Testicular hyperthermia, also called testicular heat stress, is a term that refers to abnormally high body temperature. Specifically, scrotal hyperthermia is the increase in temperature in the scrotal area, the sac that surrounds the testicles. This harms spermatogenesis, altering the quality of the semen and putting the male's
reproductive health at risk.
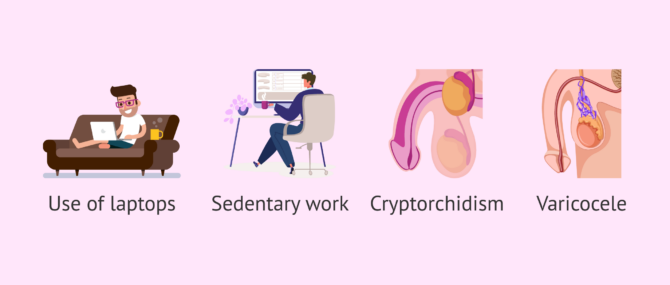
Some testicular pathologies, such as cryptorchidism or varicocele, for example, can cause testicular hyperthermia. Besides, other factors cause an increase in the temperature of the testicles, such as the use of tight clothing, exposure to heat, or the use of laptops, among others.
Provided below is an index with the 7 points we are going to expand on in this article.
- 1.
- 2.
- 2.1.
- 3.
- 4.
- 4.1.
- 4.2.
- 4.3.
- 5.
- 6.
- 7.
Definition of scrotal hyperthermia
The testicles are located in a pouch outside the abdomen called the scrotum, whose function is to maintain the ideal temperature of the testicles for the development of sperm. For this reason, the testicles are approximately two degrees below body temperature, that is, 37ºC.
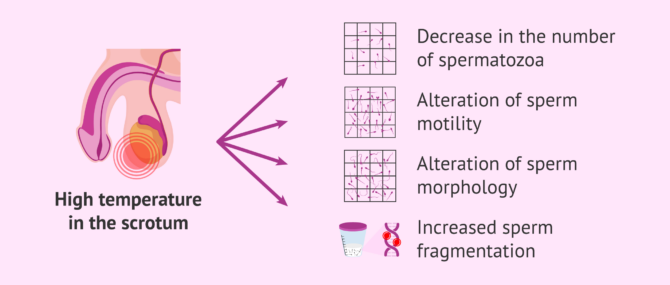
When the testicles are at a temperature higher than 35ºC it is said that there is scrotal hyperthermia and the formation of sperm is altered. Therefore, heat in the scrotal area causes a decrease in the number of spermatozoa and alterations in their mobility and morphology, apart from increasing their DNA fragmentation.
As a result of the effects of heat in the scrotal area, the ability of the sperm to fertilize the egg is reduced.
