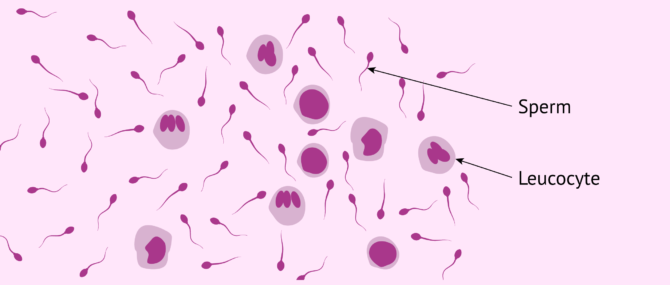
Leukocytes or white blood cells (WBCs) are present in the semen by default, though in a reduced number.
If an elevated number of WBCs appears after a semen analysis (SA), we may suspect that there exists an infection. The presence of a high number of leukocytes in the semen is an abnormality known as leukospermia or pyospermia.
Provided below is an index with the 10 points we are going to expand on in this article.
- 1.
- 1.1.
- 2.
- 3.
- 4.
- 5.
- 6.
- 7.
- 7.1.
- 7.2.
- 7.3.
- 7.4.
- 7.5.
- 7.6.
- 7.7.
- 8.
- 9.
- 10.
Definition
Leukospermia, leukocytospermia, or pyospermia is defined as the presence of more than 1 million leukocytes in 1 ml semen. As stated earlier, having Leukospermia means that there is an abnormal increased amount of leukocytes in the ejaculate.
Leukocytes, leucocytes, or white blood cells (WBCs) are cells produced by the immune system that can be found in the blood. Their main function is to help your body fight infections.
While it is normal to detect a few WBCs in the semen after performing a sperm analysis, an elevated concentration of leukocytes in a sample can compromise male fertility, as it increases the levels of oxidative stress and decreases sperm quality. In short, in can reduce a man's sperm concentration.
The presence of leukocytes in the semen can cause temporary sterility, but rarely permanent sterility or infertility. For this reason, when leukospermia is detected, the patient needs a specific treatment to solve the infertility issues it might be causing and avoid that it becomes permanent.
How are pyocytes counted in semen?
Specialists calculate the amount of leukocytes in the semen per milliliter of semen following the criteria of the World Health Organization (WHO), which reference value is set at 1 million leukocytes per ml of semen. If a sample surpasses this figure, the patient will be diagnosed with pyospermia or leukospermia.
The picture above shows how a semen sample with leukocytospermia would look under the microscope. Leukocytes differ from spermatozoa because they are round-shaped structures and larger in size.
Symptoms and effects
Normally, leukospermia is asymptomatic and can only detected via a sperm analysis, often when the patient is getting started with a fertility treatment or applies to become a sperm donor.
However, sometimes the patient has certain signs and symptoms that may indicate the presence of pyospermia, including:
- Semen appears yellow in color
- Swelling in the area of the penis or groin
- Genital infections: herpes, chlamydia, gonorrhea...
- Widened or dilated veins coming from the testes
- Infrequent ejaculation
- Reduced fertility
Inflammations often cause the formation of a large amount of active-oxygen radicals, which can have negative effects on sperm, including the disruption of the integrity of their membranes, and the inhibition of sperm motility.
Causes of leukospermia
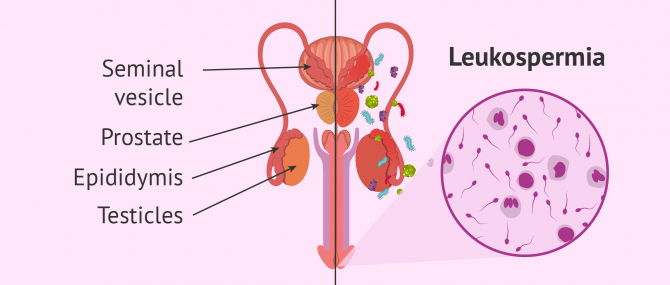
The main causes of leukospermia are infections or inflammations of the urethra, and prostatitis or inflammation of the prostate gland.
More often than not, this kind of infections come with no symptoms and are detected after performing a semen analysis, when a man is about to start an infertility treatment or being screened to become a sperm donor.
