Semen freezing is currently a widely used technique in assisted reproduction centers. It is a simple procedure that allows preserving fertility in men.
Thanks to sperm cryopreservation, sperm that are frozen and stored in sperm banks can be used by assisted reproduction techniques in the future. In addition, these spermatozoa will not see their quality affected nor will they have a storage time limit.
Provided below is an index with the 9 points we are going to expand on in this article.
- 1.
- 1.1.
- 1.2.
- 1.3.
- 2.
- 2.1.
- 3.
- 4.
- 5.
- 5.1.
- 5.2.
- 5.3.
- 6.
- 6.1.
- 6.2.
- 6.3.
- 6.4.
- 6.5.
- 6.6.
- 7.
- 8.
- 9.
What are the indications?
Sperm freezing helps many patients who, without this technique, would not be able to become parents in the future. For this reason, semen cryopreservation is performed in cases such as those mentioned below.
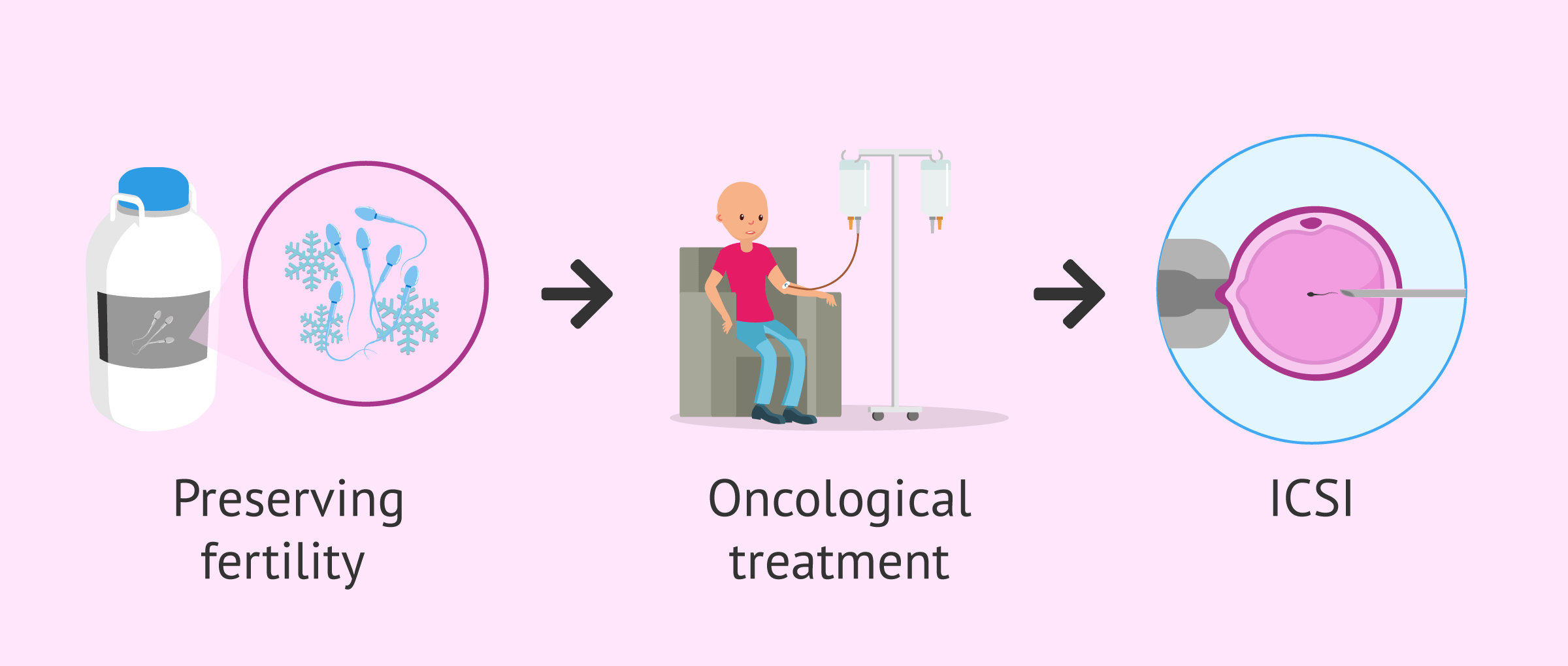
Oncology patients
Sperm freezing makes it possible to preserve fertility in patients who are likely to lose it due to chemotherapy or radiotherapy treatments. In these patients, it is necessary that the samples be frozen before starting the treatment, since, once started, the seminal quality can be altered and entail dangers for future generations.
