Sperm morphology is one of the aspects studied in the basic semen analysis or seminogram. Evaluating sperm morphology is used to see how many sperm are found with an abnormal shape and the type of alterations they present.
All men produce abnormally shaped sperm. In fact, in a semen sample considered normal, a large part of the sperm may have an altered morphology.
Despite this, if the seminogram does not find a minimum percentage of sperm with normal morphology, the man is said to have teratozoospermia.
Provided below is an index with the 8 points we are going to expand on in this article.
- 1.
- 1.1.
- 2.
- 3.
- 4.
- 5.
- 5.1.
- 5.2.
- 5.3.
- 5.4.
- 6.
- 7.
- 8.
How do I know if my sperm is normal?
In order to study the morphology of the spermatozoa, a small amount of semen is taken from the total ejaculate of the male. This semen sample is spread, fixed, and stained on a slide to facilitate its observation under the microscope, which implies the death of the spermatozoa. This procedure, therefore, prevents these spermatozoa from being used after evaluation. However, the analysis of this small sample will serve as a proxy for the rest of the semen sample.
Normal sperm morphology
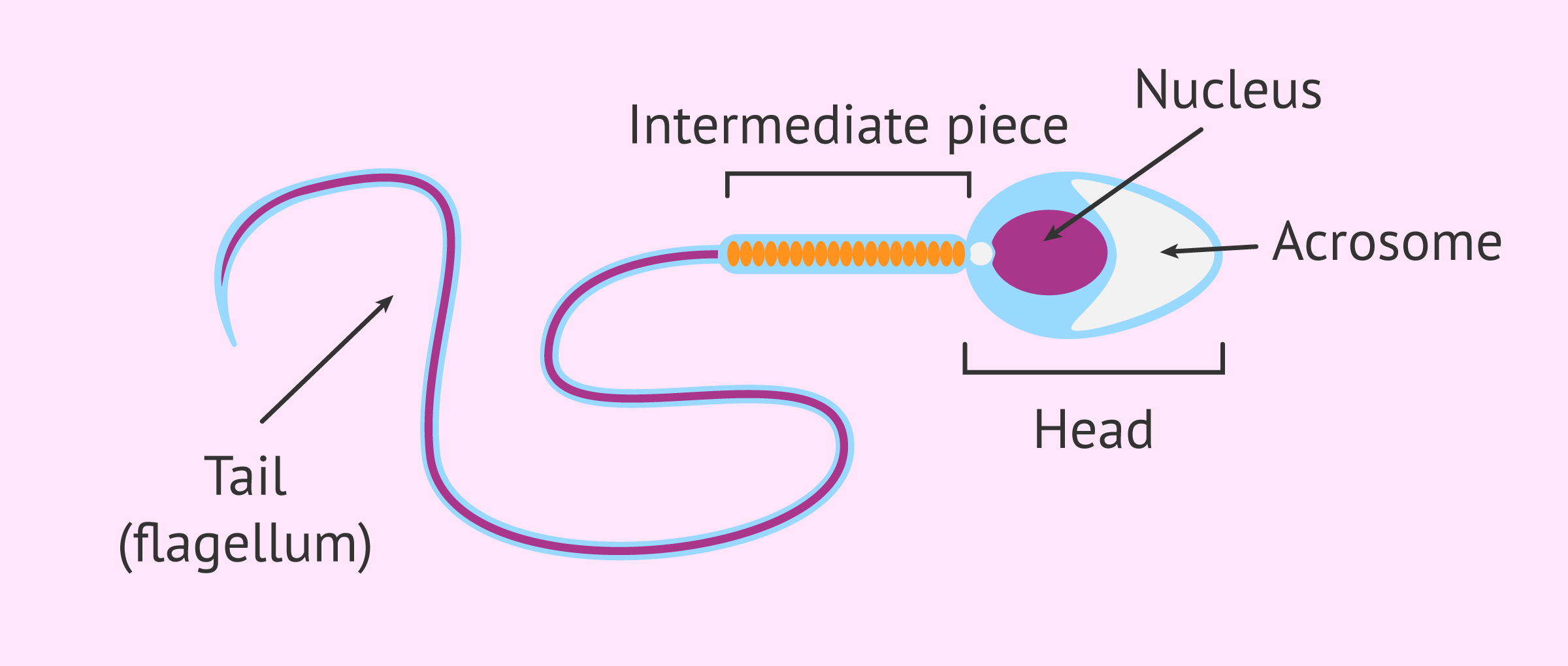
To evaluate the morphology of sperm, its three main structures are observed under a microscope: head, midpiece, and tail. Broadly speaking, the characteristics of sperm with normal morphology are the following:
- The head of the spermatozoon should be oval and smooth, 5 to 6 microns long and 2.5 to 3.5 microns wide. The acrosome should cover 40-70% of the head volume, and if there are vacuoles they should be scarce and occupy less than half of the head volume since if they are numerous or large it may mean that the DNA is damaged.