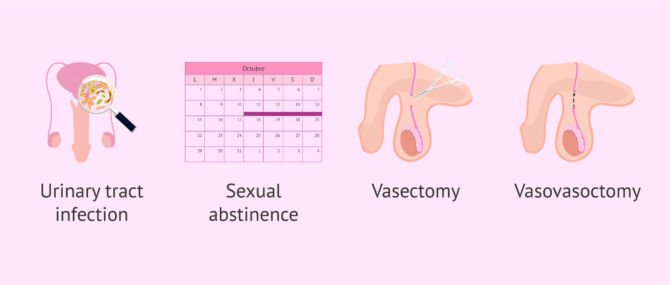
There exist other causes that can lead to an increased level of leukocytes in the semen. Various studies have revealed that sexual abstinence can have an influence, as the more time sperms remain in the epididymis, the greater the amount of macrophages and granulocytes that will be attracted by older sperm, which can cause an elevated level of leukocytes in the ejaculate.
As for men with a vasectomy, there is proof that men who have undergone this surgical intervention have a lower amount of leukocytes in their semen if compared to men who have not had a vasectomy done.
On the other hand, men who have undergone a vasovasostomy or vasectomy reversal tend to present altered sperm parameters in the results of their semen analysis, as well as sperm dysfunction, mainly caused by high levels of Reactive Oxygen Species (ROS). There is direct link between an increase in the ROS levels and the presence of WBCs in the semen. This is not an absolute association, though.
Genital tract infection
Genital tract infections represent about 4 to 10% of the cases of male sterility. Inflammation causes leukocytes to infiltrate in the seminal fluid, which diminishes sperm motility, triggers acrosome reaction, and reduces the fertilization potential of sperms. All this makes it more difficult for the couple to achieve pregnancy.
Approximately 50% of leukocytes that infiltrate in the seminal fluid come from the prostate and the seminal vesicles where the man suffers from prostatitis (prostate infection) or seminal vesiculitis (seminal vesicle infection). Thus, infections in the accessory glands lead to an increased number of leukocytes in the ejaculate.
The following is a list of the most common microorganisms that can cause it:
- Escherichia coli or E. coli
- Klebsiella pneumonia
- Ureaplasma urealyticum
- Proteus mirabilis
- Pseudomona aeruginosa
- Staphilococcus aureus
- Mycoplasma hominis
- Enterococcus faecalis
- Morganella morganii
- Chlamydia trachomatis, and other sexually transmitted diseases (STDs).
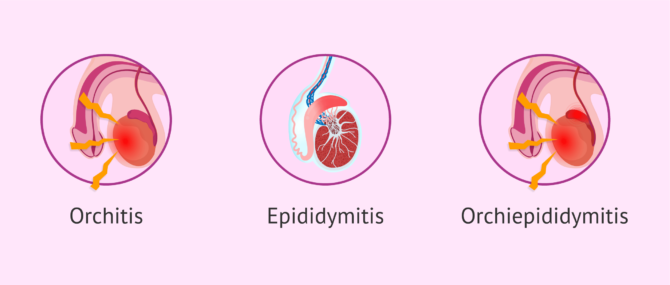
Bacteria and other germs can nest in any organ of the seminal tract, thereby causing the gonads, seminal ducts, and accessory glands to become swollen. Depending on the location of the infection, it will lead to:
- Orchitis
- infection of the testicles.
- Epididymitis
- infection of the epididymis.
- Orchiepididymitis
- infections of both the testicles and the epididymis.
For more information about seminal infections, please read the following article: Sperm Infections and Temporary Infertility.
Semen culture
When the amount of leukocytes in the semen is above 1 million/ml after a semen analysis, a bacteriological workup that involves semen culture is required.
Samples are incubated at the adequate temperature in each culture medium. Then, the specialist evaluates the results of the semen culture, that is, whether any of the microorganisms analyzed is present.
If the result is positive, the next step is to examine the plate, and count the number of colonies. One should note that the color of a colony is an indicator of the microorganisms that form it.
Additionally, sperm staining techniques and subsequent observation under the microscope can also help the specialist to determine what is causing the infection.
The result of the semen culture should be null, as bacteria, yeast, or any other microorganism that causes infections should not be present.
Undergoing a semen culture is also recommended in men who experience any of the symptoms listed above, including pain and inflammation of the testicles, blood in the sperm (hematospermia), or changes in the color and/or odor of the ejaculate.
The presence of blood in the seminal fluid can be caused by the rupture of a small blood vessel at some point throughout the pathway of sperm, generally as a consequence of an urinary infection or trauma.
