Artificial insemination or intrauterine insemination (IUI) is a simple technique, and therefore the number of risks associated is low. Nonetheless, one of the most concerning ones is related to the increased likelihood of having twins since a multiple pregnancy carries a greater number of complications than a singleton pregnancy for both the mother and the fetus.
Throughout this article, you can find information on this and other mild risks associated with intrauterine insemination.
Provided below is an index with the 10 points we are going to expand on in this article.
- 1.
- 2.
- 2.1.
- 2.2.
- 3.
- 4.
- 5.
- 6.
- 7.
- 7.1.
- 7.2.
- 7.3.
- 7.4.
- 7.5.
- 7.6.
- 7.7.
- 8.
- 9.
- 10.
Potential complications
With the latest advancements in the field of Reproductive Medicine, we have witnessed a major decrease in the number of risks associated with fertility treatments. In spite of that, there are still some things one should keep a close eye on to avoid potential complications.
Intrauterine insemination (IUI) is a very simple technique. Moreover, it is carried out quickly and safely. But, sometimes, complications can arise, and it is important that patients are well informed about the risks associated before getting started.
Did you know that we can help you to choose a fertility clinic for your IUI cycle? All you have to do is get your Fertility Report now. It is an easy-to-use tool that is capable of filtering the best clinics and tailor an individual report exclusively for you with useful tips that will help you make a well informed decision.
In IUI cycles, complications can appear at any of the following stages of the procedure:
- Side effects of ovarian stimulation drugs
- Risks derived from the insemination procedure
- Pregnancy complications
We will discuss each of these potential AI risks in more detail below.
Risks of ovarian stimulation
Although IUI involves just a mild ovarian stimulation cycle that is closely monitored so that only one or two eggs mature, ovarian response varies from woman to woman. For this reason, in some cases, this response is an excessive one, which can lead to complications like:
Multiple pregnancy
When more than one follicle matures, the risk of multiple pregnancy increases. Particularly, the chances of getting pregnant with multiples ranges between 12 to 30% approximately, being especially common in these cases:
- Young women
- Women with more than 5 ovarian follicles larger than 16 mm
- Women inseminated with high-quality sperm (over 30 million sperm/ml)
As explained above, getting pregnant with multiples or more is a dangerous situation for both the health of the mother and the babies. In cases of advanced maternal age, a twin pregnancy could entail even more risks.
To get more data about the potential risks of a twin pregnancy, click here: What Are the Risks of a Multiple Pregnancy?
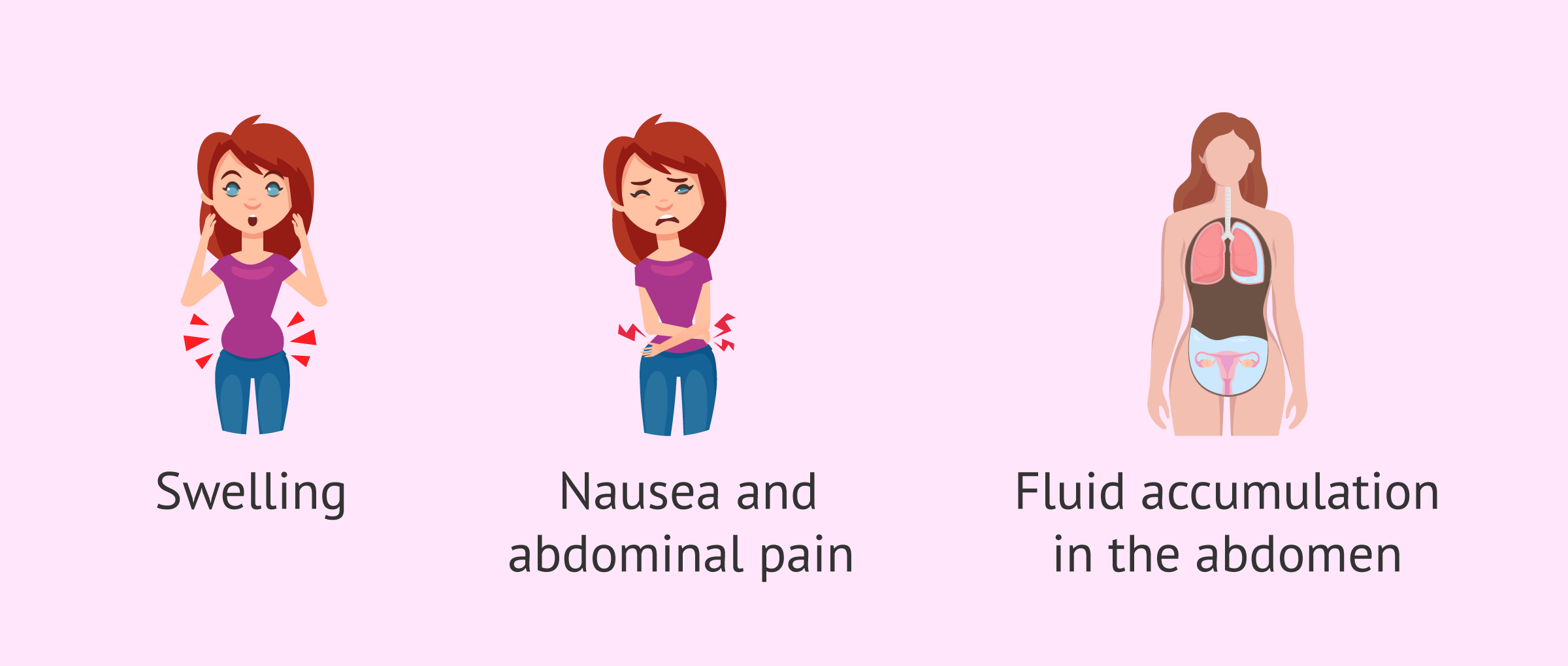
Ovarian hyperstimulation syndrome (OHSS)