Causes of testicular hyperthermia
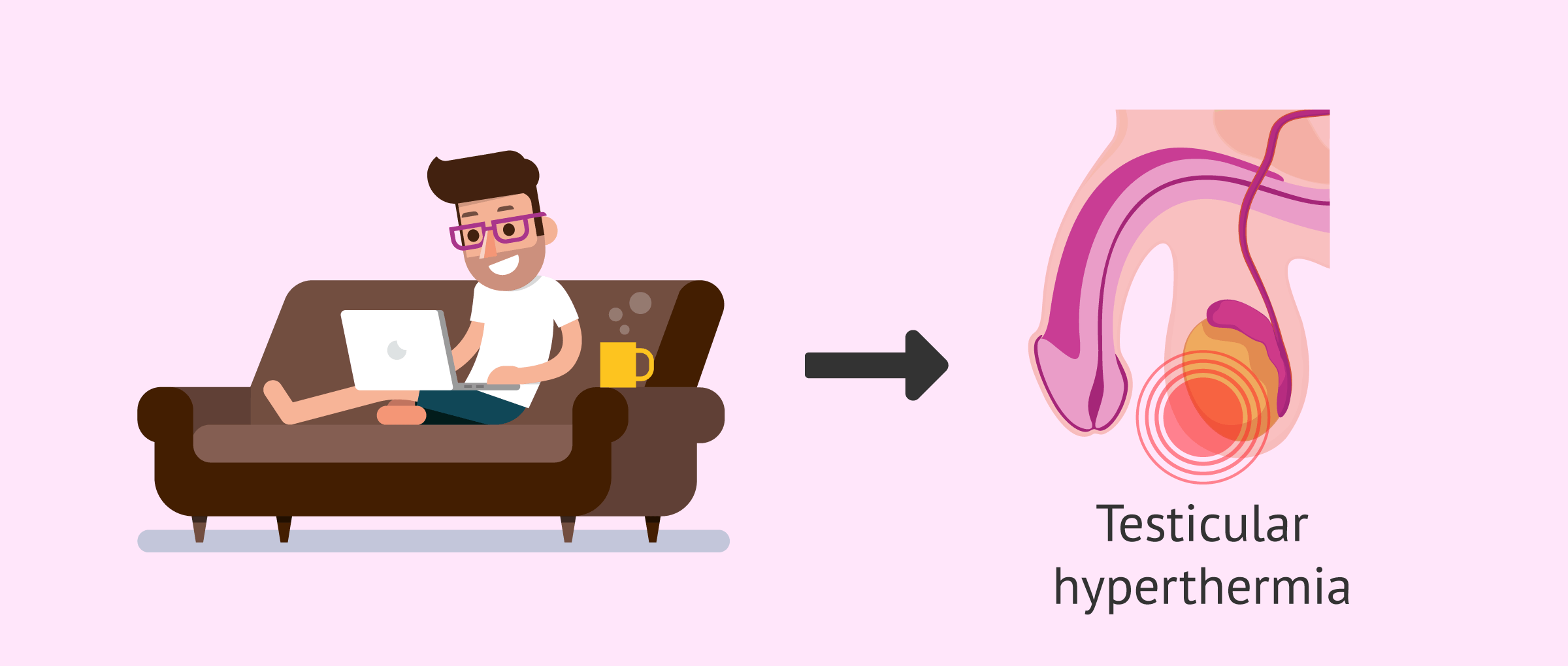
Normally, the increase in scrotal temperature is associated with certain factors such as prolonged driving, sedentary work, poor posture, and certain clothing. The increasingly frequent use of the laptop computer is another of the factors that can make the temperature of the testicles rise since it is a device that generates heat and is usually placed on the legs for long periods.
On the other hand, certain medical pathologies can generate an increase in testicular temperature. Below we detail some of these pathologies.
- Cryptorchidism
- is an incomplete descent of the testicles. The testicles must descend from the abdomen into the scrotum during the development of the embryo. When this process does not occur correctly, the testicles are subjected to an increase in temperature./dd>
- Varicocele
- is an increase in the size of the veins located in the testicles. As the veins dilate, the blood flow goes up resulting in a rise in temperature.
Laptop usage
The prolonged use of laptops on men's legs can affect their semen. These devices emit heat, which can cause abnormalities in the movement, morphology, and/or concentration of the sperm. It should be noted that the use of protective pads or covers between the legs and the laptop does not protect the testicles from heat.
This does not mean that the man will be infertile by placing the laptop on his legs at any time, but it does mean that repeated and prolonged use can cause reproductive problems in the male.
Tips to avoid hyperthermia of the scrotum
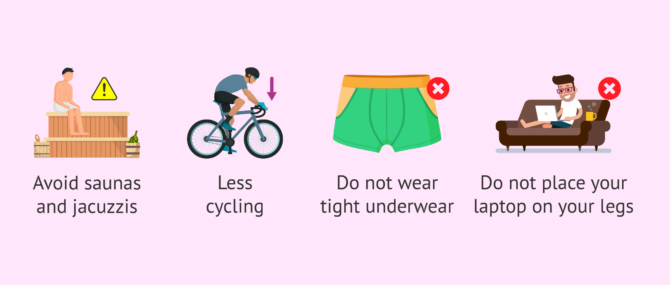
In general, to avoid raising the temperature of the scrotum it is important to change the lifestyle, eliminating anything that can negatively affect the semen.
