A semen analysis, also known as sperm test or spermogram, is a type of test to evaluate the quality of a sperm sample and the sperm count. In other words, it is an effective method for determining male fertility. Therefore, the semen analysis is the basic test in the study of male fertility, although it is usually accompanied by other additional tests.
Broadly speaking, after collecting the semen sample, the clinic analyzes the different sperm parameters in the lab. When the results are ready, a report with the results is provided to the patient. In order to understand them, it is important that you learn how to read them. Here are some key factors to keep in mind when it comes to interpreting a semen analysis.
Provided below is an index with the 6 points we are going to expand on in this article.
- 1.
- 1.1.
- 1.2.
- 2.
- 2.1.
- 3.
- 3.1.
- 3.2.
- 3.3.
- 3.4.
- 3.5.
- 3.6.
- 4.
- 5.
- 6.
Semen parameters
The WHO (World Health Organization) has published a series of guidelines as regards the sperm parameters that should be examined in a semen analysis, and has established the reference values to determine if the results are normal or not.
Although the World Health Organization (WHO) has published an update of the Laboratory Manual for Semen Examination and Processing in 2021 (the sixth edition), the most common practice is to continue to follow the criteria of the fifth edition (2010).
Sperm parameters can be examined macroscopically and microscopically. Continue reading in order to learn how to understand each type of analysis along with the reference values of each:
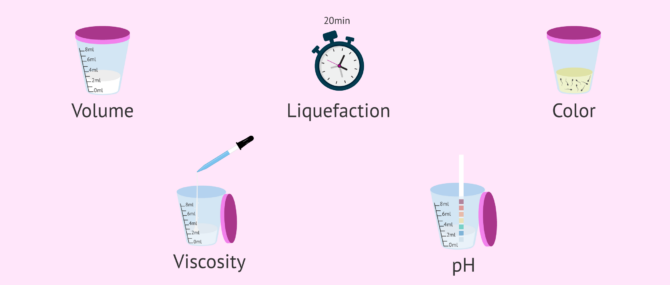
Macroscopic examination
