Male infertility is defined as the inability of the sperm to fertilize the oocyte and, therefore, cause a pregnancy in the woman. There are several factors that can lead a man to be infertile. Testicular disorders, including damage to the testes, are one of these factors.
By testicular causes for male infertility we refer to the factors that can affect the testicles and have a direct impact on the reproductive function.
Testicular diseases may be caused by congenital disorders, if present from birth, or by external agents that affect the man throughout his lifetime.
Provided below is an index with the 7 points we are going to expand on in this article.
- 1.
- 1.1.
- 1.2.
- 1.3.
- 2.
- 2.1.
- 2.2.
- 2.3.
- 2.4.
- 2.5.
- 3.
- 4.
- 4.1.
- 4.2.
- 4.3.
- 4.4.
- 4.5.
- 5.
- 6.
- 7.
Genetic disorders
Sperm formation, also known as spermatogenesis, is a complex process that occurs in the testicles. For this reason, any alteration in their function is likely to alter spermatogenesis and lead to alterations in sperm parameters, including sperm count, motility, morphology, and other defects.
If the cause of testicular failure is congenital (present from birth), it is usually caused by chromosomal alterations or gene mutations. Genetic diseases are likely to be transmitted from parents to children, including infertility.
Infertility or sterility may be acquired in spite of being due to genetic causes. Commonly, this type of infertility is due to problems during fertilization, due to a failed chromosome distribution or recombination. This may result in an embryo that is compatible with life, but that carries a genetic disease.
The following is a list of the most common genetic causes of male sterility that lead to testicular failure:
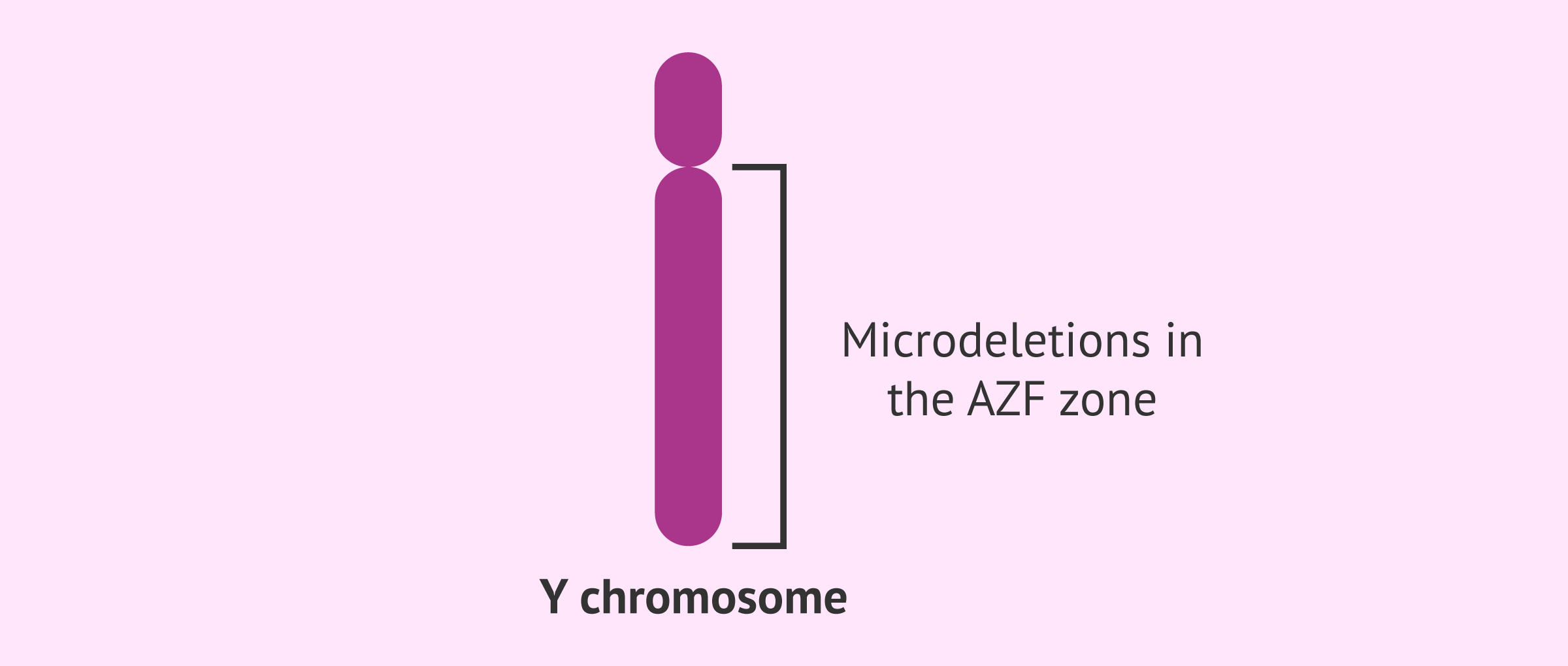
Y chromosome microdeletion (YCM)
The Y chromosome can only be found on males and is smaller in size than other chromosomes. When an embryo receives the Y chromosome from the father instead of the X, the woman gets pregnant with a boy.