Therefore, the patient's reproductive capacity may be reduced after cancer treatment. In these cases, previously frozen semen samples may be used in assisted reproduction techniques to search for a pregnancy. In this way, these men will be able to become fathers once the disease has been overcome, despite the effects that the oncological treatment may have had on their fertility.
You can continue reading more information on this topic in the following article: How does Cancer affect fertility in Men and Women?
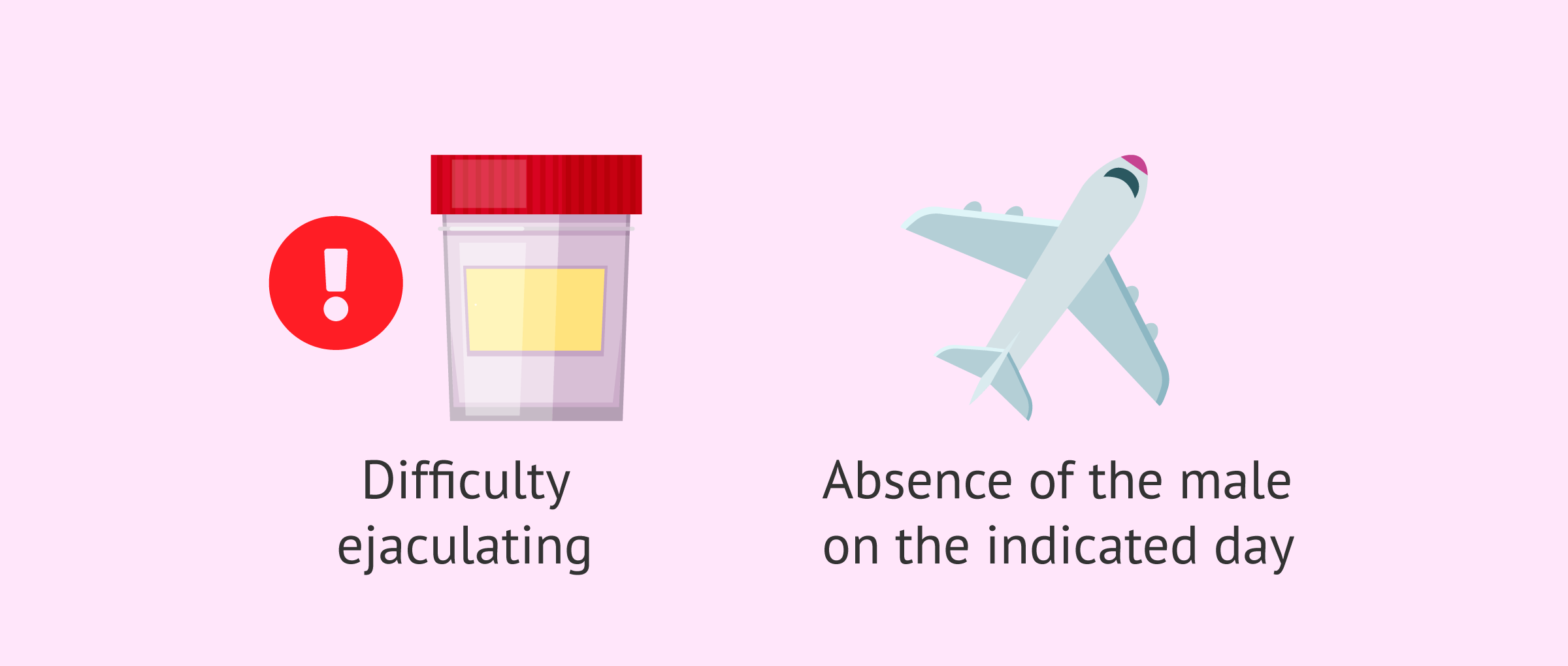
Patients with difficulties in obtaining the sample
Some men have limitations when submitting the seminal sample on the day of artificial insemination (AI) or in vitro fertilization (IVF). Freezing sperm beforehand allows assisted reproduction treatments to be handled more comfortably when this type of situation occurs.
For example, freezing semen would be useful in patients with difficulties ejaculating due to psychological blockage. This technique would also be very useful for those patients who cannot attend the fertility clinic because their place of residence is far away (especially in cases of egg donation).
