Intrauterine insemination with donor sperm, also known as artificial insemination with donor sperm (AID) is an assisted reproductive treatment indicated for couples with a severe male factor or for women who lack a male partner, whether they are single women or same sex female couples.
In these cases, the seminal sample used to perform the artificial insemination comes from a sperm bank.
Provided below is an index with the 11 points we are going to expand on in this article.
- 1.
- 1.1.
- 2.
- 2.1.
- 3.
- 3.1.
- 3.2.
- 4.
- 5.
- 6.
- 7.
- 8.
- 8.1.
- 8.2.
- 8.3.
- 8.4.
- 8.5.
- 8.6.
- 8.7.
- 8.8.
- 9.
- 10.
- 11.
When is IUI with donor sperm recommended?
Intrauterine insemination with donor sperm is a simple reproductive technique that is used in many cases, but IUI is not always possible. The main reasons for doing an IUI with a sperm donor are the following:
- Single mothers by choice: women who decide to be single mothers.
- Same sex female couples: couples of women who decide to have a child together.
- Risk of transmission of genetic diseases from the father, although preimplantation genetic diagnosis (PGD) should be considered first.
- Severe male infertility: very poor semen quality, secretory azoospermia, sperm DNA fragmentation, etc.
- Failed attempts at other assisted reproduction treatments, such as in vitro fertilization (IVF) with own semen.
In the past, the fact that the father had a sexually transmitted disease (STD) was also an indication for an IAD. Currently this has changed thanks to seminal lavage techniques. For this reason, in these situations, artificial insemination can be performed using the partner's semen, which will have previously had pathogenic loads removed to prevent infection.
You can obtain more information about this technique in the following article: Washing of semen with HIV for techniques of assisted reproduction.
Donor sperm IUI for single women and lesbians
Today, a woman can be a single mother using donor sperm for artificial insemination. In this case, the assisted reproduction clinic will assign the woman a sperm donor who has characteristics similar to hers.
This family model has increased in recent years due to the fact that women are postponing motherhood until they find the moment of their life with greater stability. However, when this happens, it may happen that you do not have a partner.
Since women's fertility declines as they age, many women between the ages of 35-40 find themselves in the situation of having to decide if they really want to be mothers, whether they are in a partnership or not.
In the case of female homosexual couples, they can also become mothers thanks to IUI treatment with donor sperm. The legal aspects covering who will be the parent may vary from country to country as well as state to state.
For example, in Spain, for and IUI treatment with donor sperm the couple does not have to be married. Although only one of the two women will undergo the treatment to become pregnant, both will sign the consent for its performance, so the two women of the couple will be the legal mothers of the baby.
In the UK, in married or in a civil partnership, both the mothers will be the legal parents when undergoing a fertility treatment with donated sperm, as long as the treatment is carried out in a licenced clinic and both parents sign the consent forms.
In the USA, laws vary from state to state so it is always recommended to seek legal advice on the issue.
Donor artificial insemination process
The treatment of donor IUI is exactly the same as that of conjugal artificial insemination with the partner's semen. The only difference between the two procedures is obtaining the sperm.
When partner sperm is used it is usually provided fresh and then processed in the laboratory. In contrast, with donor IUI the semen comes from a bank where it has been frozen for at least 6 months. This cryopreservation time of the donated semen is necessary to verify that the donor does not have any type of infection such as HIV.
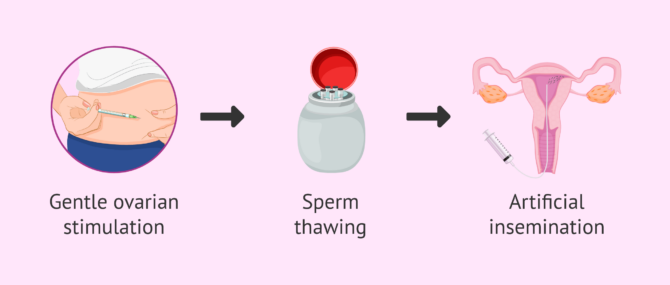
Therefore, the steps of intrauterine artificial insemination with a sperm donor are as follows:
- Controlled ovarian stimulation
- the woman's ovaries are gently stimulated so that only one or two eggs mature. Ovulation is then induced so that the specialist can introduce the semen into the uterus at the most appropriate time: just when the woman has ovulated. If the woman ovulates correctly, IUI can be done in a natural cycle, that is, without hormonal medication.
