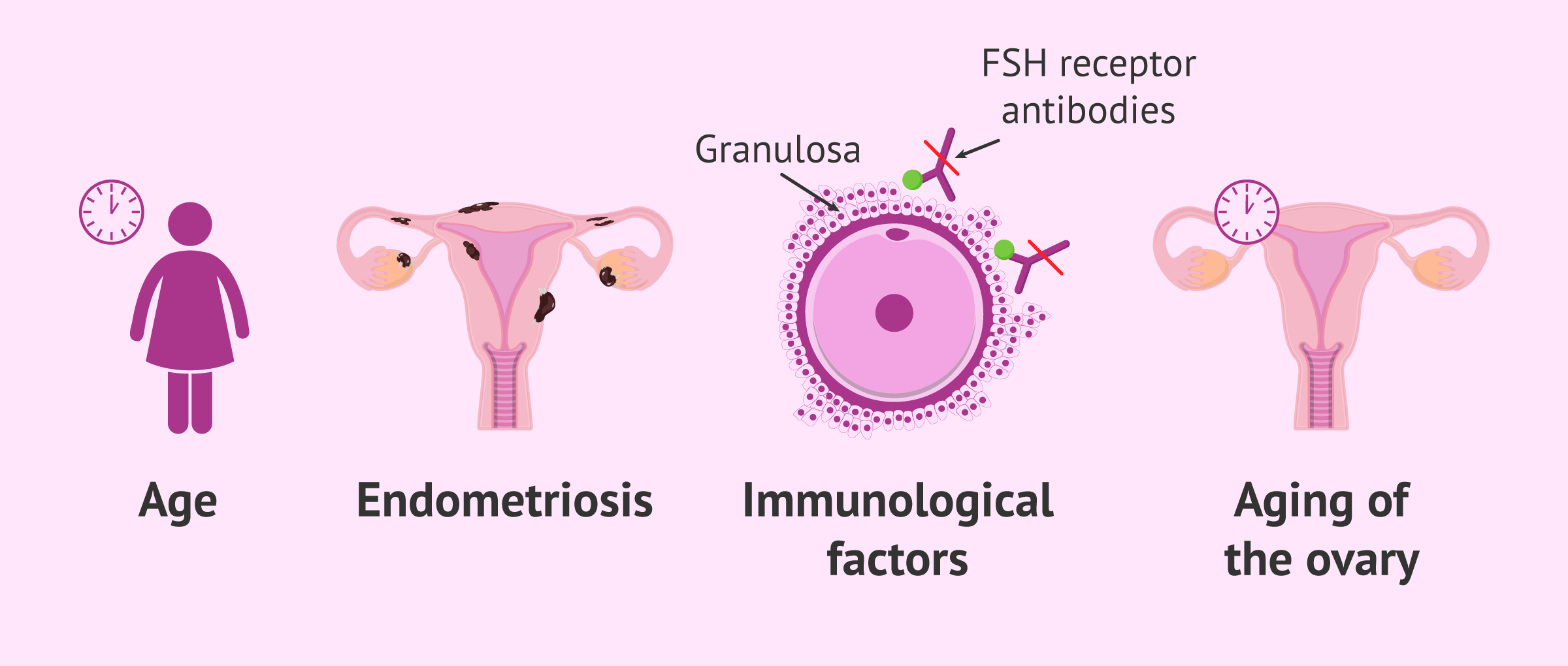
Causes of low ovarian response
The main causes of low ovarian response to drugs administered for stimulation are as follows:
- Age: It is inversely proportional to the ovarian reserve. The older, the harder for them to conceive due to a reduced egg supply.
- Autoimmune disease: Action of FSH receptors (FSHR) in the granulosa cells is blocked by FSH antibodies.
- Reduced ovarian size after undergoing surgery or treatment for endometriosis
- Ovarian aging
For more information on how to measure ovarian reserve, you can continue reading the following article: What Can Ovarian Reserve & AMH Tests Tell Us? - Results Explained.
Consequences of low response in an IVF cycle
The ultimate goal of every IVF cycle is to induce the production of multiple eggs so that a large number can be retrieved and at least one of them is able to result in a viable embryo.
This is precisely the reason why being a poor responder has negative effects on the outcomes of IVF. An insufficient number of eggs available for fertilization diminishes the chances of getting pregnant and increases the probability of canceling the embryo transfer.