A macroscopic examination allows the specialist to evaluate the basic characteristics of the sperm sample, that is, the ones that can be seen by the naked eye, without using a microscope. The following are key values:
- Volume
- Measured in milliliters (ml). Samples are considered normal if the volume is above 1.5 ml.
- Liquefaction
- The sample needs to be liquefied for 20 minutes prior to doing the analysis until it becomes totally liquid.
- Color
- The normal color of the semen is yellowish to greyish. If the sample is too transparent, it may indicate the presence of white blood cells (leukocytospermia). If it is too opaque, it is likely that the sperm count is high.
- Viscosity
- The specialist measures the length of the threads formed by drops. Threads must break so that the sample can be examined accurately. A sample that is too viscose can indicate prostate problems.
- pH
- The normal pH of semen ranges between 7 and 8. Variations under or above this range are associated with infections.
Taking these aspects into account, it is not complicated to be able to interpret the semen analysis by oneself and get an approximate idea of whether the semen sample presents any alteration.
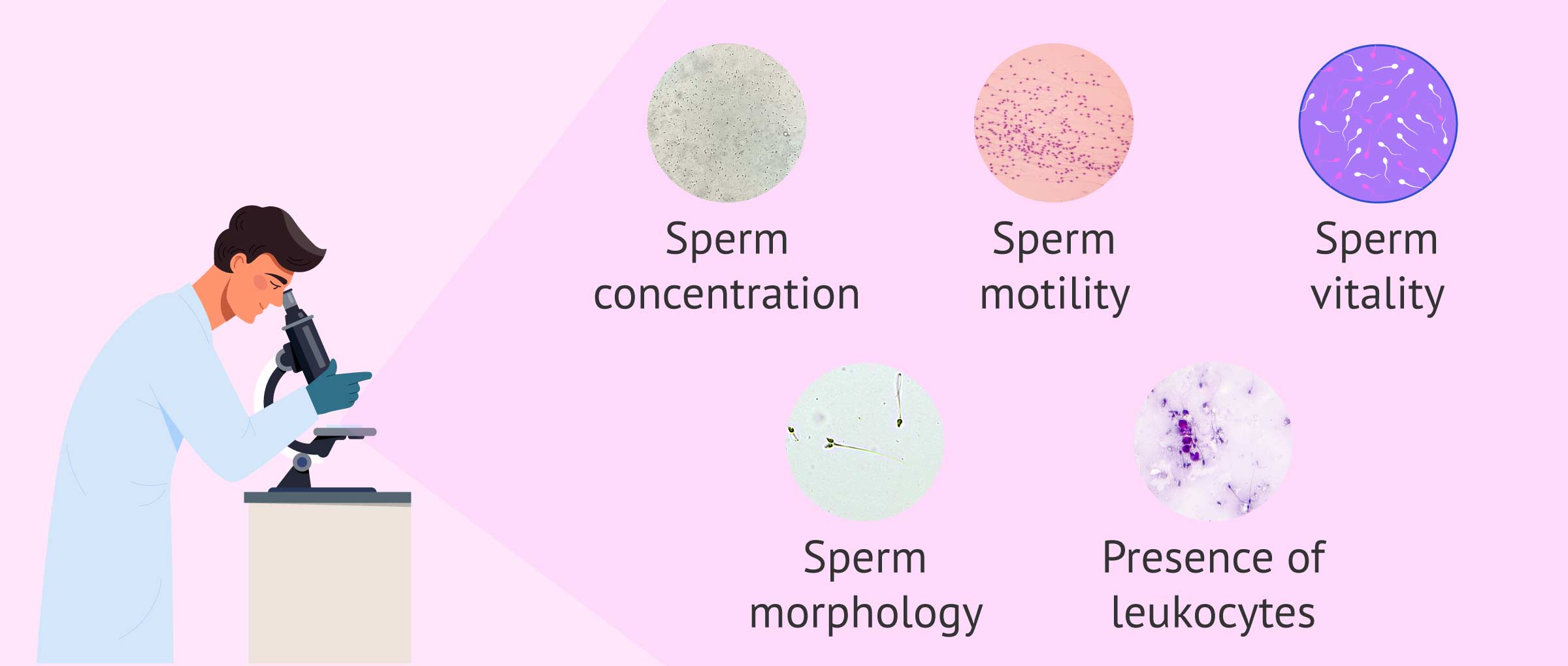
Microscopic examination
If a macroscopic examination is more associated with the external traits of the semen and the fluids it is composed of, a microscopic examination focuses on all aspects related to the sperm cells.
To this end, a drop of semen is put in a Makler counting chamber to analyze the following sperm parameters under the microscope:
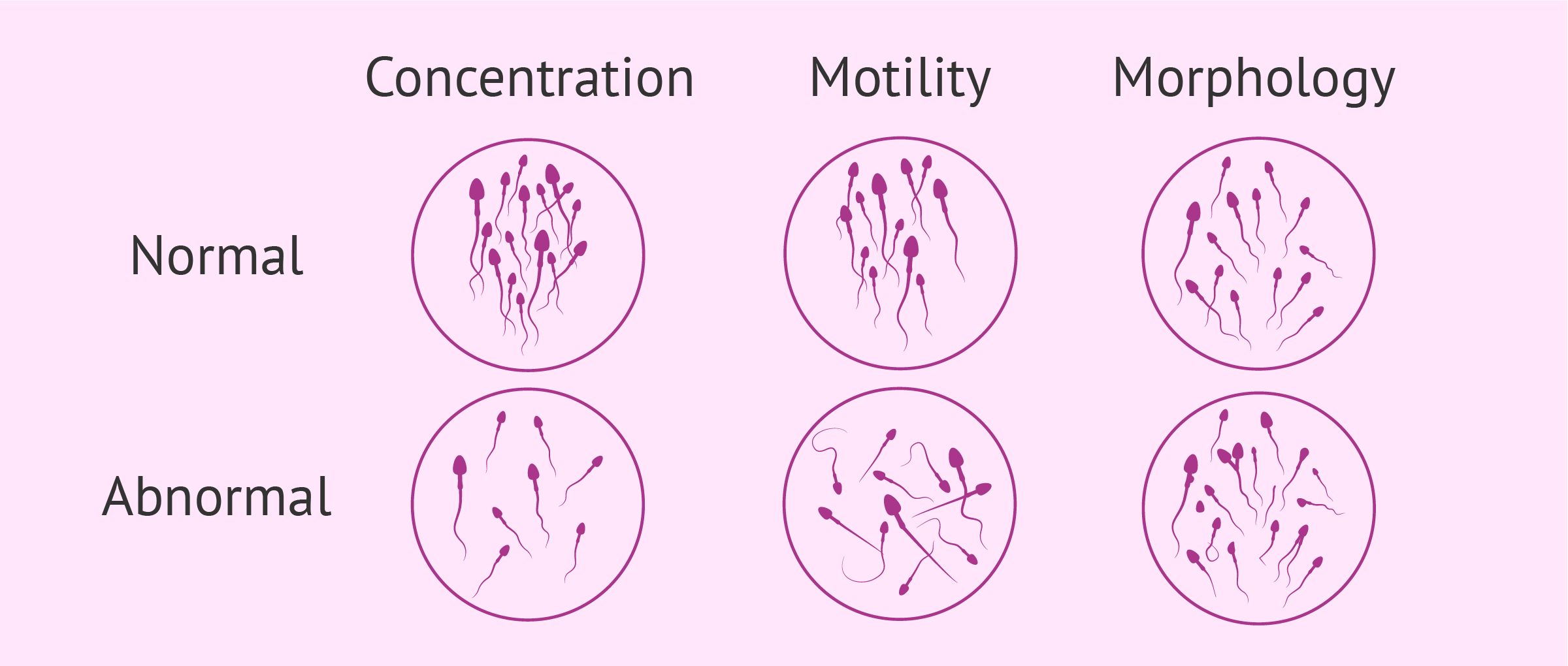
- Sperm count
- The total sperm count must be higher than 15 million sperm per milliliter or 39 million per ejaculate in order to be considered normal.