In addition, sperm cryopreservation also makes it possible to optimize the use of valuable semen samples. These types of samples are those obtained by testicular biopsy or epididymal aspiration, semen washes from seropositive men, or samples from cancer patients. In this way, the seminal samples can be dosed and used little by little, as required.
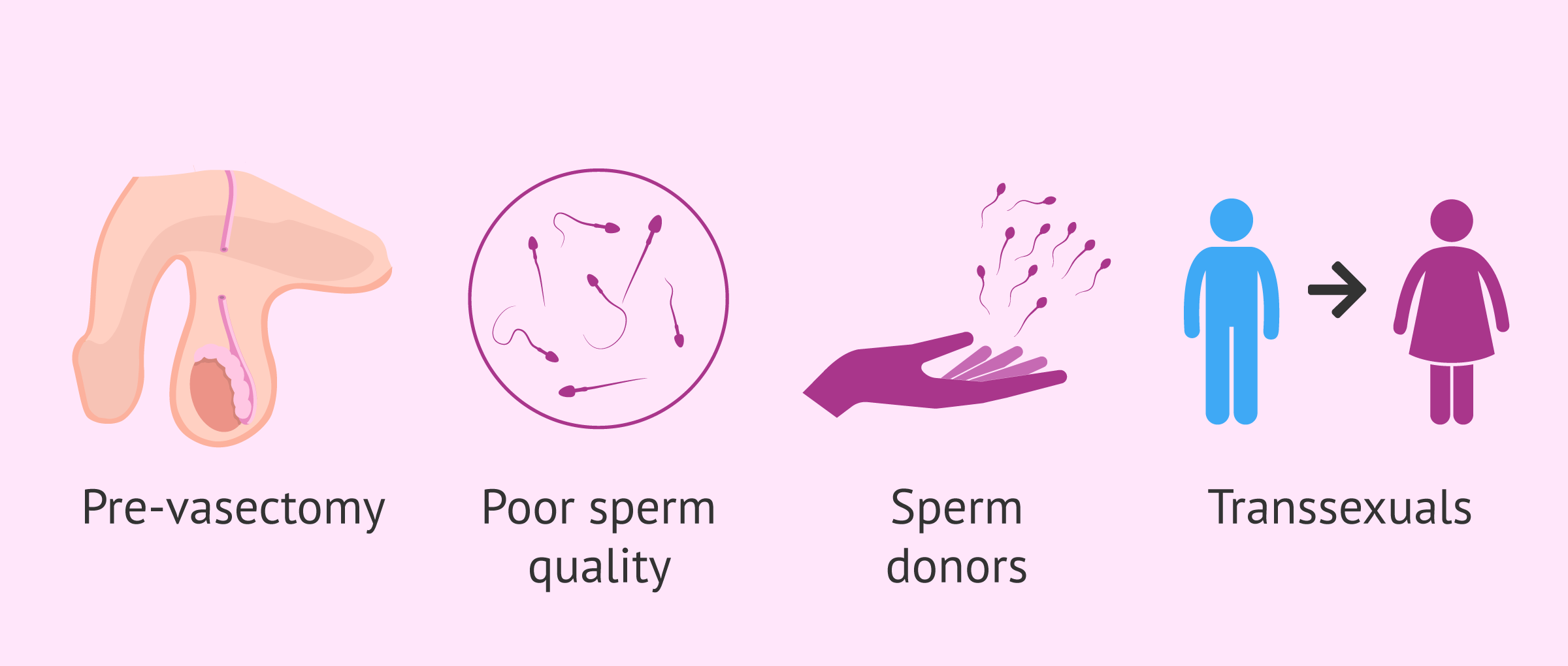
Other indications
Freezing some semen samples is highly recommended for patients who are going to have a vasectomy. Having frozen semen will be useful if these patients wish to become parents in the future since it would avoid undergoing a testicular biopsy or by a new intervention to have offspring with their own sperm.
On the other hand, in patients with very low sperm quality, it is advisable to freeze semen samples prior to starting assisted reproduction treatment. In these cases, the purpose of freezing the semen is to ensure that on the day of the follicular puncture there will be sperm available to fertilize the ovules obtained.
As for sperm donors, it is essential that semen samples be frozen. Spanish legislation requires that a series of analyzes be carried out before being used, to ensure that they do not transmit any disease. In this way, sperm cryopreservation allows time to confirm the absence of HIV infection in donated samples.