Treatment of leukospermia
If some sort of microorganism is detected, the specialist will prescribe a treatment to erradicate the infection. Normally, the medicine of choice are antibiotics.
The type of antibiotics used and the duration of the treatment depend on the pathogen identified through the semen culture as the cause of the infection.
Aside from antibiotics, sometimes doctors prescribe painkillers or antioxidants that help diminish the levels of oxidative stress caused by the infection. This is also the treatment of choice when discovering the pathogen behind the infection has not been possible (i.e. abacterial leukocytospermia).
After the treatment, the patient should undergo another spermatobioscopy to count the number of leukocytes again. If antibiotics have worked, the amount of leukocytes in the semen would be lower. In general, if the infection is cured, all other sperm parameters improve as well, thereby boosting sperm quality.
If you need to undergo IVF to become a mother, we recommend that you generate your Fertility Report now. In 3 simple steps, it will show you a list of clinics that fit your preferences and meet our strict quality criteria. Moreover, you will receive a report via email with useful tips to visit a fertility clinic for the first time.
FAQs from users
Is IVF possible in cases of leukocytospermia?
Leukocytes or pyrocytes are generally scarce in the seminal fluid or even absent. However, if there is a large number of these cells, it could be an indication that there is an infection. This high presence of leukocytes is known as leukospermia, leukocytospermia or pyospermia.
It is common to observe some of them in semen samples when seminograms are performed. However, when they are in an abnormally high concentration (over 1 million leukocytes per ml according to WHO definition), it can compromise male fertility because it increases oxidative stress and causes a worsening of seminal quality, as it can affect sperm concentration. The presence of leukocytes in sperm can cause temporary sterility.
For this reason, in cases where leukospermia is detected, specific treatment is needed to resolve this sterility and prevent it from having a negative impact on the result of in vitro fertilization or becoming permanent.
Is there a cure for leukocytospermia?
Yes. In most cases, it is possible to erradicate it by means of antibiotics. The type of antibiotics to administer is dependent on the pathogen causing the infection.
When there is no infection, and the only symptom is an inflammation, painkillers may be enough.
Can leukocytospermia cause male infertility?
Leukocytospermia is a cause of male factor infertility, but in principle there is no reason why it should lead to long-term male sterility. As explained above, in most cases, it can be treated with antibiotics and normally patients are able to recover or even improve their sperm parameters.
Is there a link between leukocytospermia and teratospermia?
Yes. Several studies have found a link between leukospermia and greater chances of suffering teratospermia, that is, having an elevated number of morphologically abnormal sperm in the ejaculate.
However, this association is not clear enough yet, as it does not apply in all cases—the amount of sperms with abnormal forms does not always increase, or not so severely as to diagnose the patient with teratozoospermia.
Also, pyospermia has been related to low sperm concentration (oligospermia) as well as alterations in sperm motility (asthenospermia).
How is leucospermia diagnosed?
Leukospermia is the presence of a high number of white blood cells in a semen sample. According to the World Health Organisation (WHO) in 2010, there must be more than 1 million leukocytes per millilitre of semen for a diagnosis of leukospermia to be made. For this, a semen analysis should be carried out in a specialised centre.
The presence of leukocytes in the sample is indicative of an infection or inflammation of the urinary tract or seminal tract and can lead to a decrease in the quality of the semen sample because the leukocytes expel reactive oxygen species in an attempt to eliminate the pathogens that are causing the infection.
To diagnose what type of pathogen is causing the infection, a semen sample and a urine sample from the patient should be sent to the microbiology laboratory for analysis, where a culture of both will be performed. In this way it can be determined which microorganism it is and which antibiotic is indicated to fight the infection.

Once the micro-organism has been identified, the patient will be prescribed the indicated antibiotic. Some time after completing the treatment, the semen analysis can be repeated to assess whether the number of leukocytes in the sample has decreased. Therefore, leukospermia is a reversible alteration that does not necessarily cause permanent sterility.
If I have leukocytospermia, what treatment do I have to follow?
The first step would be to identify the origin of the leucospermia. If it is infectious, which is demonstrated by a semen or urine culture and antibiogram, antibiotic treatment will be necessary, and if it is of inflammatory origin, it will be treated with anti-inflammatory drugs.
Does leukospermia affect the chances of pregnancy?