The Y chromosome contains the genes that will lead to the formation of the testicles in a chromosomal region called AZF. Alterations in this region or absence of the most important genes can cause the male to suffer severe testicular factor infertility, often associated with oligozoospermia or complete secretory (non-obstructive) azoospermia.
Moreover, in case these males have children through Assisted Reproductive Technology (ART), it should be taken into account that the future baby would also inherit this condition. In other words, he will be infertile.
If you need to undergo IVF to become a mother, we recommend that you generate your Fertility Report now. In 3 simple steps, it will show you a list of clinics that fit your preferences and meet our strict quality criteria. Moreover, you will receive a report via email with useful tips to visit a fertility clinic for the first time.
Klinefelter syndrome
Klinefelter syndrome (KS) is a chromosomal disease that occurs when males have an extra X chromosome, that is, instead of having an XY pair, the baby has three chromosomes. Given that their genotype is XXY, KS is also known as XXY syndrome.
This leads to a failed development of the male reproductive system and the secondary sex characteristics in boys affected by KS syndrome. Moreover, they will be infertile due to azoospermia.
The treatment of KS involves administering testosterone to promote the development of muscular anatomy and other male characteristics. However, testosterone does not cure infertility caused by this chromosomal disease.
Get more info by clicking the following link: Klinefelter Syndrome (XXY Syndrome) – Symptoms, Causes & Fertility.
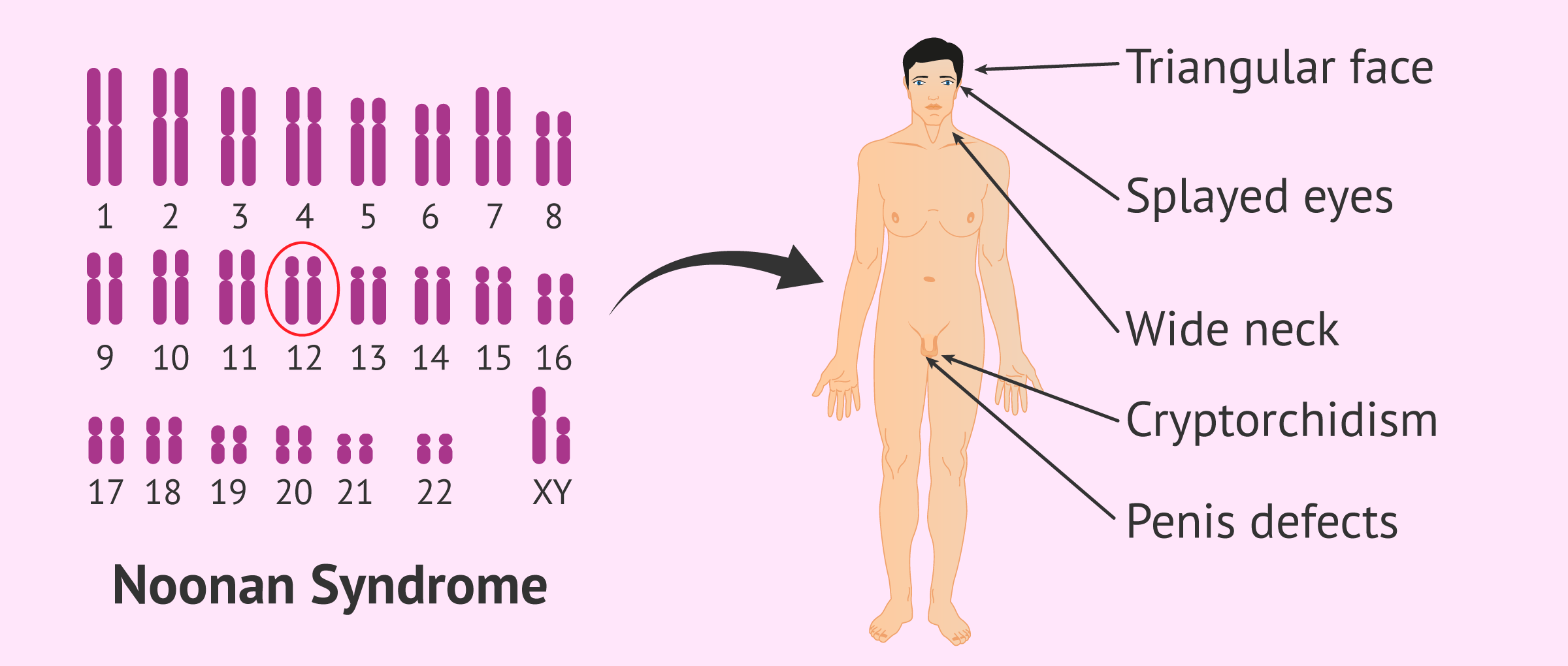
Noonan syndrome
Noonan syndrome (NS) is a congenital disorder due to a mutation of chromosome 12. It is often inherited from the mother, although it may develop in embryos resulting from gametes of healthy parents.