- Semen Thawing
- the sperm sample from the donor bank is thawed in the laboratory and it is verified that the spermatozoa have survived. Next, a REM seminogram is done and the most suitable amount of sample for insemination is calculated.
- Artificial insemination
- refers to the act of introducing the donor's semen into the woman's uterus through an insemination cannula. It is a very simple process that can be done in the gynecologist's own office and without the need for anesthesia.
If you want more detailed information about artificial insemination step by step, you can consult the following article: Artificial insemination process.
Choosing the sperm donor
In the USA you can chose your sperm donor, perhaps someone you know, or opt for an anonymous donor. However, in many countries, you cannot and it is the clinic itself that is responsible for donor selection.
When the sperm donor is anonymous, the woman who is going to undergo an IAD does not intervene in the selection of the donor. In the same way, the donor will not know the identity of the woman or couple who receives his sperm.
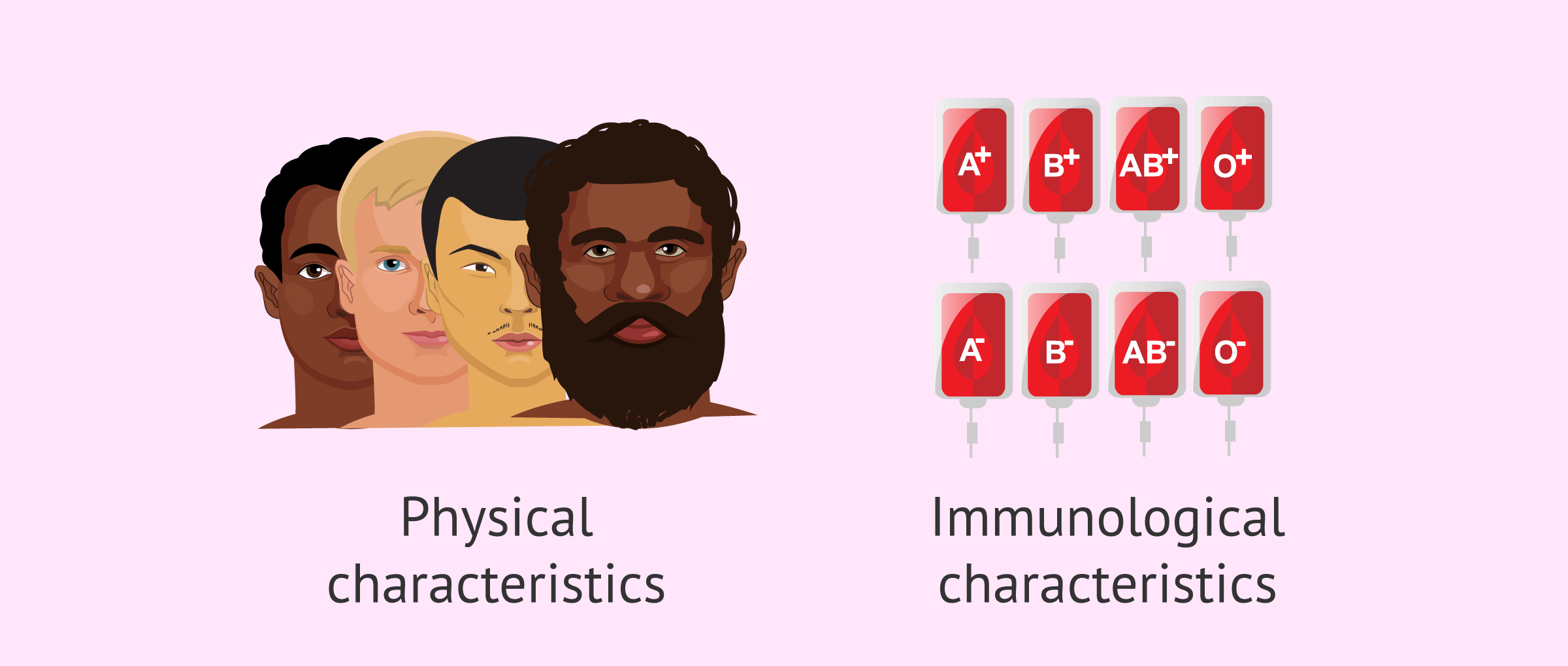
The clinic chooses the most suitable donor based on their physical and immunological characteristics: blood group, race, skin color, physical complexion, height, hair color, eye color, etc. etc. For this reason, the woman receiving the seminal sample will receive general data from the donor, but at no time will they be identified to guarantee her anonymity.