Additionally, POR often leads to eggs of poorer quality that compromise the viability of the embryos at the laboratory, which increases the number of complications for these women.
See this for more: What Is a Good Number of Eggs Retrieved for IVF?
Solution for low responders
Fortunately, low responders in IVF have various options to deal with POR and achieve success. Let's find each one of them explained below.
Androgen pretreatment
After experiencing poor response during an IVF cycle, it is possible for the patient to start an androgen pretreatment in order to trigger the production of multiple eggs.
It can be done using transdermal testosterone or DHEA (oral dehydroepiandrosterone) replacement therapy. Their effectiveness in cases of PORs, however, has not been proved yet.
Converting an IVF cycle to IUI
If the development of one or two follicles was observed through ultrasound, we may consider the possibility of converting an IVF cycle to Intrauterine Insemination (IUI), always keeping in mind the remaining factors, including the presence of severe male infertility.
Modified ovarian stimulation protocols
In poor responder patients, we always try to offer more personalized treatment in order to obtain the largest possible number of eggs.
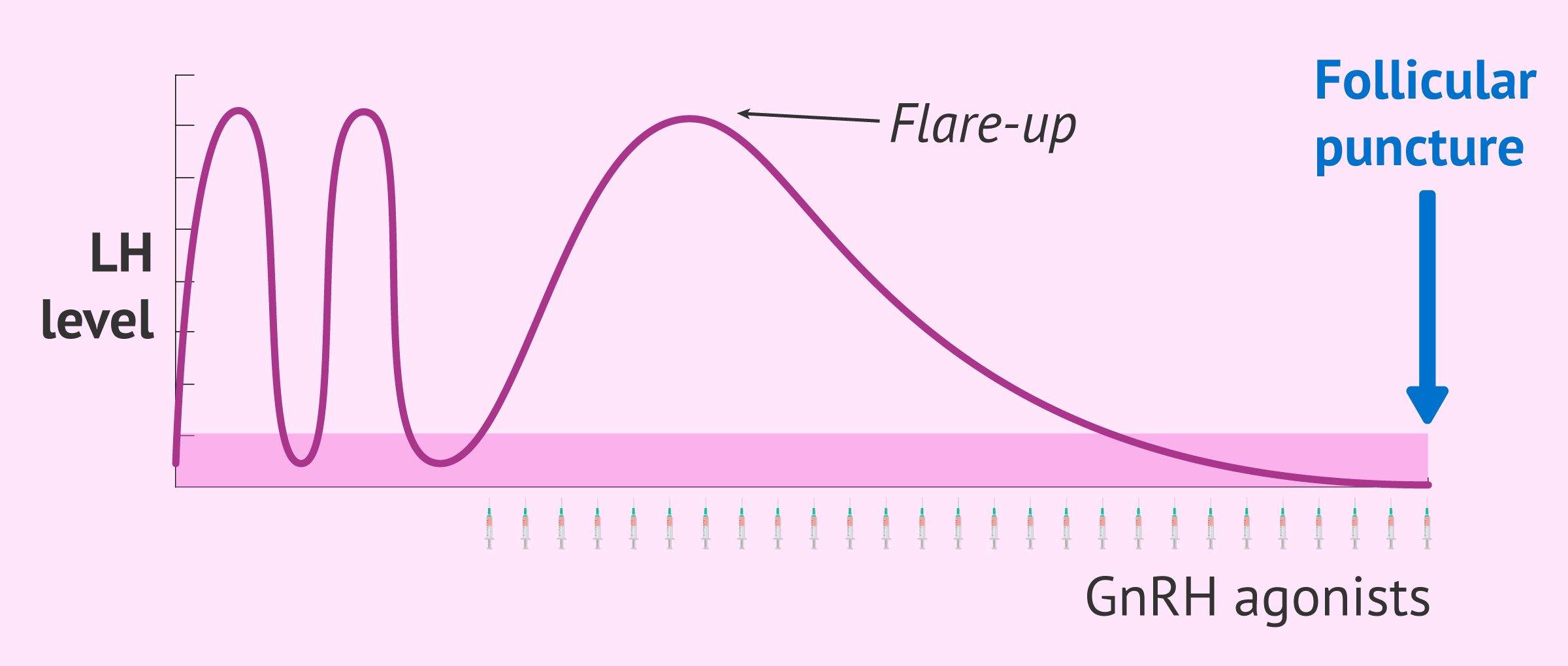
The short protocol with GnRH agonists known as flare-up offers better results in poor responders since it avoids the profound ovarian suppression of long treatment and takes advantage of the flare-up effect.