Children affected by this disorder experience an abnormal development of several body parts like the face and skeleton, in addition to having heart diseases after reaching puberty. Some of the most prominent physical features of individuals diagnosed with Noonan syndrome are a triangular face, wide-set eyes, broad neck, low-set ears, etc.
As for its relationship to fertility, NS-affected children can be born with defects in their penis or suffer from cryptorchidism (undescended or maldescended testis).
Diseases & conditions of the testicles
Not all testicular diseases and conditions have a genetic origin. In fact, some of them are diagnosed at birth or, conversely, they appear later in life, even during adulthood.
The following is a list of the most common types of testicular disorders:
Cryptorchidism
It is defined as the incomplete descent of one or both testicles through the inguinal canal into the scrotum.
In children born with this testicular disease, surgery to move the undescended testicle is required before they reach age 2. If this surgical procedure is not done as a baby, the male will experience problems with sperm production due to an elevated temperature of the testicles.
Cryptorchidism might appear during adulthood as a consequence of mumps, causing male infertility.
Get more info by clicking the following link: What Is Cryptorchidism?
Varicocele
It occurs when the veins of the spermatic cord that drain the testicles dilate. It is caused by alterations in the blood flow.
Varicocele may compromise male fertility depending on whether it affects one or both testicles. If only one testis is affected, it develops on the right testicle in 87% of the cases, while only 3% have varicocele on the left testicle. The remaining 10% have bilateral varicocele, in which case the grade of infertility is higher.
Males affected by varicocele can have children successfully after undergoing surgery.
See this for more: What Is Varicocele? - Symptoms & Treatment.
Orchitis or orchiditis
Orchitis or orchiditis is the swelling of one or both testicles due to an infection or a trauma. Unilateral orchitis is the most common type.
