Seminal infections are those invasions of pathogenic microorganisms that occur at some point in the male reproductive and urinary tract, so they may be present in the seminal fluid.
In the path that the spermatozoa and seminal fluid must follow to go outside, contact with the infected area will occur, which may alter the ability of the spermatozoa to fertilize the egg. Also, inflammation due to infection can cause an obstruction and impede the exit of sperm or ejaculate.
For all these reasons, infections in the male reproductive tract can cause fertility problems in the male and, therefore, difficulty in achieving pregnancy.
Provided below is an index with the 8 points we are going to expand on in this article.
- 1.
- 1.1.
- 1.2.
- 1.3.
- 2.
- 2.1.
- 2.2.
- 2.3.
- 2.4.
- 3.
- 4.
- 5.
- 5.1.
- 5.2.
- 5.3.
- 5.4.
- 5.5.
- 6.
- 7.
- 8.
How do I know if I have a seminal infection?
Usually, seminal infections do not cause symptoms, so it is possible for them to remain undetected in the male for a long period of time. Precisely because of this, i.e., because seminal infections are not treated as soon as possible, they can lead to male infertility.
Since in most cases the man is unaware that he has an infection, it is very common that it is detected after a medical consultation for infertility of the couple.
Even so, a man may still notice some discomfort if he has a seminal infection such as those listed below:
- Changes in semen, such as odor and color.
- Irritation and itching.
- Burning when urinating.
- Fluid discharge from the urethra.
- Blood in seminal fluid.
- Genital or inguinal pain, whether of the prostate, testicles, etc.
If any of these symptoms are present, it is important to avoid sexual intercourse and consult a physician immediately to request a semen and urine analysis.
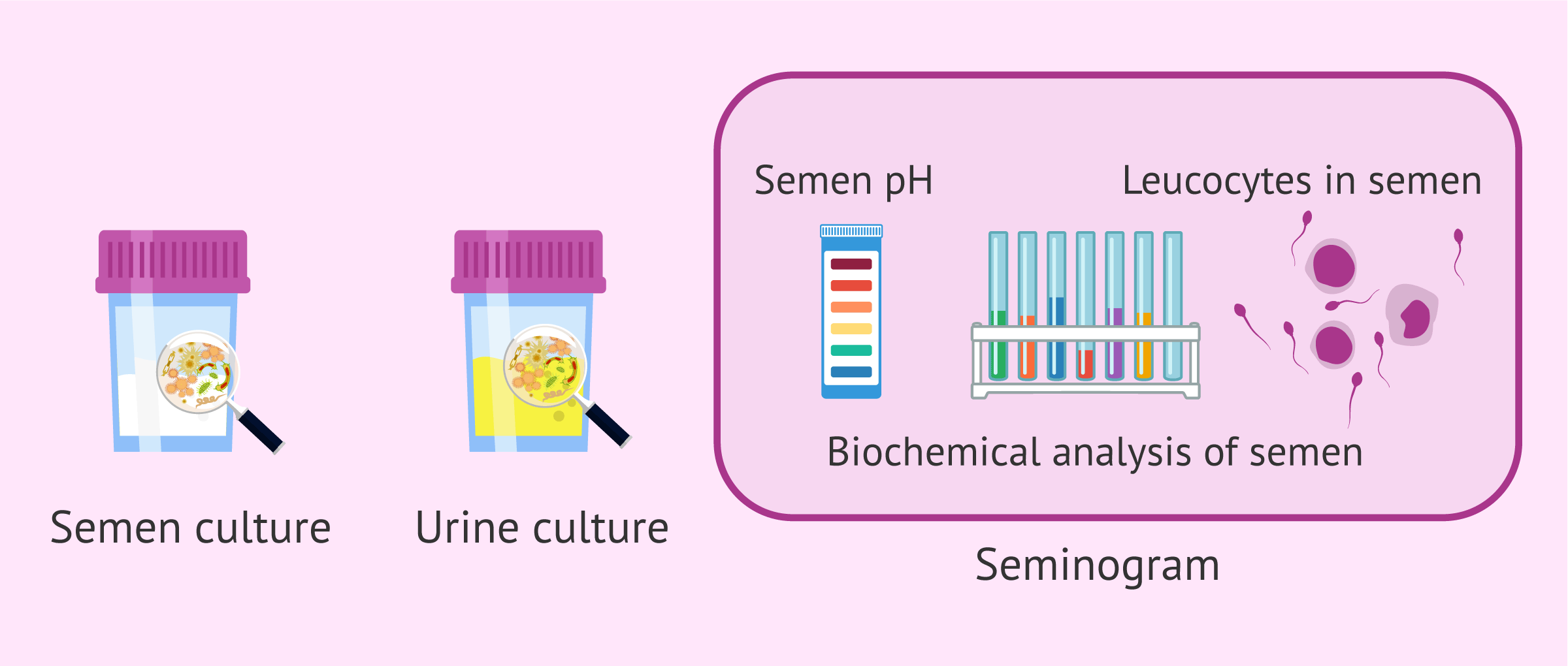
Semen analysis
The basic test in the study of male fertility is the seminogram, also called spermogram. This is an analysis of the ejaculate to see the state of the semen, analyzing both the seminal fluid and the spermatozoa it contains.
If a high number of leukocytes, an acid pH or altered semen biochemistry values are observed in the semen analysis, it could be due to a seminal infection. Therefore, a urine and semen culture should be requested to confirm this.
The first evaluation made in the seminogram is a macroscopic study of the seminal fluid. In this part, the study of the pH can already indicate the possibility of infection if it is acidic. The pH of the semen should be above 7.2. Otherwise, sperm motility and fertility may be impaired.
