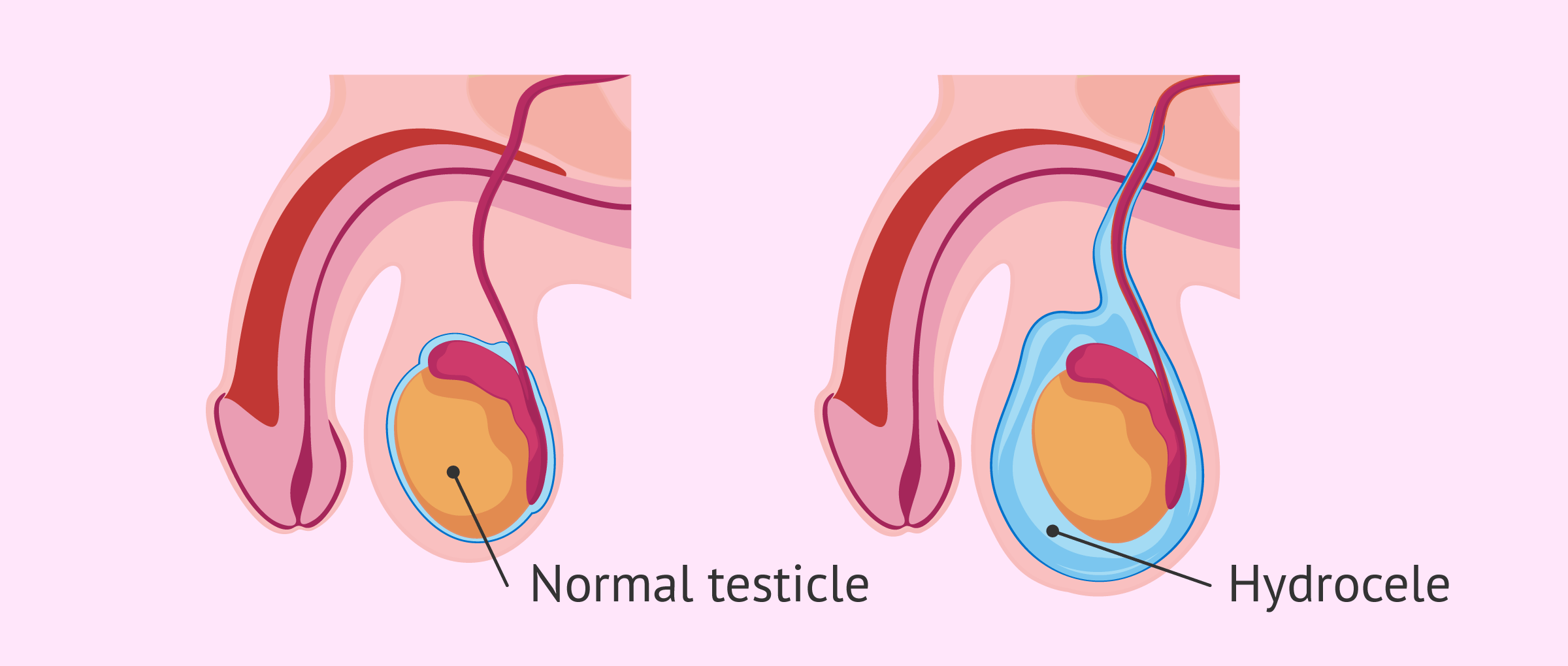
Hydrocele consists of the accumulation of anomalous fluid in some area of the body. In the case of testicular hydrocele, the most frequent, the increase in fluid occurs between the scrotal pouch and the vaginal tunic of the testicles.
A distinction is made between bilateral hydrocele, if it occurs simultaneously in both testicles, and unilateral hydrocele, if it occurs in only one of them. In this second assumption, the hydrocele can be right or left.
Provided below is an index with the 8 points we are going to expand on in this article.
- 1.
- 1.1.
- 1.2.
- 2.
- 3.
- 3.1.
- 3.2.
- 4.
- 5.
- 5.1.
- 5.2.
- 5.3.
- 5.4.
- 5.5.
- 5.6.
- 5.7.
- 6.
- 7.
- 8.
Types and causes
The testicles are inside a pouch called the scrotum. There, they are immersed in a small amount of liquid that helps make them mobile and less vulnerable to shocks.
We speak of testicular or scrotal hydrocele when the amount of fluid in this area is greater than normal.