The flare-up effect consists of the immediate release of FSH and LH at the start of treatment, whose effect is added to that of the hormones administered exogenously.
We have discussed GnRH agonists as a suitable treatment for low responders. You can learn more about their indications, advantages, and disadvantages at the following link: GnRH analogues.
Oocyte banking with vitrification cycles
With the purpose of maximizing the number of eggs retrieved and subsequently increasing the number of viable embryos to transfer, several oocyte accumulation cycles can be performed.
Oocyte accumulation means that the eggs retrieved with each cycle are frozen until an optimal amount is available. Then, they are thawed, mixed with the fresh ones that were collected in the last cycle, and fertilized by ICSI.
Egg donation
When several IVF cycles have already been canceled due to low ovarian response, the most successful alternative is egg donation.
In IVF with egg donation, a young woman donates her eggs to another woman and these are fertilized by the sperm of the recipient woman's husband. This reproductive option has high success rates but also has the disadvantage of having to give up the woman's genetic load and its high cost.
If you need to undergo IVF to become a mother, we recommend that you generate your Fertility Report now. In 3 simple steps, it will show you a list of clinics that fit your preferences and meet our strict quality criteria. Moreover, you will receive a report via email with useful tips to visit a fertility clinic for the first time.
Given the delay of motherhood by the general population today, egg donation is widely used in all assisted reproduction clinics because, as the woman's age increases, the quality of her own eggs is very low. For this reason, to become a mother, she needs eggs from a young woman if she has not previously preserved her eggs.
Read more: What’s Being an Egg Donor Recipient Like? – Preparation & Process.
Cost of treatment options for PORs
Another complication derived in cases of poor ovarian response is related to the financial impact of several IVF cycles. This is the reason why selecting the right treatment option is crucial in order to make it as cost-affordable as possible.
The cost of an IVF cycle typically ranges between $8,500 and $12,000 on average. If you opt for a multiple cycle IVF cost plan, you should expect an average amount of about $16,000. This option can be very interesting for poor responders.
On the other hand, only the medications used for the microdose lupron flare protocol can cost up to $5,800 plus the costs of the IVF treatment itself. In case donor eggs were needed, you should expect prices from $20,000.
FAQs from users
Is the natural cycle a good option for poor responders?
In women who are poor responders, there is medical evidence for similar live birth rates using high dose ovarian stimulation vs. Natural cycle, particularly in younger women. This is presumably because poor responders do not produce many eggs and high does’ stimulation may be detrimental to egg quality. Younger reproductive aged women have the advantage of better egg quality. In older reproductive age women who are poor responders, the option of egg donation is usually much more successful in achieving a live birth. However, the optimal approach to the poor responder is far from certain.
Can a low antimüllerian be indicative of a low response?
Antimüllerian hormone (AMH) in women informs us of the number of ovarian follicles available, independent of the menstrual cycle and the age of the patient, although it is usually related to her reproductive age.
It is known that women are born with a finite follicular endowment that is depleted as they get older, therefore, a low antimüllerian is indicative that the number of total follicles available in the ovary is decreased. Fewer follicles available means less response. But this is not entirely true, since we have to take into account another important factor which is the AFR (Antral Follicle Count).