The inflammation and increased temperature of the testes that occurs as a consequence leads to an incomplete sperm production process and therefore male infertility, particularly when it is present in both testicles.
When orchitis is caused by an infection (bacterial orchitis), it can be treated with antibiotics. In such case, infertility can be reversed easily. However, mumps can increase the severity of the infertility issue.
In the worst-case scenario, orchitis may cause testicular atrofia, thereby hindering sperm production and causing the testis to be smaller in size.
Learn more: What Is Orchitis? - Definition, Causes & Symptoms.
Hydrocele
It is an excessive accumulation of fluid in the spermatic cord, particularly between the two layers that cover the testicle and the inner layer of the scrotum.
Testicular hydrocele may be congenital or acquired as a consequence of trauma, an infection, or cancer. Also, it may be unilateral or bilateral, that is, be present in one or both testicles, and be accompanied by an inguinal hernia.
In all cases, hydrocele may disappear on its own or treated if the patient has symptoms. Although it does not cause infertility by default, it may appear as a symptom of other conditions that do cause male infertility.
Related content: What Causes Hydrocele? - Symptoms & Treatment.
Germ cell aplasia
Germ cell aplasia, also called germinal cell aplasia or Sertoli-cell-only (SCO) syndrome, is a congenital disease that occurs at embryo stage as a consequence of a failure during the formation of the testicles. As a result, the testes are smaller than usual.
It is typically found at or soon after puberty, when the testes are smaller than normal adult testes.
Other external factors
Aside from the causes explained above, there exist other situations that may increase the risk for the man to suffer temporary or permanent infertility. The following are the most frequent ones:
- Environmental factors
- Environmental pollutants such as street drugs, alcohol, or tobacco can affect the cells that promote sperm production in the testis.
- Medications and treatments
- Cancer treatments such as chemotherapy and/or radiotherapy can affect the testicles and cause infertility. Other drugs to treat serious diseases can have a negative impact, too.
- Laptop use
- It may the increase of the temperature and hinder sperm production, since the production function of the testicles is conducted at a temperature of between 2 and 4 °C below the normal body temperature.
- Cycling
- A recent study has concluded that bike riding can affect the testicles due to the use of tight clothes and an incorrectly positioned bicycle saddle.
FAQs from users
What symptoms are associated with infertility due to testicular factor?
Male infertility is responsible for almost half of all reproductive problems today. Specifically, infertility at the testicular level refers to problems that directly influence the testicles.
The most common reasons for male fertility problems at the testicular level are Y-chromosome microdeletions and Klinefelter's syndrome, which often cause oligoasthenozoospermia or azoospermia (complete absence of sperm). However, these are not the only causes of male infertility at the testicular level.
Read more
What is congenital testicular factor male infertility?
In the case of male infertility of testicular origin, there are two different origins. On the one hand, there is the congenital origin in which the problem of infertility in the male is present from the birth of the individual.
On the other hand, male infertility due to testicular factor can also have an acquired origin, that is, throughout the male's life is when the cause of infertility occurs.
The most common causes of congenital male infertility of testicular cause are:
- Genetic causes
- certain genetic mutations that can be inherited from the parents or that occur de novo in embryonic development. For example, this is the case of microdeletions of the Y chromosome, Klinefelter syndrome, Noonna syndrome. Sertoli syndrome or others.
- Alterations during embryonic development without genetic cause
- can be caused by hormonal alterations in the fetus or in the mother, they can also be due to errors in the migration of germ cells in the formation of the gonads or because these cells enter apoptosis (programmed cell death of unknown cause). Alterations in embryonic development may manifest with testicular agenesis, testicular dysgenesis, cryptorchidism, oligozoospermia and / or azoospermia.

Can mumps cause infertility due to testicular factor?
Mumps, commonly called mumps, is a contagious disease caused by a viral infection. Mumps can result in meningitis, inflammation of the pancreas and inflammation of the testicles, which can lead to male infertility.
Inflammation of the testicles causes them to atrophy, so that sperm production is impaired. Therefore, the male reproductive capacity is diminished.