It occurs when the ovary gives an exaggerated response to hormone medications, which increases permeability of blood vessels and fluid extravasation. Some potential effects include:
- Swollen ovary and abdomen
- Bloating
- Nausea and/or dizziness
- Acute pelvic pain
- Accumulation of fluid in the abdomen
In addition, in the most severe cases of OHSS, liver, renal and respiratory disorders may also occur.
However, ovarian hyperstimulation syndrome is very rare in AI and may occur more frequently in other assisted reproductive techniques such as IVF (in vitro fertilization), since higher doses of hormones are used for stimulation.
Risks of insemination
When the insemination procedure is carried out at the doctor's office, the following complications may occur:
- Vaginal or pelvic infections
- Due to the use of lab instruments or remainder of seminal plasma. They occur in about 0.07% of the cases per insemination cycle.
- Allergic reactions
- Although it is very rare, some women develop allergies to some componentes of the seminal washing.
- Immune reactions
- Some women are allergic to the semen due to the presence of antisperm antibodies in the vaginal discharge. The likelihood is lower than 5%.
These risks occur very rarely and, if any of them appears, the effects are mild.
Risks of pregnancy
Complications derived from pregnancy after intrauterine insemination are:
- Miscarriage
- It is more common in the first weeks of pregnancy. The miscarriage rate ranges between 20 and 22%.
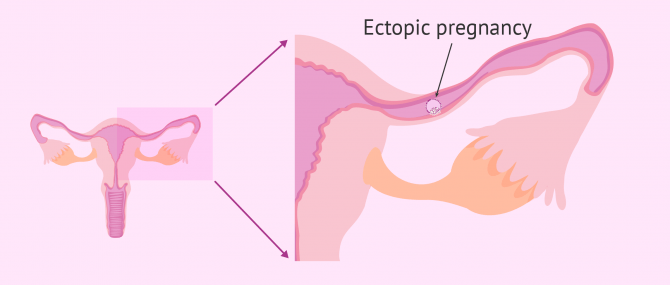
- Ectopic pregnancy
- Embryo implantation occurs in a place other than the womb. In IUI procedures, the chances for an ectopic pregnancy increase because the semen is inserted into the uterus directly. The occurrence rate is 4%, while in natural pregnancies it occurs in 0.8% of the cases.
- Multiple birth
- Either naturally (identical twins) or after the fertilization of multiple oocytes (fraternal twins), it is considered a high-risk pregnancy, as explained above.
An ectopic or multiple pregnancies can occur naturally as well, though the rate is considerably lower. On the contrary, a miscarriage is an event that occurs in natural pregnancies more often than one might think since sometimes it occurs when the woman has not even realized she was pregnant.
Risks of home artificial insemination
When it is a home artificial insemination, there are no possible consequences derived from ovarian stimulation, since the woman is not administered hormonal medication. However, the risks derived from the insemination itself are the same.
On the other hand, one of the main risks of performing a home artificial insemination refers to the origin of the semen. When intrauterine insemination is performed in a fertility clinic, the sperm sample is previously analyzed. On the contrary, when the insemination is performed at home, the sperm is introduced directly, without analysis or processing.