There are two main causes of hydrocele that give rise to the two basic types of this pathology: congenital hydrocele and acquired hydrocele.
Congenital hydrocele
Congenital hydrocele is the hydrocele that appears in newborn babies. It is the most common type of testicular hydrocele and is also known as communicating hydrocele.
It occurs when the vaginal tunic of the testicle is not completely closed, so that communication with the peritoneal cavity is preserved and this leads to fluid flowing into the scrotal cavity.
During normal development, the testicles descend through a tube from the abdomen to the scrotum. In this case, hydroceles are formed when this duct fails to close and fluid flows from the abdomen through the open duct and accumulates in the scrotum. For this reason, the testicle looks swollen.
Congenital hydrocele may or may not be accompanied by an inguinal hernia.
Congenital hydrocele is very common in infants, but usually disappears between 18 and 24 months of age. If this is not the case, surgery is required.
Acquired hydrocele
In contrast to the previous type, this is known as non-communicating hydrocele. The main reason for the accumulation of fluid is an inflammation caused by various reasons such as infection, testicular torsion, trauma, epididymitis, tumor, etc.
Surgery on the testicular area, such as vasectomy, varicocele intervention or inguinal hernia, may also be the cause of hydrocele.
Acquired hydrocele occurs in children and adults. It most often appears in men aged 40 and older.
Symptoms and Diagnosis
The clinical manifestations of hydrocele are inflammation or painless swelling of the affected testicle or both testicles, in the case of bilateral hydrocele.
Sometimes, this inflammation can cause pain and redness in the area. However, these symptoms are usually mild and do not prevent daily routines.
The diagnosis of hydrocele should be made by a urologist, who will perform the following tests:
- Palpation
- the circulating fluid makes the testicle very soft and not noticeable when touched. When the scrotal pouch is carefully palpated, the doctor will perceive the swelling, but that the testicle has a normal volume inside the scrotum. Also, if there is a variation in the amount of fluid, it is usually due to an inguinal hernia.
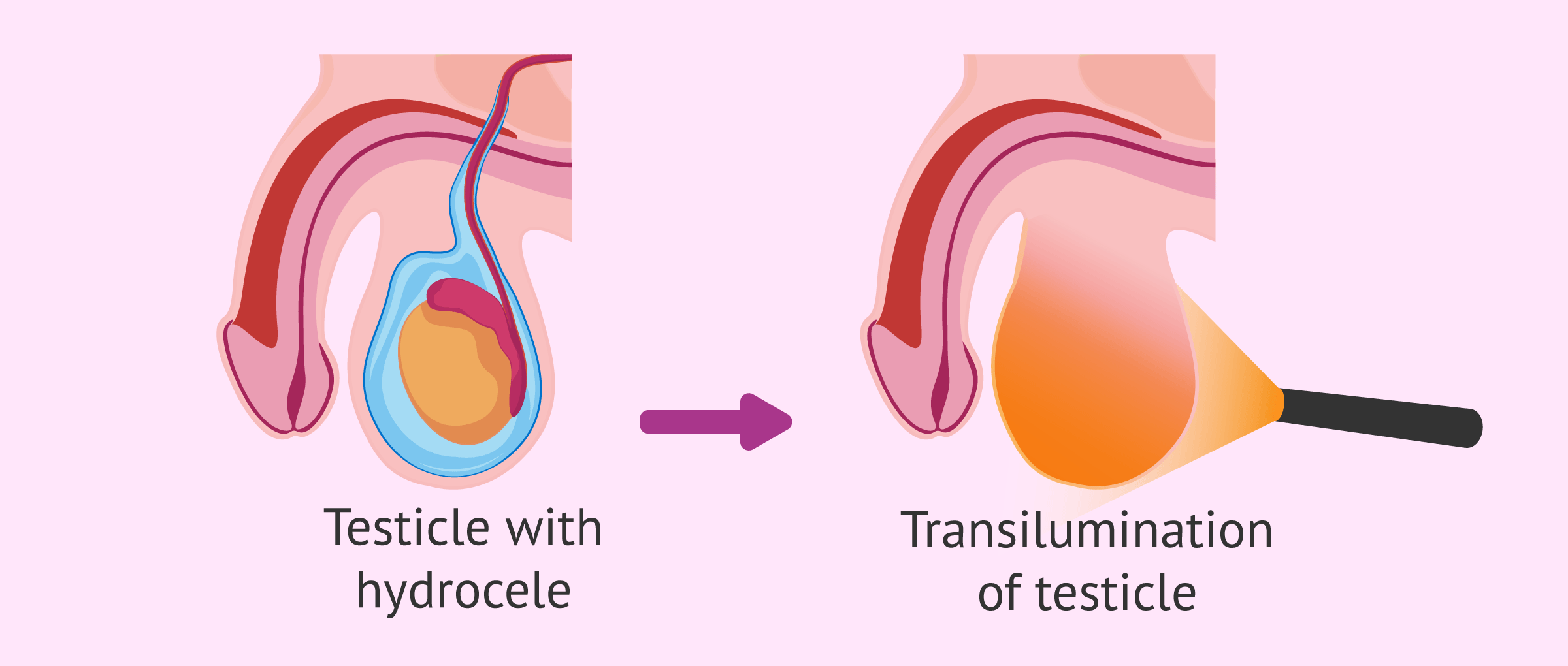
- Transillumination of the scrotum
- is a diagnostic test that involves applying a light source behind the scrotal pouch to illuminate it. When there is a testicular hydrocele, the scrotum lights up because it is filled with clear fluid.