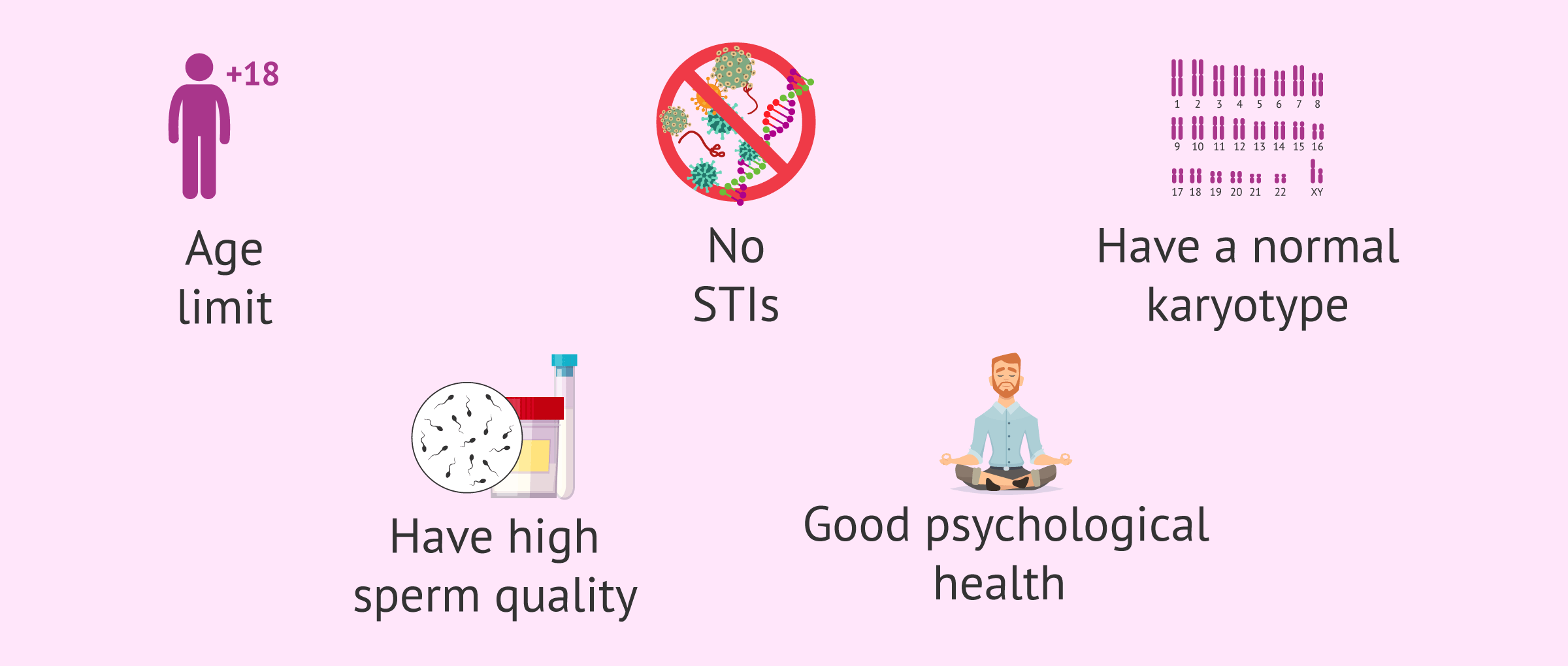
In addition, in order for a man to be a sperm donor, he must meet a series of requirements and pass some medical and psychological tests that show that he is healthy. Some of the requirements that a potential sperm donor candidate must meet are the following:
- Be between 15 and 35 years old.