Is male fertility affected in men with only one testicle?
Possessing a single testicle, either from birth or due to a later occurence such as cancer, does not imply that there is a fertility problem. If the remaining testicle works correctly and the spermatogenesis is not affected, the man will be able to father a natural pregnancy without any problem.
Can testicular torsion cause infertility?
Testicular torsion refers to the twisting of the spermatic cord that supports the testicle due to a blow or bad maneuver, for example when riding a bicycle. The consequence of this is inflammation and interruption of the blood supply to the testicle. Therefore, it can lead to serious problems if not corrected immediately, even to the loss of the testicle.
It should be noted that spermatogenesis is interrupted in the testicle after 4 to 6 hours with no blood flow.
Suggested readings
In addition to the conditions and diseases explained herein, there exist a series pre-testicular and post-testicular factors that can lead to male infertility as well. Learn more: Conditions that Cause Male Infertility.
To find out whether the man is fertile or not, he should be properly screened in order to find the potential cause. Get more info by clicking the following link: Male Fertility Testing – How Do You Know if a Man’s Sperm Is Fertile?
There exists a wide range of treatments to fight against male infertility. Obviously, the treatment of choice depends on the cause. Check out this for more information: Treating Male Infertility.
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
G.R. Dohle, T. Diemer, A. Giwercman, A. Jungwirth, Z. Kopa, C. Krausz (2010). Guía clínica sobre la infertilidad masculina. European Association of Urology 2010 (actualización en abril de 2010).
Griffin DK, Finch KA (2005). The genetic and cytogenetic basis of male infertility. Human Fertil;8(1);19-26.
Guzick DS, Overstreet JW, Factor-Litvak P, Brazil CK, Nakajima ST, Coutifaris C, et al. (2001). Sperm morphology, motility, and concentration in fertile and infertile men. N Engl J Med; 345: 1388-1393.
Juárez de Diego JF (1999). Principales causas de infertilidad masculina. En: Arrondo JL. Actualización en Andrología. Publimed Comunicación SL. Pamplona.
Male infertility best practice policy committee of the American Urological Association (AUA) (2010). The optimal evaluation of the infertile male. AUA Best Practice Statement. Revised,.
Matorras R, Hernández J (eds.) (2007): Estudio y tratamiento de la pareja estéril: Recomendaciones de la Sociedad Española de Fertilidad, con la colaboración de la Asociación Española para el Estudio de la Biología de la Reproducción, de la Asociación Española de Andrología y de la Sociedad Española de Contracepción. Adalia, Madrid.
Pierik FH, Van Ginneken AM, Dohle GR, Vreeburg JT, Weber RF (2000). The advantages of standardized evaluation of male infertility. Int J Androl; 23(6): 340-6.
Sociedad Española de Fertilidad (SEF) (2011). Manual de Andrología. Coordinador: Mario Brassesco. EdikaMed, S.L. ISBN: 978-84-7877.
World Health Organization (WHO) (2000). WHO Manual for the Standardized Investigation, Diagnosis and management of the infertile male. Cambridge: Cambridge University Press.
FAQs from users: 'What are the causes of testicular factor male infertility?', 'What symptoms are associated with infertility due to testicular factor?', 'What is congenital testicular factor male infertility?', 'Can mumps cause infertility due to testicular factor?', 'What causes testicular cancer?', 'Is male fertility affected in men with only one testicle?', 'What is testicular torsion?', 'Can testicular torsion cause infertility?' and 'What are the causes of testicular shrinking?'.
Authors and contributors
More information about Cristina Algarra Goosman










Hello, my baby was born with water in the testis… they are going to remove via surgery but i want to know if my son is going to be childless as an adult for god’s sake!!??
Dear Vanessa009,
Normally, congenital hydroceles go away on their own during the first 18-24 months of life in babies. If not, they can be removed through surgery to prevent infertility issues in the future. It doesn’t mean that your son is going to be sterile.
I hope this helps,
Best