Here are some tips for protecting your scrotum from hyperthermia:
- Avoid saunas, jacuzzis and hot baths.
- Reduce time for activities that require a lot of sitting, such as cycling.
- Do not wear tight underwear.
- Do not place the laptop on your legs.
However, it must be taken into account that there are testicular pathologies that also cause an increase in the temperature of the testicles but do not produce any symptoms. For this reason, it is recommended that men have urological check-ups.
FAQs from users
To what extent can a laptop cause male infertility?
Today there is still much ignorance as to what factors affect fertility. For example, when a male has a seminogram and it is altered, most of the time we will not know the cause.
Just like food, life habits such as exercising and not consuming toxins are very important for reproduction. We know that environmental factors can also affect, although we are not yet sure how they all affect each other.
A rise in temperature maintained in the area of the external genitalia of males can be one of the causes of poor semen quality. In this sense, laptops can be affected when used on the lap. Studies in urology describe that with more than 10-15 minutes of computer use in the lap, scrotal temperature increases considerably and this can cause problems in sperm production. Therefore, it is recommended that computers are used on the table so that this potentially damaging temperature increase does not occur.
Is the damage in sperm caused by heat reversible?
Yes. Sperm cells regenerate every 3 months. For this reason, if the male's testicles have been exposed to high temperatures for more than 3 months, the sperm formed later are not affected by the temperature rise.
How can you maintain a proper temperature in the scrotum area?
To have a good scrotal temperature it is mainly necessary to follow a healthy lifestyle and not to abuse hot baths. It is also recommended not to wear tight underwear or to reduce the time spent sitting, since having the testicles closer to the body increases their temperature. It is also advisable to avoid using laptops above the legs.
Suggested for you
Scrotal hyperthermia causes problems in the male's reproductive health. However, other conditions also affect testicular function. You can learn more about this topic at the following link: Testicular Disorders & Infertility - Impact on Reproductive Function.
Also, scrotal hyperthermia can cause problems in achieving a pregnancy. If you want to know the treatments that exist for this situation, we recommend you visit the following article: Treatments for Male Infertility.
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
Kastelic JP, Wilde RE, Bielli A, Genovese P, Rizzoto G, Thundathil J. Hyperthermia is more important than hypoxia as a cause of disrupted spermatogenesis and abnormal sperm. Theriogenology. 2019 Jun;131:177-181. doi: 10.1016/j.theriogenology.2019.03.040 (View)
Mieusset R, Fouda PJ, Vaysse P, Guitard J, Moscovici J, Juskiewenski S. Hyperthermia is more important than hypoxia as a cause of disrupted spermatogenesis and abnormal sperm. Theriogenology. 2019 Jun;131:177-181. doi: 10.1016/j.theriogenology.2019.03.040 (View)
Sheynkin Y, Welliver R, Winer A, Hajimirzaee F, Ahn H, Lee K. Protection from scrotal hyperthermia in laptop computer users. Fertil Steril. 2011;95(2):647-51 (View)
FAQs from users: 'To what extent can a laptop cause male infertility?', 'Is the damage in sperm caused by heat reversible?' and 'How can you maintain a proper temperature in the scrotum area?'.



Hi, I usually use my laptop on my legs but reading this I think I’m going to stop. How long does it take to warm up the scrotum? Thank you.
Hello couchpotatoe,
According to numerous urology studies, scrotal temperature rises when you spend more than 10-15 minutes with your laptop on your legs.
I hope I helped you.
Best regards