- Do not suffer from any sexually transmitted infection.
- Do not have a history of genetic diseases and have a normal karyotype.
- Good seminal quality with values higher than the reference values established by the World Health Organization (WHO).
On the other hand, potential sperm donors must be in good psychological health and be of sound mind.
The criteria for selecting gamete donors are very strict and not all those who volunteer are finally accepted. The clinics only accept 1 donor out of 10 candidates.
If you are interested in reading more about this topic, you can access the following post: Selection of the sperm donor.
Advantages and disadvantages of donor IUI
Like any reproductive technique, donor IUI has certain advantages and disadvantages. The following sections detail each of them.
Advantages
Donor artificial insemination, like conjugal artificial insemination, has a series of benefits for the woman or the couple who decides to undergo this treatment. Each of them is listed below:
- Very simple and inexpensive technique.
- Assisted reproduction procedure that is closest to the natural conception, since there is no intervention in the selection of the sperm and fertilization takes place within the woman's body.
- Reproductive technique that is painless and does not require anesthesia, so the risk is low and the patient feels calmer.
- By performing ovarian stimulation, it is possible to control the exact moment of ovulation, which increases the probability of success compared to directed intercourse.
- The required ovarian stimulation is mild, that is, low hormonal doses are used, thus reducing the side effects associated with these drugs.
- Increased pregnancy rate compared to partner IUI, since the quality of donor sperm is very good.
- It allows single women and couples formed by two women to become mothers.
For further information, we recommend you visit the following article: Advantages of artificial insemination.
Disadvantages
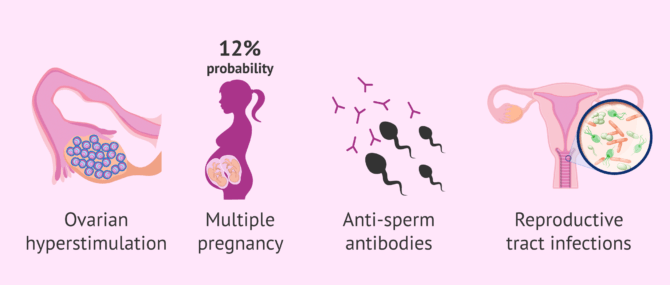
Despite these benefits, donor artificial insemination can also give rise to a number of complications, albeit very rarely. Some of these complications may be the following:
- Ovarian hyperstimulation syndrome (minimal risk due to very low doses of medication).
- Multiple pregnancy (in 12% of cases).
- Allergies to the components of the seminal fluid (very rare).
- Immune reactions by creating antisperm antibodies (probability less than 5%)
- Infections in the reproductive tract (the risk is also very low).
In addition, another negative aspect of IUI, both with partner sperm and donor sperm, is the low probability of success in cases of severe infertility or when the woman is of advanced maternal age.
On the other hand, using donor sperm implies the renunciation of genetic inheritance, something that not all men are capable of accepting.
We recommend you continue reading in the following post to obtain more information on this topic: Risks and consequences of artificial insemination.
Success rates
Generally, better results are obtained with donor insemination than using the partner's semen, since the donors are always young men who have extraordinary seminal quality.
However, one of the most important factors to ensure the success of intrauterine insemination is the age of the woman. As we see below, the delivery rates per cycle of artificial insemination is better when using donor sperm, but in women under 40 years of age:
- Women <35 years old
- 11,3% delivery rate with partner sperm and 19,5% delivery rate with donor sperm
- Women 35-39 years old
- delivery rate of 9,4% with partner sperm and delivery rate of 13.9% with donor sperm
- Women ≥ 40 years old
- delivery rate of 3,3% with the partner sperm and delivery rate of 5.8% with donor sperm.