In the case of using a sperm bank to perform a donor artificial insemination at home, it is essential that the bank is approved and accredited for this purpose. In addition, it is important to be well informed about the tests required for donors and the quality controls of the semen samples.
Finally, there may also be problems due to inexperience, since it is possible that the insemination may tear the vagina or cause damage to the female reproductive system.
Cancellation of an IUI cycle
Although it is rare, sometimes the patient's response to ovarian stimulation medications is not the one expected. Some women have an exaggerated response to treatment, which causes the ovary to develop excessively, increasing the risks of getting pregnant with twins, and developing OHSS.
During ultrasound monitoring visits, your doctor will measure the size of your follicles, which is an indicator of how mature the egg is. If you see more than 2 large follicles (more than 16 mm), it is recommended that the cycle is canceled, since the likelihood of ovulating multiple eggs is high, which can lead to multiple births.
Also, hormone medications do not work in some women, or their response is too poor. If the specialist considers that the egg is not maturing adequately, it is likely that ovulation does not occur, or that an immature egg is released. This would lead to the creation of a non-viable embryo after fertilization.
Depending on the impressions provided by the specialist during ultrasound scan visits, he or she will determine whether performing the insemination is worth it, or if the best option would be to cancel the cycle and try again in the next cycle, perhaps with a greater dose of medication, or a different medication protocol.
FAQs from users
Am I prone to ovarian hyperstimulation during AI as a PCOS patient?
It is very rare for an ovarian hyperstimulation syndrome to occur in an artificial insemination treatment, as low doses of medication are usually used. The aim is to achieve growth of between 1 and 4 follicles at most.
Read more
Can multiple pregnancy in AI be avoided if three ovarian follicles have developed?
Yes, indeed, it can and should be avoided. Multiple pregnancy, in the past, was a complication that fortunately today has been overcome thanks to the progress and study of human assisted reproductive techniques. Nowadays, it is not advisable to maintain a cycle with a high risk of multiple pregnancy.
In the case in question, if during the course of ovarian stimulation three or more follicles develop, the situation will be redirected to maintain the stimulation and the ovarian puncture will be programmed to extract and fertilize the eggs obtained in the laboratory and carry out the transfer of the embryos in successive deferred cycles.
How does age affect success of intrauterine insemination? Is there an age limit?
For artificial insemination to be successful and pregnancy can be achieved, it is necessary for the woman to have a normal ovarian reserve and be able to ovulate naturally, either spontaneously or with the help of hormone medications.
For this reason, in general, women aged more than 37 years are rarely referred to IUI, since the ovarian reserve starts diminishing from age 35 onwards until its complete depletion between 45 and 55.
Another basic requirement for the patient, regardless of whether she is undergoing AIH or AID, is having tubal patency in at least one tube.
What are the potential complications of artificial insemination?
As explained above, AI is a simple procedure, and therefore the likelihood of problems to occur is low. However, it involves a previous process of ovarian stimulation that can lead to negative effects such as multiple births, with a greater number of risks than a singleton pregnancy, or the ovarian hyperstimulation syndrome (OHSS) due to an exaggerated response to fertility drugs.
Some women develop allergy or infections as well.
In any case, AI is a safe technique that is done under supervision to reduce the chance of complications to the minimum.
Can children born by IUI experience developmental problems?
IUI is a method to achieve pregnancy. Once this goal is met, the stages and development of the pregnancy is exactly the same as if achieved naturally. Also, there is no reason for the development and education of the child born as a result to be different.
Is the miscarriage rate associated with IUI higher than in natural pregnancies?
The chances of having a natural miscarriage in young women range between 12 and 15%, and they increase to 25% in women older than 40 years old. In cases of IUI, where the woman is typically younger than 37 years old, the miscarriage rate is about 20%. Thus, the answer is yes, the risk of miscarrying is slightly higher.
Which has more complications associated, AIH or AID?
The complications associated with AI are the same irrespective of the type chosen. In other words, the origin of the sample does not increase the risk of complications. Thus, the potential risks associated are the same in cases of artificial insemination by donor (AID) and by husband (AIH).
Suggested readings
Throughout this post, we have seen that home insemination carries a greater number of risks than clinical insemination. However, since we skip the ovarian stimulation step when doing it at home, the potential complications associated with fertility drugs are removed, too. Simultaneously, the fact that there is no stimulation reduces the chances of success as well. In short, if you want to get a much deeper insight into DIY insemination, read: What Is Artificial Insemination at Home? – Process Step by Step.