If you want to know what macroscopic and microscopic analyses are performed in a semen analysis, click on this link: What is a semen analysis and how is it done step by step?
Seminal fluid analysis
Next, the semen content is studied. For this purpose, a biochemical study is performed (usually a complementary test in the semen analysis) to detect the nutritional molecules present in the semen. In addition, a microscopic analysis is performed to analyze the spermatozoa and the presence of other cells.
One of the components of seminal fluid is the secretions of the accessory glands of the male reproductive tract. Thanks to this biochemical study of semen, it is possible to analyze these secretions and diagnose any abnormalities, either in the seminal glands (prostate and seminal vesicles) and/or in the epididymis.
Likewise, if the microscopic examination shows a high number of pyocytes or leukocytes, i.e., more than 1 million per milliliter, there is leukocytosis, which indicates the presence of an infection and a culture would be necessary.
Urine and semen culture
Semen culture or sperm culture allows the detection of microorganisms in semen. Under normal conditions, the semen should not have any bacteria or fungi. If the result of the semen culture indicates the presence of any microorganism, it means that there is an infection.
Normally, it is recommended that the male maintain a period of abstinence for 3 to 5 days before a semen culture is performed. Otherwise, the result of the seminal culture could be erroneous.
One of the requirements for a semen culture is that the male obtains the sperm sample by masturbation. In addition, it is important that the semen is analyzed within one hour of collection.
On the other hand, urine culture, urine culture or urine culture detects infectious microorganisms in urine, mainly bacteria and fungi. In normal situations, urine contains microorganisms, but if these are in high quantities they can cause a urinary tract infection.
what type of seminal infection can it be?
Infections can affect different parts of the male genital tract, both in the reproductive and urinary tracts. There are infections in the urethra, prostate, ejaculatory duct, seminal vesicles, vas deferens, epididymis and testicles.
If the infection affects the spermatic ducts, they may become inflamed and cause an obstruction. Depending on the point at which the inflammation occurs, the outflow of ejaculate and/or sperm may be impeded. For this reason, seminal infections could be the reason for male infertility.