These data have been obtained from the latest report published by the Spanish Fertility Society (SEF) with the results obtained by the Spanish centers in 2021 (National Activity Register 2021-SEF Register).
Furthermore, the success rate of artificial insemination is cumulative. For this reason, after a failed donor IUI, it is advisable to carry out more inseminations, since the chances of pregnancy increase up to four attempts.
In the case of single women and lesbian couples, it is recommended to make up to a maximum of 6 IUI attempts to achieve pregnancy, unless there is some cause of infertility that indicates otherwise.
For more information on success rates with IUI treatment, you can click here: What is the probability of success with artificial insemination?
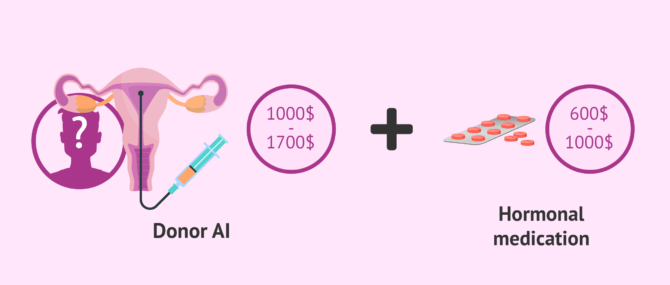
Price of donor intrauterine insemination
Assisted Reproduction Techniques establish that a semen donation is an altruistic act. However, it is true that sperm donors receive financial compensation.
For this reason, artificial insemination with donor sperm has a higher price than with partner sperm, since it is necessary to cover the expenses involved in the tests carried out on the donor and the cost of storing the frozen sample.
Depending on the assisted reproduction clinic and the city in which it is located, the price of the donor insemination in the USA is between $1,000 and $1,700.
Hormonal medication for ovarian stimulation must also be added to this cost since it is not usually included in the initial IUI estimate. The price of these drugs is usually around $1000, depending on the indicated dose by the gynecologist.
Due to the variation in the price of the intrauterine insemination between the clinics, the best thing to do before starting the process is to consult the budget and be clear about which aspects are included and which are not, as well as if they have discounts for a second or third attempt in case pregnancy is not achieved at first.
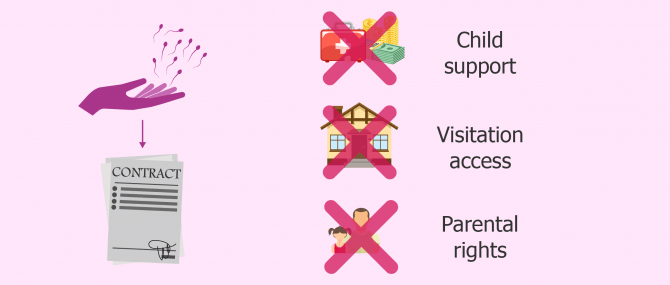
Sperm donor agreement
A sperm donor agreement is a contract signed by both the intended parents and the sperm donor, without using a sperm bank as an intermediary. In spite of the excitement of planning parenthood, and regardless of the family type, all patients should have one in order for the role of each party to be clear.
The following are the different types of sperm donor profiles that can be found, depending on each country's regulations on third-party reproduction:
- Anonymous donor: identifying information about the donor is confidential, and only the sperm bank or fertility clinic has access to it. The intended parents cannot meet him or vice versa.
- Non-anonymous or known donor: The man contributing his sperm cells is known to the prospective parents (name, address, phone number...), who can get touch with him or allow him to have a co-parenting role if they wish to.
If known sperm donation is the option of choice, it is strongly advisable to sign a sperm donor agreement to make it clear the donor—even if he is a member of the family—cannot seek parental or legal rights over the child born as a result of his donation, including visitation and child support.