- Ultrasound
- is used to confirm the diagnosis and to check that there is no testicular tumor.
In addition to these tests, the specialist may decide to order blood and urine tests to check for infection as a possible cause of the hydrocele.
Treatment
Hydrocele is usually not dangerous and is only treated when it causes great discomfort, embarrassment, or when the testicles become so large that they compromise blood supply.
A simple hydrocele usually disappears without treatment. However, there are cases where intervention is needed.
In the next section, we are going to comment on the two operations currently used to eliminate hydrocele.
Hydrocelectomy
It is an ambulatory surgery of low complexity and with excellent results. The only handicap is that it requires general or epidural anesthesia.
Broadly speaking, surgery involves making a slight incision in the scrotum or lower abdomen, removing excess fluid through it, and removing some of the tissue to prevent it from filling up again.
The complications that can arise from operating the hydrocele with the hydrocelectomy technique are the following:
- Blood clots
- Infection
- Injury to the scrotal tissue or structures
The duration of the hydrocelectomy usually lasts about 30 minutes and the patient can return home the same day of surgery. Once at home, the patient can put ice on the area to reduce swelling and take analgesics for pain if indicated by your specialist.
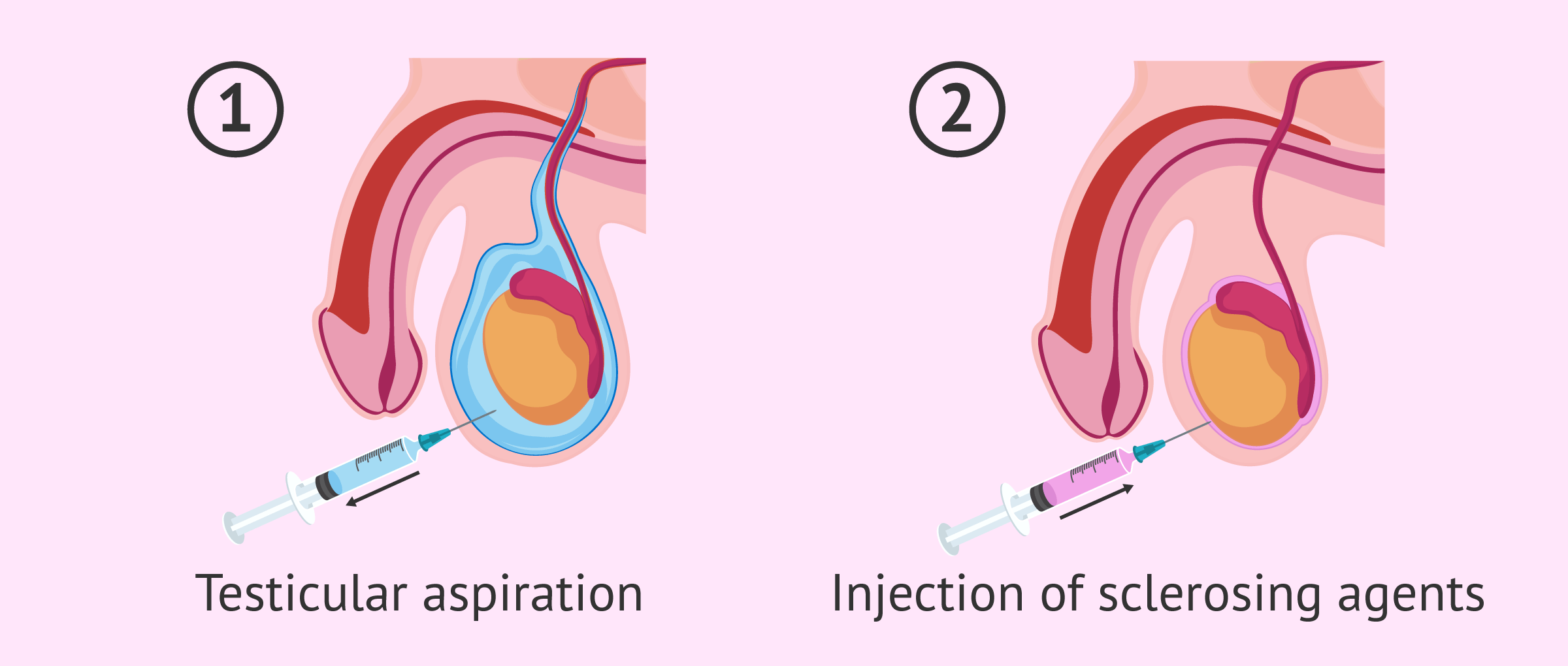
Testicular aspiration
The other treatment option is to remove fluid from the scrotum with a needle, which is known as testicular aspiration.
This aspiration is usually combined with sclerotherapy, which involves injecting sclerosing drugs (which harden or thicken) to close the opening. The benefit of using this technique is that it helps prevent further accumulation of fluid.
The risks associated with aspiration and sclerotherapy are as follows:
- Fibrosis
- Infection
- Mild or moderate pain in the scrotal area
- Return of the hydrocele
Ultimately, because of the high risk of infection and the high likelihood that the hydrocele will come back, surgery is usually preferred. Aspiration may be a good alternative for people who have certain surgical risks.