- The middle piece or neck, as its name indicates, is located between the head and the flagellum, and it is a slightly wider area than the base of the tail. Its function is primordial because it houses the mitochondria, considered the motor of the sperm's movement, as they are responsible for generating energy.
- The flagellum or tail is made up of the same structural molecules responsible for the correct distribution of chromosomes in mitosis and meiosis, so an irregular flagellum will reflect problems in the distribution of chromosomes, and above all, its movement will not be able to compete with the batting of a normal spermatozoon.
In this way, spermatozoa are evaluated individually, taking into account that a spermatozoon must be normal in all its parts to be considered morphologically normal. It should be noted that this evaluation can be subjective and subject to variation.
Generally, 200 spermatozoa are evaluated, noting whether their shape is normal or not. In addition, this evaluation should be done in duplicate. Subsequently, the percentage of spermatozoa with normal shape is calculated and presented in the seminogram results report.
Abnormal spermatozoa: causes and alterations
A high percentage of morphologically abnormal spermatozoa has been related to altered spermatogenesis, as well as to some pathologies of the epididymis.
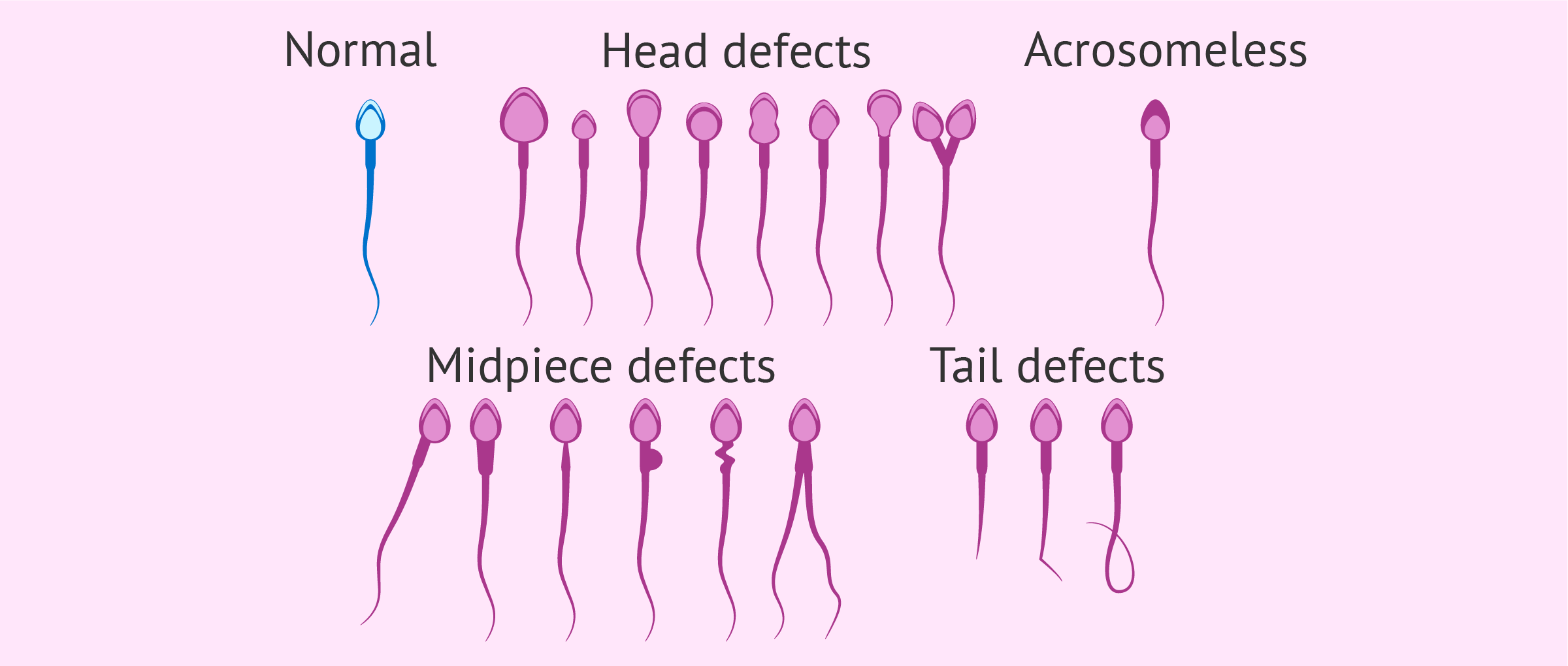
Sperm with abnormal morphology can present defects in any of its parts (or in several). The following alterations can be found in each of the parts of the sperm:
- Head: headless spermatozoa (pinhead), small, amorphous, round, elongated, large, pear-shaped (pyriform) head, with large or small acrosome, vacuolated (with more of 2 vacuoles, vacuoles that occupy more than 20% of the head or with vacuoles in the postacrosomal region) or sperm with two heads.