Also, we recommend that you get more info on the intrauterine insemination process with this comprehensive guide in order to understand more clearly the potential risks and complications involved: What Is Artificial Insemination (AI)? – Process, Cost & Types.
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
Allen NC, Herbert CM 3rd, Maxson WS, Rogers BJ, Diamond MP, Wentz AC. Intrauterine insemination: a critical review. Fertil Steril. 1985 Nov;44(5):569-80. (Ver)
Chaabane S, Sheehy O, Monnier P, Fraser W, Bissonnette F, Trasler JM, Muanda FT, Boukhris T, Karam F, Santos F, Blais L, Bérard A. Ovarian Stimulation, Intrauterine Insemination, Multiple Pregnancy and Major Congenital Malformations: A Systematic Review and Meta- Analysis- The ART_Rev Study. Curr Drug Saf. 2016;11(3):222-61. (Ver)
Evans MB, Stentz NC, Richter KS, Schexnayder B, Connell M, Healy MW, Devine K, Widra E, Stillman R, DeCherney AH, Hill MJ. Mature Follicle Count and Multiple Gestation Risk Based on Patient Age in Intrauterine Insemination Cycles With Ovarian Stimulation. Obstet Gynecol. 2020 May;135(5):1005-1014. (Ver)
Goldfarb JM, Peskin B, Austin C, Lisbona H. Evaluation of predictive factors for multiple pregnancies during gonadotropin/IUI treatment. J Assist Reprod Genet. 1997 Feb;14(2):88-91. (Ver)
Hurd WW, Randolph JF Jr, Ansbacher R, Menge AC, Ohl DA, Brown AN. Comparison of intracervical, intrauterine, and intratubal techniques for donor insemination. Fertil Steril. 1993 Feb;59(2):339-42. (Ver)
Matorras R, Rubio K, Iglesias M, Vara I, Expósito A. Risk of pelvic inflammatory disease after intrauterine insemination: a systematic review. Reprod Biomed Online. 2018 Feb;36(2):164-171. (Ver)
Nuojua-Huttunen S, Tomas C, Bloigu R, Tuomivaara L, Martikainen H. Intrauterine insemination treatment in subfertility: an analysis of factors affecting outcome. Hum Reprod. 1999 Mar;14(3):698-703. (Ver)
Plosker SM, Jacobson W, Amato P. Predicting and optimizing success in an intra-uterine insemination programme. Hum Reprod. 1994 Nov;9(11):2014-21. (Ver)
Rowell P, Braude P. Assisted conception. I--General principles. BMJ. 2003 Oct 4;327(7418):799-801. (Ver)
Starosta A, Gordon CE, Hornstein MD. Predictive factors for intrauterine insemination outcomes: a review. Fertil Res Pract. 2020 Dec 11;6(1):23. (Ver)
Van Voorhis BJ, Sparks AE, Allen BD, Stovall DW, Syrop CH, Chapler FK. Cost-effectiveness of infertility treatments: a cohort study. Fertil Steril. 1997 May;67(5):830-6. (Ver)
Zayed F, Lenton EA, Cooke ID. Comparison between stimulated in-vitro fertilization and stimulated intrauterine insemination for the treatment of unexplained and mild male factor infertility. Hum Reprod. 1997 Nov;12(11):2408-13. (Ver)
FAQs from users: 'Am I prone to ovarian hyperstimulation during AI as a PCOS patient?', 'Can multiple pregnancy in AI be avoided if three ovarian follicles have developed?', 'How does age affect success of intrauterine insemination? Is there an age limit?', 'What are the potential complications of artificial insemination?', 'Can children born by IUI experience developmental problems?', 'Is the miscarriage rate associated with IUI higher than in natural pregnancies?' and 'Which has more complications associated, AIH or AID?'.
Authors and contributors

More information about Cristina Algarra Goosman








Hello, my partner and I want to become mothers and I would like to know if this treatment can be done with donor sperm, is it the right one?
Hi Tedy,
Artificial Insemination can be done with either partner sperm or donor sperm. In your case, if there is no problem with the reproductive system of the intended mother. If there is any kind of problem, IVF can be performed with donor sperm.
I leave you with this article where we explain the options to achieve pregnancy: Baby Options for Lesbian Couples with Donor Sperm
I hope I have helped you.
Best regards.