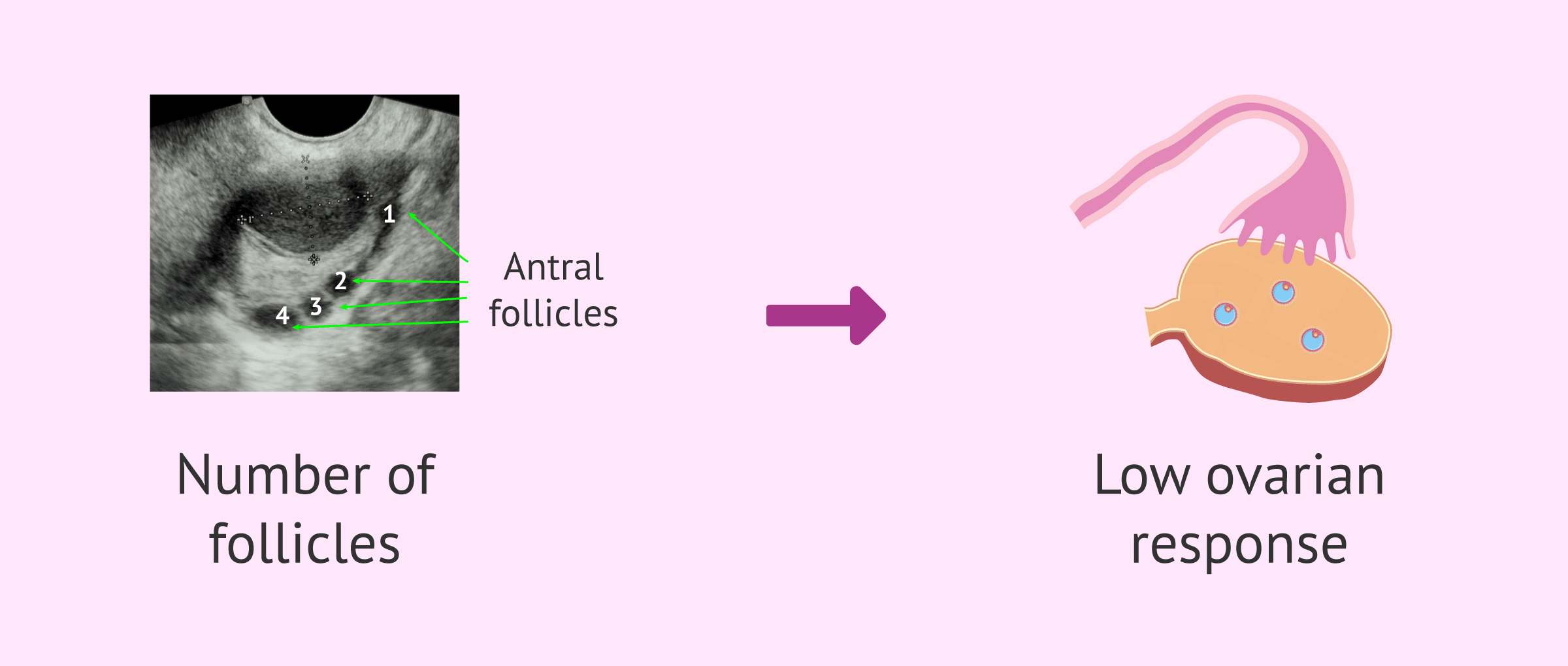
Each menstrual cycle the ovaries make a number of follicles available for development each cycle. This number of available follicles usually decreases with age but does not necessarily depend on the remaining count in the ovary. Let's say that they are complementary because what really defines the low response is the number of follicles available in each cycle (RFA) which is usually lower the AMH. They are usually related, but what really defines the low response is not AMH but the AFR.
What if the number of eggs I produce is insufficient for IVF?
In order to be able to fertilize more than one egg cell in the same IVF cycle, women's ovaries are stimulated using fertility drugs. The number of eggs required depend on the technique used. For IVF, it is enough with 1 or 2; whilst for IVF/ICSI, we should have around 10 eggs ideally. Oftentimes, due to a varied set of causes, the ovarian response of some patients is inadequate and the number of eggs collected is too low (below 5). In such cases, we can turn to the following strategies:
- To cancel the cycle before egg retrieval and start a new stimulation cycle with a different stimulation protocol.
- To freeze using egg vitrification technique the eggs to collect a higher number of eggs in subsequent cycles.
- To freeze using embryo vitrification technique the resulting embryos in order to transfer 2 in the subsequent cycle.
In short, it depends on the history of each couple.
What are the chances of natural pregnancy with a low ovarian response?
Women with low ovarian response are women who have already gone to an assisted reproduction clinic because they have not achieved a natural pregnancy. Therefore, this possibility is low, probably due to the decrease in ovarian reserve and aging.
Would PGD be a possible solution for low ovarian response?
No, PGD is a method to detect genetic abnormalities in embryos. Therefore, there is no advantage for women who have few eggs to fertilize.
Is Omifin recommended for low responders?