Finally, transsexuals who are going to undergo sex transition surgery can also cryopreserve their sperm in case they decide to use it in the future.
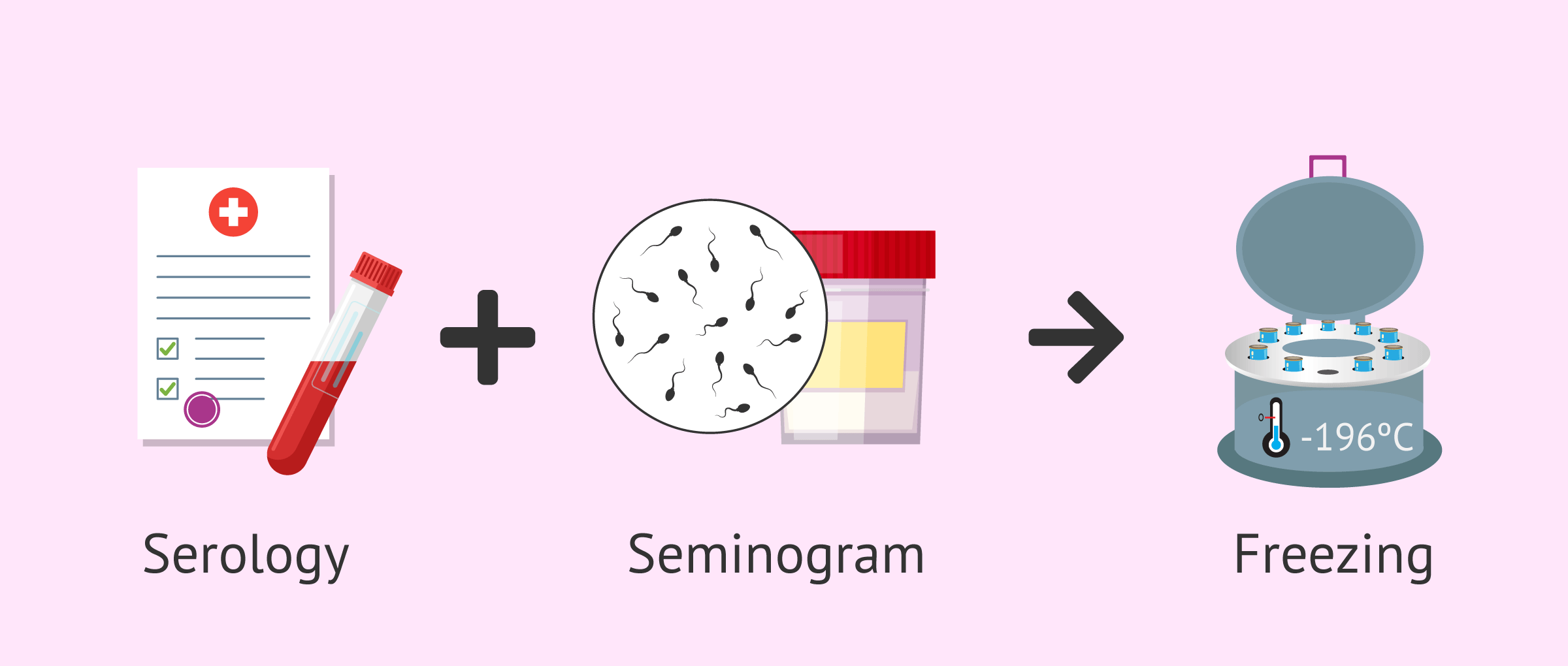
Semen freezing
Sperm freezing is a routine and simple technique that is performed in any assisted reproduction laboratory. However, it is necessary that before freezing the semen the patient provides updated serologies. In this way, it is guaranteed that the safety of the rest of the samples in the laboratory is not compromised.
In addition, it is also essential to assess seminal quality by means of a seminogram before performing this technique. Seminal quality will be the main factor that will determine the viability of the sample once it is thawed.
However, the only essential requirement to perform semen freezing is that motile spermatozoa are found in the ejaculate.