- Midpiece: asymmetrical, thickened, thin, sharply curved, irregular, or with a bulge larger than one-third of the area of the head.
- Tail: spermatozoa without a tail, short tail, multiple, coiled, broken, bent, with pronounced angles or of irregular thickness.
However, headless or tailless sperm should not be counted, as they are not taken into account in the calculation of sperm concentration.
Abnormal morphology could affect a sperm's ability to fertilize. In addition, abnormal sperm may also have altered DNA.
Normal values
According to the criteria of the World Health Organization (WHO), a quantity equal to or greater than 4% of spermatozoa with normal morphology is considered normal. If the value of abnormal sperm is greater than 96%, that is, there are less than 4% normal sperm, the man has teratozoospermia.
There is another somewhat stricter morphology analysis criterion. This is the Kruger morphology criterion, according to which the limit of normality is 14%. This means that a sample with more than 86% of its sperm abnormal will be considered teratozoospermic.
Is there treatment or is there no solution?
Un hombre cuyos espermatozoides muestran una morfología alterada, es decir, padece de teratozoospermia, puede tener mayores dificultades de conseguir el embarazo de forma natural. Aunque la teratozoospermia no es uno de los problemas seminales más graves, es posible que sea necesario recurrir a la reproducción asistida para poder tener hijos propios, especialmente en los casos de teratozoospermia severe.
If you are considering freezing your sperm to have a child in the future, we recommend that you start by creating a Fertility Report. In 3 simple steps, it will show you a list of clinics that fit your preferences and meet our strict quality criteria. Moreover, you will receive a report via email with useful tips to visit a fertility clinic for the first time.
In milder cases, sperm morphology could be improved with a proper diet, reducing caffeine intake and avoiding tobacco and drugs.
There are also food supplements rich in antioxidants that prevent damage to sperm DNA caused by oxidative stress. These supplements contain vitamins and minerals necessary for proper male reproductive function. However, their benefits have not been scientifically demonstrated in a robust manner.
This is what Dr. Jose Sánchez says:
The most suitable technique is undoubtedly ICSI or intracytoplasmic sperm injection, which consists of selecting the sperm with the best morphology and introducing them into the cytoplasm of the oocyte.
In milder cases, sperm morphology can be improved with an adequate diet, reducing caffeine consumption, and avoiding tobacco and drugs.
There are also specific food supplements that prevent damage to the DNA produced by free radicals and contain vitamins and minerals necessary for proper sperm production and maturation.
These supplements must be taken for at least 3 months, which is the time it takes for sperm to be produced from scratch and mature.
FAQs from users
How can sperm morphology be improved?
Sperm morphology is one of the most important determinations and one of the critical parameters in determining a man's ability to fertilize. Sperm morphology evaluates the morphometric characteristics of the sperm head, midpiece and tail.
Normal spermatozoa have an oval head and a long tail. In contrast, abnormal sperm have defects in the head or tail, such as a large or misshapen head or a double or crooked tail.
There are not many known factors that can improve sperm morphology and thus increase the percentage of normal forms.
It has been seen that the time sperm spend stored in the epididymis can be a determining factor in seminal quality; low ejaculatory frequency has been related to increased exposure to the effects of oxidative stress.
The time of sexual abstinence is one of the clinical criteria taken into account during seminal analysis; the interval recommended by the WHO is 2 to 7 days. Some studies have shown that increased ejaculatory frequency has positive effects on different conventional semen parameters, including sperm morphology.
In Assisted Reproduction, when performing IVF, we can improve fertilization results in cases of alterations in sperm morphology with intracytoplasmic sperm injection (ICSI). This technique makes it possible to select the spermatozoa at the time of fertilization also based on morphological criteria.
Can an abnormal sperm fertilize? Is pregnancy possible?
Yes, abnormal sperm is able to fertilize but most likely will not since those with normal shape move faster and will have it easier to reach the egg.
Depending on how the sperm are altered and how many abnormal sperm there are, the likelihood of pregnancy will be higher or lower.