- Sperm motility
- It is used to examine the percent of motile sperms in the sample, as well as the ones that are able to "swim" in terms of rapidly progressive, slowly progressive, or non progressive. A sperm sample is considered normal when more than 40% of sperm are able to move and over 32% are able to make forward progress.
- Sperm vitality
- There exist many tests to determine whether there are dead sperm cells in the ejaculate: eosin Y dye test, hypo-osmotic swelling test, etc. For a semen sample to be considered normal, the percentage of live sperm should be above 58%.
- Sperm morphology
- Hematoxylin and Eosin stain is used to evaluate the morphology of a drop of semen. The sperms are examined one by one to detect the presence of anomalies. Normal forms must be present in at least 4% to consider that the sample is normal.
- Presence of WBCs
- In case white blood cells (WBCs) are present in the sample, the amount is examined under the microscope. If the presence of WBCs or leukocytes is above 1 million/ml, it is an indicator of infections. This condition is known as leukocytospermia or pyospermia.
You may also enjoy some further information reading this: What Is a Semen Analysis Report? – Purpose, Preparation & Cost.
How to read a sperm analysis report
Once you have the results of the semen analysis, you should consider the following aspects concerning the format in order to understand your report accurately:
- The WHO's reference values are normally included in brackets next to your result.
- The sperm count is provided in millions per milliliter (ml).
- Sperm motility, morphology, and vitality are provided in percentages.
- The unit measures or reference values used might differ from lab to lab, should you repeat the semen analysis at a different clinic.
- The WHO's reference values used today are the ones they published back in 2010.
If the results of your spermogram reach the lower reference values of semen variables established by the WHO, your semen analysis report is considered normal. In other words, you don't have any fertility issues. This is known as normozoospermia.
Possible alterations in seminogram results
In case any of these parameters fall outside these ranges, the sample will be considered abnormal. These are the different types of sperm disorders that may be diagnosed:
- Azoospermia
- Zero sperm count
- Oligospermia
- Low sperm count
- Asthenozoospermia
- Poor sperm motility
- Teratozoospermia
- Abnormal sperm morphology
- Necrospermia
- High number of dead sperm
- Hypospermia
- Low sperm volume
It is also possible to have a combination of two or more of these pathologies, such as oligoasthenoteratospermia. The prognosis in these cases will be worse.
Assisted procreation, as any other medical treatment, requires that you rely on the professionalism of the doctors and staff of the clinic you choose. Obviously, each clinic is different. Get now your Fertility Report, which will select several clinics for you out of the pool of clinics that meet our strict quality criteria. Moreover, it will offer you a comparison between the fees and conditions each clinic offers in order for you to make a well informed choice.
In any case, the chances of getting pregnant will depend on the parameter that is affected and the grade of severity.
FAQs from users
What else is evaluated during the semen analysis besides the number and motility of spermatozoa?
The semen analysis is a key study in the evaluation of a couple's infertility and is fundamental for defining the treatment that can help in achieving pregnancy.
The basic semen analysis (seminogram or spermogram) not only evaluates the number and motility of the spermatozoa but should also study the volume, color, liquefaction, viscosity, and pH of the seminal fluid, the presence of leukocytes in the ejaculate, or the morphology of the spermatozoa.
It should be understood that the seminal sample in an ejaculate not only contains cells from the testes but also fluid from the seminal vesicles and prostate and that alterations at these two levels can produce alterations in the physical and chemical characteristics of the sample.