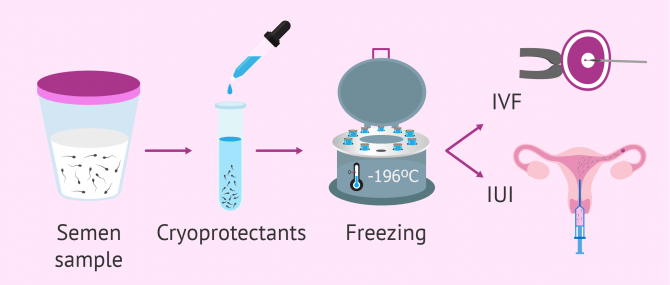
Sperm freezing process
Generally, sperm cryopreservation is carried out through a slow freezing process that consists of:
- Addition of cryoprotective agents to the seminal sample, to prevent cell damage to the spermatozoa.
- Introduction of the seminal sample in cryotubes or straws.
- Gradual drop in temperature.
- Storage of cryotubes or straws in liquid nitrogen, at -196ºC.
It is important to note that it is during the freezing and thawing processes that sperm can be damaged. During storage, the seminal quality does not change.
For valuable semen samples, semen freezing can be done on small beads. In this way, the use of these is optimized, since it is possible to thaw only a small amount of seminal sample each time it is necessary.
Results obtained with frozen semen
In good quality semen samples, some sperm parameters may be altered after thawing (such as the number of live sperm or sperm motility). Despite this, freezing semen will not reduce the chances of success of the treatment.
However, if the quality of the semen sample is poor, the alterations in the sperm parameters will be more pronounced. Therefore, for those assisted reproduction techniques in which a certain concentration of motile sperm is needed (such as artificial insemination or IA), the results may be compromised with sperm freezing.
However, with the intracytoplasmic sperm microinjection (ICSI) technique, in which only one sperm is required for each egg to be fertilized, these patients can be helped to seek pregnancy.
If you are considering freezing your sperm to have a child in the future, we recommend that you start by creating a Fertility Report. In 3 simple steps, it will show you a list of clinics that fit your preferences and meet our strict quality criteria. Moreover, you will receive a report via email with useful tips to visit a fertility clinic for the first time.
Interview with Dr. Antonio Alcaide
In high-quality samples, although some sperm parameters can be altered after the thawing process (such as the number of live sperm or sperm motility), in general, this technique does not affect the success rates of fertility treatments.
Neither does age. According to Antonio Alcaide Raya, PhD, in the case of semen, age is not a determining factor to decide whether freezing is good or bad. The most important factor when a man is about to freeze his semen is sperm quality, namely the sperm count and sperm morphology.
However, if sperm quality is bad, the severity of sperm disorders will be higher. For this reason, to carry out a technique that requires a greater sperm count (e.g. IUI), the results may be affected.
Even if some of these parameters are altered, some studies have proven that the results of fertility treatments where ICSI with donor sperm is used are not affected.
Prices
The preservation of male fertility has a more affordable cost than in the case of women. This is mainly due to the fact that the egg vitrification technique is a more complex process. As we have said before, sperm freezing is a much simpler procedure.
Cost in the USA
In the United States, the process can be divided into several phases. The first is the initial visit consultation, which can cost $150. Second, the blood panel (minimum infectious disease testing), the cost is $140. Third, the semen specimen analysis and the semen specimen release (about $500 approximately).
Cost in the UK
The process in UK fertility clinics is similar to the one followed in the USA, and includes these phases:
- Semen freezing: £300
- Subsequent semen samples: £200
- Multiple sample package: £850
Cost in Canada
The total cost of freezing sperm in Canada can be $600 CAD. Firstly, a fertility clinic can charge you for a counseling or orientation session up to $250 CAD. Then, the semen preparation process can run you about $200 CAD. Finally, the cost of storing the sperm is usually $200 CAD per year.
FAQs from users
Should men freeze their sperm to preserve their fertility?
Although there exists different studies that relate an advanced age with fertility problems, actually it is still unclear.
In the testicle, sperm production is a permanent process, contrary to what happens in with egg production in females. This is the reason why, freezing sperm as a preventive measure is not so useful as in the case of egg freezing, since egg quality and quantity decreases from age 35 onwards.
Unless there exists a disorder that affects sperm production, in the case of cancer patients who are going to undergo chemotherapy or radiotherapy, or if the man undergoes some kind of surgery (such as in the case of vasectomy), freezing sperm for the future is not required.
There exist different fertility preservation options for males who have been diagnosed with cancer. What method is being currently used before undergoing a cancer treatment?
Different to what happens with women, fertility preservation in males is quite simple, since it just involves collecting one or two semen samples. It is crucial that is is done before receiving the first chemotherapy or radiotherapy session. Otherwise, the quality of the sample would be too low. In pre-adolescent boys, a testicular biopsy could be a good option, although it is a highly controversial topic for the moment.