Some of the seminal infections are discussed below.
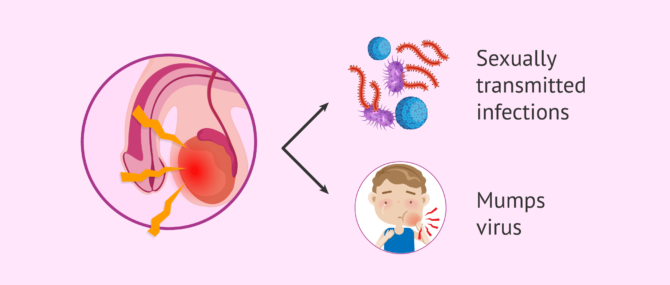
Orchitis
Orchitis is the inflammation of one or both testicles, usually due to testicular or epididymal infection (orchitis-epidididymitis). The causative agent of orchitis may be a bacterium or a virus.
Possible bacterial infections include gonorrhea and chlamydia, sexually transmitted diseases. In contrast, the most common viral cause of orchitis is mumps.
When the testicles become inflamed, their temperature increases and causes alteration in the production of spermatozoa (spermatogenesis). Therefore, orchitis can cause difficulty in the male when trying to get pregnant.
We recommend you visit the following article to read more in-depth information: What is testicular orchitis - symptoms, causes and treatment.
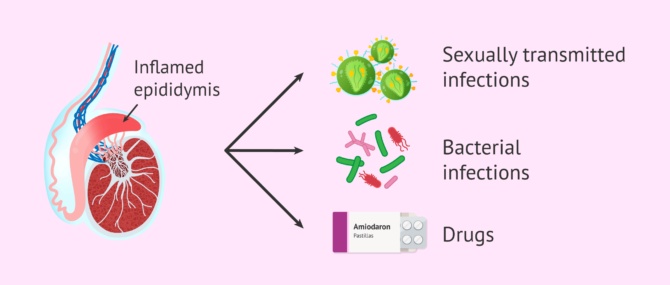
Epididymitis
Epididymitis is the inflammation of the epididymis, the structure that connects the testicle to the vas deferens. In addition, the epididymis is where sperm mature.
Generally, this enlargement of the epididymis is caused by the spread of a bacterial infection originating in the urethra or bladder. The most common microorganisms that cause epididymitis in young men are Neisseria gonorrhoeay Chlamydia trachomatis. In contrast, in boys and older men, Escherichia coli is the most common organism of epididymal inflammation.
However, epididymitis can also be caused by other microorganisms such as ureaplasma or Mycobacterium tuberculosis, as well as by a drug called amiodarone.
When a case of epididymitis is diagnosed in a man, he will be treated. Most commonly, the healing process of epididymitis leads to fibrosis and, therefore, obstruction. In this case, the sperm would not be able to go outside and azoospermia would occur, i.e., absence of sperm in the ejaculate.
If you want more detailed information about this pathology, we recommend you to visit the following link: Epididymitis or inflammation of the epididymis.
Prostatitis
Prostatitis is a group of diseases affecting the prostate that have similar symptoms. These include pain or discomfort in the perineal region and genitourinary tract, urinary problems, urine turbidity, sexual dysfunction, etc.
This condition is not always caused by an infection, nor does it necessarily involve inflammation of the prostate. Thus, prostatitis can be divided into four categories:
- Acute bacterial prostatitis: this is an acute infection of the prostate.
- Chronic bacterial prostatitis: it is due to an inadequately treated acute prostatitis or recurrent urinary tract infection.
- Chronic non-bacterial prostatitis or chronic pelvic pain syndrome: symptoms of prostatitis are present but the cause is not an infection. It may present with or without inflammation.
- Asymptomatic inflammatory prostatitis: infection and inflammation occur but there are no symptoms.