One of the important aspects to evaluate in the basic semen analysis is the sperm morphology, that is, the appearance of the spermatozoa and, as a percentage, the number of cells that are abnormal. If this percentage is higher than 96%, which implies that there are less than 4% of normal cells, in the case of infertility, the recommended treatment is in vitro fertilization with sperm microinjection.
What happens if my sperm sample is rejected?
Sperm specimens that are rejected for any reason should be repeated three days after last ejaculation in order to respect the abstinence period.
Can having your phone in your pocket make you infertile?
Some scientific studies have suggested that the radio frequencies used by cell phones could have harmful effects on health, such as a decrease in sperm quantity and quality.
However, not all studies present the same results. This may be due to the presence of confounding factors, as for example has happened in the case of coffee, which has been associated in some studies with lung cancer.
The conclusion is that at present we cannot be certain that the use of cell phones affects sperm quality. However, there are studies that suggest it and it seems reasonable to recommend that patients who have sperm problems or who are going to undergo fertility treatment should, as far as possible, not abuse the use of these devices.
The results of my semen analysis are abnormal, what's next?
Your doctor will evaluate the results of the semen analysis along with other tests such as hormonal testing, anatomical evaluation, related conditions, genetic factors, medical history, etc.
Only by doing this, he or she will be able to identify the cause behind abnormal results and find the best possible solution or treatment. In case the results don't improve after repeating the semen analysis, it is likely that a fertility treatment is needed.
What causes round cells in sperm?
Sometimes, a macroscopic examination of a sperm specimen shows a high percentage of round cells in addition to sperms. Normally, they are just bladder, prostate or urethral epithelial cells, immature germ cells, or white blood cells (leukocytes).
The presence of leukocytes indicates the presence of an infection, which could lead to alterations in other parameters. In this case, the semen analysis would be repeated after treating the infection with antibiotics.
What may be the cause of incomplete seminal liquefaction?
Incomplete liquefaction of semen may be caused by a lack of prostate enzymes. Liquefaction is the process by which semen becomes less viscous, i.e., it becomes more liquid in appearance. Liquefaction usually occurs after about 15-20 minutes.
An altered value of seminal liquefaction can affect the motility and concentration of spermatozoa, providing altered semen analysis results. Therefore, this alteration can cause problems in achieving pregnancy naturally.
Suggested for you
This post focuses on the interpretation of a semen analysis report. To learn how to prepare, how long you should abstain before a sperm analysis and more, read: What Is a Semen Analysis Report? – Purpose, Preparation & Cost.
Also, we have made several references to a condition called leukocytospermia or pyospermia, which is diagnosed when the presence of white blood cells is detected in a sperm sample. See this for more: Leukocytospermia or Pyospermia – Symptoms, Causes & Treatment.
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
Andrade-Rocha FT (2003). Semen analysis in laboratory practice: an overview of routine test. J Clin Lab Anal 2003; 17: 247-258 (View)
Baker DJ (2007). Semen analysis. Clin Lab Sci; 20: 172-187; quiz 188-192 (View)
Kruger TF, Menkveld R, Stander FS, Lombard CJ, Van der Merwe JP, van Zyl JA, et al. Sperm morphologic features as a prognostic factor in 'in vitro' fertilization. Fertil Steril; 46: 1118-1123 (View)
Kvist U, Björndahl L. ESHRE Monographs: Manual on Basic Semen Analysis. Oxford: Oxford University Press, 2002 (View)
Rogers BJ, Bentwood BJ, Van Campen H, Helmbrecht G, Soderdahl D, Hale RW (1983). Sperm morphology assessment as an indicator of human fertilizing capacity. J Androl; 4: 119-125 (View)
Sociedad Española de Fertilidad (SEF) (2011). Manual de Andrología. Coordinador: Mario Brassesco. EdikaMed, S.L. ISBN: 978-84-7877.
Sigman M, Zini A. (2009). Semen analysis and sperm function assays: what do they mean? Semin Reprod Med; 27: 115-123 (View)
World Health Organization (WHO) (1992). Laboratory manual for the examination of human semen and sperm-cervical mucus interaction. 3rd ed. Cambridge, UK; Cambridge University Press (View)
FAQs from users: 'What else is evaluated during the semen analysis besides the number and motility of spermatozoa?', 'What happens if my sperm sample is rejected?', 'Can having your phone in your pocket make you infertile?', 'The results of my semen analysis are abnormal, what's next?', 'What causes round cells in sperm?' and 'What may be the cause of incomplete seminal liquefaction?'.