Does using frozen semen affect the result of assisted reproduction treatment?
If we talk about whether the use of a frozen semen sample will affect the results, it will depend on what treatment is going to be carried out and what is the reason why it is decided to use a previously frozen sample and not a fresh sample.
It has been observed that freezing affects, to a greater or lesser extent, the mobility of the sperm, so in cases of severe male factor, the recommendation would be to use fresh semen.
In addition, donor semen samples are frozen (Spanish law does not allow the use of a fresh donor), so the use of frozen semen does not have to worsen the results except in certain particular cases.
On the other hand, the use of frozen samples allows us to have more flexibility when organizing treatments both for the needs of our patients and for the management of daily work in our clinics.
Is it possible to use semen from an international sperm bank?
Yes, as long as it is an anonymous donor and the donor has passed the tests established by the laws in your country and / or state.
How long can frozen sperm be stored?
The time during which the sample remains frozen does not affect sperm quality, which means that we can have the sample frozen for as long as we wish. In fact, there are cases of samples who have been frozen for 22 years and have led to pregnancy, without causing any problem in offspring.
Is there an age limit for men to be able to freeze sperm?
Age does not affect the results of sperm cryopreservation. As explained earlier, the most important factor when it comes to predicting the success of sperm freezing is sperm quality.
Recommended readings
As we have already seen, sperm freezing allows males to preserve their fertility after having received a cancer diagnosis. If you wish to get more details about this option, visit this post: Fertility Preservation – Cost & Options for Retaining Your Fertility.
To get more information about the egg cryopreservation process, click here: What Is Egg Vitrification? – Advantages Over Freezing.
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
WHO Manual for standardized investigation and diagnosis and management of the infertile male. Cambridge: Cambridge University Press, 2000.
Kvist U, Björndahl L. ESHRE Monographs: Manual on Basic Semen Analysis. Oxford: Oxford University Press, 2002.
Reproducción Asistida ORG. Video: Congelación de semen (Sperm freezing), by Antonio Alcaide Raya, PhD, Jan 7, 2016. [See original video in Spanish].
Sigman M, Zini A. (2009). Semen analysis and sperm function assays: what do they mean? Semin Reprod Med; 27: 115-123
Sociedad Española de Fertilidad (SEF) (febrero de 2012). “Saber más sobre fertilidad y reproducción asistida”. En colaboración con el Ministerio de Sanidad, Política Social e Igualdad del Gobierno de España y el Plan de Calidad para el Sistema Nacional de Salud.
Sociedad Española de Fertilidad (SEF) (2011). Manual de Andrología. Coordinador: Mario Brassesco. EdikaMed, S.L. ISBN: 978-84-7877.
FAQs from users: 'Should men freeze their sperm to preserve their fertility?', 'There exist different fertility preservation options for males who have been diagnosed with cancer. What method is being currently used before undergoing a cancer treatment?', 'Does using frozen semen affect the result of assisted reproduction treatment?', 'Is it possible to use semen from an international sperm bank?', 'How long can frozen sperm be stored?' and 'Is there an age limit for men to be able to freeze sperm?'.
Authors and contributors

More information about Cristina Algarra Goosman

More information about Michelle Lorraine Embleton







Hello, I have been diagnosed with cancer and will start treatments soon. In the hospital, they have recommended I freeze sperm if I want to be a father, but I don’t really understand why.
Hi Kyle,
The oncology treatments that are carried out for the treatment of cancer are radioactive, that is, they emit waves that attack the cancer cells. This type of treatment also has a harmful effect on the testicles, it affects the creation of sperm and the quality of the sperm, even altering them permanently. Therefore, before starting the treatment, it is advisable to freeze a sample to ensure that if you want to become a father in the future, you will be able to do so.
I hope this has helped you,
Best of luck
Hello, it does not affect the spermatozoa to be frozen, I would assume that these would die from the cold no?
Hello Jonathan,
Cryopreservation of semen is done by a slow freezing technique, cryoprotective agents are added and it is stored in liquid nitrogen. This allows the semen quality to be preserved and promotes a thawing process that does not damage the sample.
I hope I have helped you
I find it marvelous that semen can be frozen… It’s a very advisable alternative to men suffering from testicular cancer, since it allows them be sure they will be able to be on fatherhood if they want to in the future. Who knows what the future holds?