For example, in spermatozoa without head (no genetic content) or with a small or absent acrosome (necessary to penetrate the egg) fertilization will not take place since they lack an essential part for the process.
Can abnormal sperm cause a miscarriage?
That might happen. The altered sperm may have genetic abnormalities that make it difficult or impossible for the embryo to form or develop, so it may not be viable and may stop growing, causing a miscarriage.
Depending on the gene or genes affected, embryonic development would stop at one point or another, depending on when they have to start expressing themselves; in other words, if the gene that is defective is very important in the first few weeks of pregnancy, an early abortion would occur because it does not contain adequate information for its development.
Can there be abnormal sperm from varicocele?
Varicocele is the cause of approximately 40% of male infertility cases. It produces a decrease in sperm production capacity, mainly due to an increase in testicular temperature and free radicals.
Therefore, it decreases both the concentration and the mobility of the spermatozoa and it seems that it is also related to the appearance of anomalies in the sperm morphology such as alterations in the head.
Recommended readings
If you want more information about the seminogram, you can visit the following link: What is a basic seminogram and how is it done step by step?
If, on the other hand, you want to know more about antioxidants to improve semen quality, we recommend you read this article: What are antioxidants and how do they affect semen quality?
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
Auger J, Jouannet P, Eustache F. Another look at human sperm morphology. Hum Reprod. 2016 Jan;31(1):10-23.
Danis RB, Samplaski MK. Sperm Morphology: History, Challenges, and Impact on Natural and Assisted Fertility. Curr Urol Rep. 2019 Jun 15;20(8):43.
van den Hoven L, Hendriks JC, Verbeet JG, Westphal JR, Wetzels AM. Status of sperm morphology assessment: an evaluation of methodology and clinical value. Fertil Steril. 2015 Jan;103(1):53-8.
Kruger TF, Acosta AA, Simmons KF, Swanson RJ, Matta JF, Oehninger S. Reprint of: Predictive value of abnormal sperm morphology in in vitro fertilization. Fertil Steril. 2019 Oct;112(4 Suppl1):e61-e66.
World Health Organization (WHO) (2010). WHO laboratory manual for the Examination and processing of human semen. 5th ed. Geneva: WHO Press;2010.
FAQs from users: 'How can sperm morphology be improved?', 'What are the causes of altered sperm morphology?', 'Can an abnormal sperm fertilize? Is pregnancy possible?', 'Can abnormal sperm cause a miscarriage?' and 'Can there be abnormal sperm from varicocele?'.
Authors and contributors

More information about Cristina Algarra Goosman




I wanted to know if a sperm count/ml is necessary when the patient have a teratozoospermia of more than 30%.
Dear JOSHUA CHIWARA,
Yes, in order for sperm quality and your chances for a natural pregnancy, knowing your sperm concentration values is totally necessary.
I hope this helps,
Regards
I need your help asap, please.
A week ago my baby was born and died, Edwards syndrome trisomy 18, it is already the second baby I have and the 2 same cases with Edwards syndrome.
What test should I have, what method of fertilization should we perform?
Hi Avatar,
To avoid having another pregnancy and the embryo having this genetic alteration, you can resort to assisted reproduction.
There is a preimplantation genetic diagnosis (PGD) in which the genetic information of the embryos is analyzed to select the “healthy” one without chromosomal alterations and transfer it to the mother’s uterus. You can find out what PGD consists of at the following link: What is PGD?
In order to perform this technique, it is necessary to carry out an in vitro fertilization (IVF) treatment in a clinic. If you are interested and need help, I recommend you use this tool: Fertility Report. It is available to all our readers with the aim of helping them to find recommended clinics in their area that meet our rigorous quality criteria, a detailed explanation of how the treatment is to be carried out with an explanatory video, useful advice and more.
Hope I could help you,
wish you all the best.
Hello!
my wife and I have been trying to conceive for 10 months. Would like to know our chances of getting pregnant with a fertility treatment.
Here are my results:
Color: normal
Opacity: opaque
Viscosity: normal
Volume: 4.80 ml
Ph: 7.90
Numbers
Sperm / ml: 130.000.000
Round cells / ml: 450.000
Progressive motility: 50%
Non-progressive motility: 30%
Inmotile: 25%
Morphology:
Normal: 7%
Anormal: 93%
Hi Paolo,
Your results are normal, with a good count and mobility. The vitality parameter is missing, i.e. if there are dead sperm in the ejaculate. Possibly, if you haven’t had this result on the seminogram it’s because everything is fine.
Your wife should have a fertility test to see if she has any problems. However, to consider infertility, you must have at least 1 year of unprotected sex.
Hope I could answer your question,
all the best.