Sperm donor agreements are expected to include the following aspects: financial responsibilities, legal parenting rights, visitation rights, the relationship between the donor and the child, when will the child know about the donation, what will the child call him, etc.
Video on donor artificial insemination
In the following video, Michelle Emblenton, a biochemist at inviTRA, explains in detail all the aspects related to artificial insemination with donor sperm:
Artificial insemination, also known as intrauterine insemination, is a fairly simple assisted reproduction technique, whereby the artificial insemination is performed with donor sperm.
FAQs from users
Can I be a single mother using a friend's semen?
In the United States, the Food & Drug Administration (FDA) oversees the use of egg, sperm, and embryo donation. As a result, all donations must comply with FDA guidelines. In the circumstance of a “known” sperm donor, the friend donating must undergo a physical examination, infectious disease blood testing, psychological evaluation, and cryopreservation (freezing of the sperm) within seven days of blood work. Further, we require legal contracts between the parties prior to sperm insemination.
How many donor IUI attempts are recommended?
The recommended number of attempts is variable, although we can establish a recommendation of between 3 and 6 attempts. However, this number will be mainly conditioned by the patient's age. We do not recommend this technique after the age of 38-40 years, since, after that age, the poor oocyte quality that is assumed decreases the chances of success with this technique.
How difficult is it to achieve successful donor artificial insemination in women in their 40s?
After the age of 40, women have a considerable increase in the probability of transmitting chromosomal alterations and therefore a greater probability of miscarriage and of having children with genetic anomalies.
Getting pregnant after the age of 40 through artificial insemination is complicated, but not impossible. However, clinics generally do not perform the treatment after 37 years of age due to the low probability of success.
What is the probability of multiple pregnancy in donor artificial insemination?
During artificial insemination, the woman receives hormonal treatment to stimulate ovarian production and control the exact moment of ovulation. For this reason, the probability of multiple gestation is higher in relation to natural pregnancy.
For this reason, it is important to adequately monitor ovarian development and cancel insemination in case of risk.
The probability of a multiple pregnancy in artificial inseminations with donor sperm is approximately 8% in women over 40 years of age and 12% in women under 40 years of age. In any case, although the risk exists, the process is carried out in such a way that the probability is reduced to a minimum.
The origin of the semen sample does not affect, as the probability of having twins or triplets is the same in donor AI as in conjugal AI in the case of women under 40 years of age (which is the most common in the AI technique).
Is a sperm donor agreement required for donor insemination?
Sperm donor agreements are contracts between the donor and the person or persons seeking to use his sperm for insemination, without turning to a sperm bank.
They are used with the purpose of clearly identifying the intended parents as the legal parents of the child, and to make it clear that the donor has no legal rights or responsibilities of fatherhood over the child despite being the biological father.
Is donor artificial insemination more successful than partner artificial insemination?
The quality of donor sperm is excellent, so the pregnancy rates of artificial insemination with donor sperm are most likely to be higher than those of AIH. Thus, the probability of pregnancy with AIH is between 10 and 13% and that of DAI varies between 10 and 25%, depending on the woman's age.
In any case, as we have mentioned, the result will vary depending on other influential factors such as the characteristics of the woman and the quality of the couple's semen.
How many vials of donor sperm are required for IUI?
It depends on the quality of the semen sample and the type of vial used. If the standard process is followed and it is a high-quality sample, a single vial might be enough for an IUI cycle. Keep in mind that donor samples are of excellent quality.
In accordance with parameters such as quality and quantity, each sperm bank or clinic has a different criteria regarding how many vials should be thawed for each technique.
Is it possible to perform artificial insemination from a known donor?
In Spain, it is not possible, since the law insists that sperm donation must be anonymous and altruistic. However, there are other countries, such as the United States, where the law allows non-anonymous donations.
Recommended reading
As we have discussed throughout the article, women without a male partner are one of the main recipients of artificial insemination treatment with donor sperm. If you would like more information you can visit the following articles:
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
Ballesteros A, Castilla JA, Nadal J, Ruiz, M. Manifiesto de la SEF sobre la donación de gametos en España. Publicado a través de la Sociedad Española de Fertilidad (SEF).