Yes, leukospermia is an increase in the number of leukocytes, also known as white blood cells or pyocytes, in the semen. If there is an abnormal number of white blood cells in the semen, it may cause sperm agglutination and, as a consequence, sperm motility will be reduced.
Another effect of a large number of leucocytes in semen is that it increases oxidative stress and may reduce sperm concentration.

As a result, leukospermia may hinder the chances of pregnancy. In these cases, it will be necessary to treat the seminal condition before trying to achieve pregnancy.
Suggested for you
As you have just read, leukospermia can be detected by means of a semen analysis or seminogram. If you want to learn more about this diagnostic test, visit this post: What is a semen analysis and what does it involve?
Moreover, if you want to delve deeper into the causes of this pathology, we recommend you to have a look at this article: Infections and temporary sterility.
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
David M Rodin, Davise Larone, Marc Goldstein. Relationship between semen cultures, leukospermia, and semen analysis in men undergoing fertility evaluation. Fertil Steril. 2003 Jun;79 Suppl 3:1555-8. doi: 10.1016/s0015-0282(03)00340-6 (View)
J S Armstrong, M Rajasekaran, W J Hellstrom, S C Sikka. Antioxidant potential of human serum albumin: role in the recovery of high quality human spermatozoa for assisted reproductive technology. J Androl. 1998 Jul-Aug;19(4):412-9 (View)
K Shimoya, N Matsuzaki, T Tsutsui, T Taniguchi, F Saji, O Tanizawa. Detection of interleukin-8 (IL-8) in seminal plasma and elevated IL-8 in seminal plasma of infertile patients with leukospermia. Fertil Steril. 1993 Apr;59(4):885-8 (View)
S Long, S Kenworthy. Round Cells in Diagnostic Semen Analysis: A Guide for Laboratories and Clinicians. Br J Biomed Sci. 2022 Feb 2;79:10129. doi: 10.3389/bjbs.2021.10129. eCollection 2022 (View)
Ye Yao, Xin-Jian Qiu, Dong-Sheng Wang, Jie-Kun Luo, Tao Tang, Yun-Hui Li, Chun-Hu Zhang, Hao Liu, Lu Zhou, Lin-Lin Zhao. Semen microbiota in normal and leukocytospermic males. Asian J Androl. 2022 Jul-Aug;24(4):398-405. doi: 10.4103/aja202172 (View)
FAQs from users: 'Is IVF possible in cases of leukocytospermia?', 'Is there a cure for leukocytospermia?', 'Can leukocytospermia cause male infertility?', 'Is there a link between leukocytospermia and teratospermia?', 'How is leucospermia diagnosed?', 'If I have leukocytospermia, what treatment do I have to follow?' and 'Does leukospermia affect the chances of pregnancy?'.
Authors and contributors








Volume 3.5 mL
Color Grey
PH 8.0
Liquefaction Time 30 Min
Motility (%) 65-70
Progress Motility 3+
Spermatozoa Count 200 x10^6/L
Spermatozoa vitality (%) 80
Morphology-Abnormal 25
RBC /hpf 6-8
WBC /hpf 15-20
Crystals are Nil
Clumping is 3+
Normal functional Sperm x10^6/L is 365
Hello Ehsan,
Volume is ok. As regards motility, it is kind of difficult for me to provide an answer, as I don’t know which type of motility is being measured here. However, it seems to be fine in principle. Concentration and vitality are ok, too.
Given that your WBC are above 2-5, it indicates the presence of an infection on your semen. Red blood cells are also above the normal values, which indicates the presence of some blood traces on your sample as well. Sperm agglutination is also present.
If the infection is confirmed by your doctor, you’d be prescribed antibiotics and advised to repeat the semen analysis.
Hope this helps,
Regards
My semen report says I have leukocytes 10 to 12/HPF (High Power Field) noted and absence of spermatozoa… Pls help, what treatment to take and which doctor to consult.
Dear prashun,
First of all, the doctor you should consult is an andrologist ideally. Secondly, I’m afraid in principle there is no treatment to take or follow. With azoospermia, patients should go for a second semen analysis to confirm the diagnosis. If so, the next step would be to find what is causing it by means of a testicular biopsy if you want to find out whether you’ll be able to conceive in the future. If nothing is found through a biopsy, I’m afraid it is a case of secretory azoospermia, and there’s nothing to be done. Conversely, if sperm are found, it is obstructive azoospermia and you might still have chances with ICSI.