In cases where prostatitis is caused by a bacterial infection, the diagnosis is simple and in its acute form the treatment is effective. However, in chronic non-bacterial forms, the origin is not entirely clear. Therefore, the diagnosis and treatment of chronic non-bacterial prostatitis is complicated.
If you wish to continue reading about this pathology, you can access this article What is prostatitis?
Seminal vesiculitis
Seminal vesiculitis is the inflammation of the seminal vesicles, this inflammation is due to the extension of an infection from another area of the genitourinary system, such as prostatitis, urethritis or epididymitis. Rarely, seminal vesiculitis is an independent disease.
This condition can be a cause of male infertility, as it can affect sperm quality. Sometimes, men are not aware of this problem until they have been having sex for a year without getting pregnant.
How can an infection affect fertility?
An infection in the reproductive tract and organs can cause a reduction in male fertility for various reasons. Each of them is listed below:
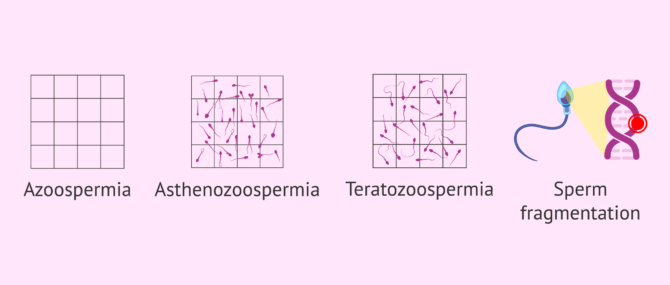
- Impede sperm formation: if the infection affects the testicles, as occurs with orchitis, spermatogenesis may be impaired, causing oligospermia or secretory azoospermia.
- Seminal tract obstruction: can cause oligospermia or obstructive azoospermia by preventing the normal outflow of spermatozoa.
- Alteration of sperm motility: microorganisms can adhere to the spermatozoa and cause asthenozoospermia, so their movement to the egg may be hindered.
- Alteration of sperm morphology: spermatozoa are continuously produced in the testicle by a process called spermatogenesis. It lasts 60 to 75 days and, if there is an infection that affects the formation of spermatozoa, an alteration in their shape (teratozoospermia) may occur. Alterations in the shape can impede its movement to the egg and fertilization.
- Increased sperm DNA fragmentation: DNA strands that are tightly packed in the head of the spermatozoon undergo small cuts that appear to negatively affect fertilization and embryo implantation capacity.
- Formation of anti-sperm antibodies: this causes sperm agglutination and reduces the chances of fertilizing the egg.
Likewise, infections of the male genital tract can be spread through the semen, so they can infect the woman's reproductive organs and affect her fertility as well.
Treatment of seminal infections
In most cases, seminal infections can be treated and cured with antibiotics. Anti-inflammatory drugs may also be administered to reduce inflammation and analgesics to relieve pain.
When a seminal infection is diagnosed, it is best to avoid sexual intercourse until treatment is complete and the infection is eliminated. If medical recommendations are not followed, the infection can recur and lead to complications in your reproductive health.
When fertility treatment is initiated, and these tests are positive for any infection, it is imperative to detect the infectious agent and eliminate it before beginning assisted reproductive procedures. It is necessary to wait for the leukocyte levels in semen to return to normal values before starting a reproductive treatment.
Because the organism is suffering from an infection, seminal parameters may be affected and not representative, so that the ideal assisted reproductive technique cannot be indicated. If male fertility is not restored, in vitro fertilization (IVF) or ICSI may be used.
Assisted procreation, as any other medical treatment, requires that you rely on the professionalism of the doctors and staff of the clinic you choose. Obviously, each clinic is different. Get now your Fertility Report, which will select several clinics for you out of the pool of clinics that meet our strict quality criteria. Moreover, it will offer you a comparison between the fees and conditions each clinic offers in order for you to make a well informed choice.