Comisión Nacional de Reproducción Humana Asistida (CNRHA) (2015). Aspectos legales y éticos de la donación. En: Registro Nacional de Donantes de Gametos y Preembriones. Ministerio de Sanidad, Consumo y Bienestar Social de España.
Goldberg JM, Mascha E, Falcone T, Attaran M. Comparison of intrauterine and intracervical insemination with frozen donor sperm: a meta-analysis. Fertil Steril. 1999 Nov; 72(5):792-5.
Ley 14/2006, de 26 de mayo, sobre técnicas de reproducción humana asistida. Jefatura del Estado «BOE» núm. 126, de 27 de mayo de 2006 Referencia: BOE-A-2006-9292
Sociedad Española de Fertilidad (SEF) (febrero de 2012). “Saber más sobre fertilidad y reproducción asistida”. En colaboración con el Ministerio de Sanidad, Política Social e Igualdad del Gobierno de España y el Plan de Calidad para el Sistema Nacional de Salud.
Sociedad Española de Fertilidad. Registro Nacional de Actividad 2019-Registro SEF (ver)
Sociedad Española de Fertilidad (SEF) (2011). Manual de Andrología. Coordinador: Mario Brassesco. EdikaMed, S.L. ISBN: 978-84-7877.
O'Brien P, Vandekerckhove P. Intra-uterine versus cervical insemination of donor sperm for subfertility (Cochrane Review). In: The Cochrane Library, Issue 1, 2001. Oxford: Update Software.
The ESHRE Capri Workshop Group. Intrauterine insemination. Human Reproduction
Update, 2009; 15 (3): 265–277.64
FAQs from users: 'Can I be a single mother using a friend's semen?', 'How many donor IUI attempts are recommended?', 'What is the average cost of IUI with donor sperm?', 'How difficult is it to achieve successful donor artificial insemination in women in their 40s?', 'Donor insemination vs. donor-sperm IVF, what are the main differences?', 'What is the probability of multiple pregnancy in donor artificial insemination?', 'What does artificial insemination by donor consist of?', 'How successful is intrauterine insemination (IUI) with donor sperm?', 'Can I give IUI with donor sperm a try after a failed IVF?', 'Is a sperm donor agreement required for donor insemination?', 'Is donor artificial insemination more successful than partner artificial insemination?', 'Is there any difference between artificial insemination by donor and IUI with the patient’s semen?', 'What are the advantages and disadvantages of donor sperm intrauterine insemination (IUI)?', 'How does intrauterine insemination (IUI) with donor sperm work?', 'How many vials of donor sperm are required for IUI?', 'Is natural insemination with a sperm donor legal?', 'How many IUI cycles with donor sperm before success?', 'Is it possible to perform artificial insemination from a known donor?', 'How long does artificial insemination treatment with donor sperm take?', 'When is donor sperm intrauterine insemination (IUI) recommended?', 'How early will I feel pregnancy symptoms after donor insemination?', 'Are there any risks such as side effects or infections in artificial insemination by donor?', 'How much does intrauterine insemination (IUI) with donor sperm cost?', 'What is a sperm donor agreement?', 'How many donor intrauterine insemination (IUI) attempts should we try?' and 'How successful is donor intrauterine insemination (IUI) for women over 40?'.
Authors and contributors


More information about Michelle Lorraine Embleton








Hey there!
Hubby and I have been ttc for over 4 years… but no baby 🙁 We’ve decided now to move to donor sperm… we’re scared but full of hope now… My husband has been diagnosed with azoospermia, and even with ICSI no sperm has been able to fertilize my eggs 🙁 What could be done to maximize our chances?
Thanks
Hello Sonya,
If you have no fertility issue, your egg supply is good and have tubal patency, there should be no problem. However, sometimes, embryos are unable to implant for a number of reasons. So even if all these requirements are met, chances for pregnancy are not 100%.
Wishing you the best of luck!