I hope this helps,
Best
I did a sperm analysis and the results were as follows:
Volume – about 1 ml
Viscosity- Normal viscous
Motility- about 50 % progressive forward – about 15 % sluggish movement – about 35 % dead
Count – < 20 millions/ umm
Leucocytes – 30 – 50 hpf
Please can you help to analyse the information and give me some prescriptions?
Hello, the result of my semen analysis reads:
Appearance: greyish-white & non viscous fluids
volume: 2.5ml
motility: 2% sluggishly motile
cell count: 900,000 cells/ml
morphology: few normal cells seen
leukocytes: numerous
culture: yielded scanty growth of staphylococcus Aureus
please kindly help me to explain the result, can I father children under such conditions? if there’s any problem kindly mention it with possible solutions.
I need your urgent reply. Thanks
Dear Tony,
Your semen analysis shows several seminal alterations that affect your possibilities of conceiving naturally. Motility, concentration and morphology are strongly altered with values way lower than the ones that are considered normal and that allow natural pregnancy. The recommendation is to consult an assisted reproduction specialist in order to determine which would be the best treatment and technique in your case.
On the other hand, on the culture has been detected an infection that may need antibiotic treatment. The appropriate antibiotic will be prescribed by your doctor.
I hope I have been able to help.
Best regards,
Can anybody help? My doctor is now on leave and the private clinic want another £100 to tell me what these results actually mean!
Volume ml – 2.40
pH – 7.50
Appearance – Clear
Viscosity – Normal
Liquefaction – Complete
Density x106 /ml – 44.00
Total count x106 – 105.60
Motility %
Progressive – 72.0
Non progressive – 1.0
Immotile – 17.0
Normal forms % – 4.00
Other Parameters
Agglutination – Nil
Aggregation – Nil
Round Cells (x106 /ml) – >5.0×10/6/ml
Conclusions:
Normozoospermia. All parameters above the lower reference limits, therefore this sample is suitable for any form of treatment.
High density round cells
Increased round cells please discuss with the clinicians. Please call the contact centre on —– to book a follow-up appointment with the clinical team.
Dear Sophie,
As the conclusions of this analysis indicate, your partner is normozoospermic, which means his semen results are within the normal results and in principle there should be no problem to achieve a pregnancy naturally.
What if wbc count is 2.50? If this is a real concern??
Total volume: 3 ml
Sperm concentration: 28 mill per ml
Active: 20
Mod active: 20
Sluggish:30
Dead:30
Normal morphology:80%
Abnormal morphology:20%
Wbc:2.50
Rbc: 0.4
Madam please give your feedback! Thanks
Dear Kally,
What unit of measure have they used for measuring WBC in this semen analysis? And what are the reference values used? I can’t give you an answer without that.
I need help please, I would like to know if the results are normal.
COLOR. White grey
PH: 8.0
VOLUME:6.0ml
LIQUEFACTION: 15min.
LEUCOCYTES: 0.2-0.3 /ml
SPERM COUNT: 70 000 000/ML
NORMAL: 70%
ABNORMAL:30%
0 HOURS
MOTILITY:65%
VITALITY:70%
1 HOUR
MOTILITY: 60%
VITALITY : 65%
2 HOURS
MOTILITY:55%
VITALITY:60%
Dear Roxy,
All the parameters seem to be within the normal range. Anyway, the doctor that requested the analysis should take a look in order to check that everything is alright taking into account the reference values used by the lab.
I hope I have been able to help.
Volume 4.5 ml
pH 7.6
Sperm Concentration 13 million ml
Progressive Motility 54%
Total Motility 54%
Total Sperm Concentration 58.5 million
Round Cell > 1 million
WBC > 1 Million
Normal Spermatozoa 4%
Spermatozoa with head defects 89%
Spermatozoa with Midpiece defects 6%
Spermatozoa with Tail Defects 1%
Once we clear up the WBC, does it seem like we’ll have good odds of getting pregnant? Seeing urologist Wednesday but anxious for answers.
Hello Beth,
After evaluating this semen analysis, I see that this is a case of mild oligospermia. However, as the volume is right, the total amount of sperms is right. As for WBC, yes, once the infection is cured, it is likely that the sperm concentration improves, so you can have chances of getting pregnant.
I hope this helps,
Best