Yes, Omifin is a drug made up of clomiphene citrate that can be used as an adjuvant treatment. The advantages are the following:
- Allows moderate follicular growth.
- There is no blockade of endogenous FSH and LH.
- Allows stable and progressive increase in estradiol levels.
- The number of injections in the patient is less.
- The cost is cheaper.
Can I get pregnant with low ovarian response?
The answer is yes. When a low response to hormonal medication is observed in fertility treatment, a change from an AI cycle to IVF may be indicated. Another alternative would be to modify the ovarian stimulation protocol or to accumulate oocytes during several cycles of stimulation, prior to fertilization.
As a last option, pregnancy could be achieved in low responders by IVF with donor eggs.
Are low reserve and low ovarian response the same thing?
No. Ovarian reserve refers to the number of eggs available in a woman at a given time in her life. For example, if the woman has a maximum of 6 eggs and 4 mature eggs are obtained in the puncture, this would be considered a normal ovarian response.
On the other hand, the low ovarian response is when there are many eggs available, but only 3 or fewer mature eggs are obtained.
Recommended readings
Ovarian stimulation is a key step in every IVF cycle. Want to learn more about the process? Read: Ovarian Stimulation Protocols for IVF - Process & Medications Used.
A common doubt between IVF patient is related to the number of eggs that should ideally be retrieved for IVF. If this is your case, you may enjoy some further information reading this: What Is a Good Number of Eggs Retrieved for IVF?
The opposite to low ovarian response is having a high response, a side effect of IVF known as ovarian hyperstimulation syndrome or OHSS. Check out this for information: What Is the Ovarian Hyperstimulation Syndrome (OHSS)?
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
Badawy A, Wageah A, El Gharib M, Osman E. Prediction and Diagnosis of Poor Ovarian Response: The Dilemma. J Reprod Infertil. 2011 Oct-Dec; 12(4): 241–248.
Conforti A, Esteves S, Cimadomo D, Vaiarelli A, Di Rella F, Ubaldi F, Zullo F, De Placido G, Alviggi C. Management of Women With an Unexpected Low Ovarian Response to Gonadotropin. Front. Endocrinol., 27 June 2019 | https://doi.org/10.3389/fendo.2019.00387.
Kailasam C, Keay SD, Wilson P, Ford WC, Jenkins JM. Defining poor ovarian response during IVF cycles, in women aged <40 years, and its relationship with treatment outcome. Human Reproduction, Volume 19, Issue 7, July 2004, Pages 1544–1547, https://doi.org/10.1093/humrep/deh273Kallen P, Sundstrom P. The probability of successful IVF outcome after poor ovarian response. Acta Obstetricia et Gynecologica Scandinavica Volume 86, 2007 - Issue 4. Tarlatzis BC, Zepiridis L, Grimbizis G, Bontis J. Clinical management of low ovarian response to stimulation for IVF: a systematic review. Hum Reprod Update. Jan-Feb 2003;9(1):61-76. doi: 10.1093/humupd/dmg007.Venetis Efstratios M. Kolibianakis Theoni B. Tarlatzi Basil C. Tarlatzis. Evidence‐based management of poor ovarian response. Annals of the New York Academy of Sciences. 14 September 2010FAQs from users: 'Can I have sex as a low responder in ovulation induction?', 'Is the natural cycle a good option for poor responders?', 'Can a low antimüllerian be indicative of a low response?', 'What if the number of eggs I produce is insufficient for IVF?', 'What are the chances of natural pregnancy with a low ovarian response?', 'Can poor responders use supplements to improve IVF outcomes?', 'Would PGD be a possible solution for low ovarian response?', 'Growth hormone for IVF poor responders, yay or nay?', 'Is Omifin recommended for low responders?', 'What's the best IVF protocol for poor responders?', 'Can I get pregnant with low ovarian response?' and 'Are low reserve and low ovarian response the same thing?'.
Authors and contributors

More information about Cristina Algarra Goosman








Hello dr, this is my 1st ivf cycle and after 7 days on gonal 900 and menopur i have three mature eggs in each ovary… is it normal or i’m a poor responder? i’m 34…
Dear Karli,
If you have 3 eggs in each ovary, that means that you have a total of 6 mature eggs to fertilize. Poor ovarian response is diagnosed when there are less than 6 follicles, so you are within the normal threshold yet.
Wishing you the best of luck!