If the infection is severe, because it has not been eliminated with antibiotics in its initial phase, surgery may be necessary to try to repair the damage. In acute processes in which the infection has not been stopped in time, it may result in permanent infertility
FAQs from users
Do they look for semen infections before assisted reproduction treatment?
Yes, initially, semen parameters compatible with infection (leucocytes in the semen, appearance of the semen, etc.) are looked for and, depending on these findings, it is decided whether or not to culture the semen in search of pathogenic microorganisms. Seminal infections reduce semen quality and, therefore, the chances of success in an assisted reproduction technique.
What effect does a seminal infection in semen have on fertility?
Seminal infections can be an important factor in male sterility. We speak of seminal infection when germs are present in the semen. These pathogenic micro-organisms in the semen can come from any part of the seminal tract, mainly the urethra, prostate, seminal vesicles and/or epididymis.
Infections at these levels can cause, by different mechanisms, a deterioration of semen quality. At the level of the seminogram, this results in a decrease in semen quantity, a reduction in sperm motility (asthenoazoospermia), altered sperm morphology (teratospermia) and increased sperm DNA fragmentation.
Can prostatitis cause infertility?
Yes, prostatic fluid forms part of the seminal fluid that is expelled during ejaculation and is essential for the survival and mobility of spermatozoa during their journey to the egg. If there is an infection and/or inflammation of the prostate, the seminal fluid may not contain the necessary prostatic component and therefore natural conception may be complicated. Also, the presence of micro-organisms can affect the quality of the spermatozoa.
How do I know if I have epididymitis?
The most common sign of epididymitis is pain in one of the testicles. It is also common to have testicular swelling, redness, painful urination or blood in the urine. It is advisable to consult a doctor in the event of any discomfort or symptoms of this type.
Can there be inflammation in the seminal ducts?
Yes, infection of the vas deferens is called deferentitis. This infection can be caused by a bacterial infection and usually occurs along with epididymitis. Infection can also occur in other tubes through which semen passes: the urethra (urethritis) and the ejaculatory duct.
Suggested for you
As we have discussed throughout the article, semen infections can cause sterility at the testicular level in the male. If you want to learn more about this male factor of infertility, we recommend you to visit the following article: Male infertility due to a congenital or acquired testicular factor.
In addition, seminal infections can affect sperm quality and cause sperm DNA fragmentation. If you want to continue reading information about this topic, we invite you to access this link: Sperm DNA Fragmentation and its causes in fertility.
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
C Keck, C Gerber-Schäfer, A Clad, C Wilhelm, M Breckwoldt. Seminal tract infections: impact on male fertility and treatment options. Hum Reprod Update. Nov-Dec 1998;4(6):891-903. doi: 10.1093/humupd/4.6.891.
Massimo Tonolini, Sonia Ippolito. Insights Imaging. 2016 Oct;7(5):689-711. doi: 10.1007/s13244-016-0503-8. Epub 2016 Jun 7.
Michael Solomon, Ralf Henkel. Semen culture and the assessment of genitourinary tract infections. Indian J Urol. Jul-Sep 2017;33(3):188-193. doi: 10.4103/iju.IJU_407_16.
Stefan Stephanus Du Plessis, Sheila Gokul, Ashok Agarwal. Semen hyperviscosity: causes, consequences, and cures. Front Biosci (Elite Ed). 2013 Jan 1;5:224-31. doi: 10.2741/e610.
FAQs from users: 'Do they look for semen infections before assisted reproduction treatment?', 'What effect does a seminal infection in semen have on fertility?', 'Can prostatitis cause infertility?', 'How do I know if I have epididymitis?' and 'Can there be inflammation in the seminal ducts?'.
Authors and contributors







I am a male who has been diagnosed with infertility.
My results:
Sperm motility 30%
Volume 4 ml
WBC 15-20/pr
PH 7.8
Culture: staphylococcus Aureus’s. So, what antibiotic is effective for my treatment?