In addition, hydroceles that appear with an inguinal hernia should be surgically repaired as quickly as possible and a hernioplasty should be performed.
Hydrocele and fertility
Hydrocele is not a direct cause of infertility, nor does it usually drastically affect a man's reproductive capacity.
In spite of this, there are cases of hydrocele in which other factors that do influence fertility are compromised, such as an infection.
Therefore, hydrocele could indirectly hinder pregnancy and, in these cases, the option of surgery should be considered.
FAQs from users
I have hydrocele - will I be sterile?
Hydrocele is the accumulation of fluid between one of the layers of the testicle (vaginal tunic) and the scrotum of one or both testicles. It can be congenital (affects babies at birth) or acquired, i.e. secondary to infections, trauma, tumors, surgeries on the testicle, etc.
In most cases the hydrocele is presented as an inflammation of the testicle, not painful or causing mild discomfort. In itself, it is not a cause of sterility but certain cases, such as those caused by an infection, can reduce the reproductive capacity.
Does hydrocele affect male fertility?
By itself, hydrocele should not have a major impact on male fertility. However, a variation in testicular temperature may occur, which could affect sperm production.
Read more
What is spermatic cord hydrocele?
Spermatic cord hydrocele, also known as cord cyst, is a type of hydrocele in which fluid accumulation occurs along the spermatic cord, i.e., in the upper part of the scrotum.
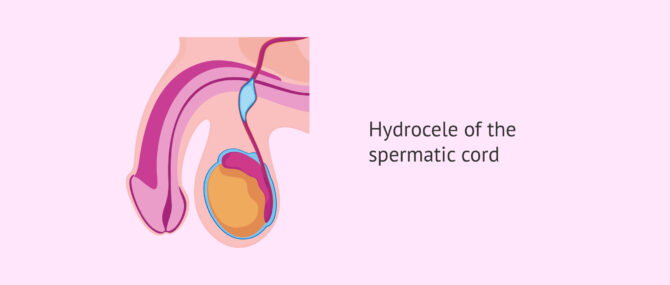
In addition, there are two other subtypes: funicular hydrocele and cystic hydrocele, depending on whether or not the accumulated fluid communicates with the peritoneum.
Are varicocele, spermatocele and hydrocele the same things?
No, all three concepts refer to testicular pathologies but they are not the same.
Varicocele refers to inflammation and enlargement of the veins that drain the testicle and the hydrocele indicates the accumulation of fluid in the scrotal pouch. Spermatocele is a benign cyst that forms in the epididymis.
How long after the hydrocele procedure can I have sex?
This is something that varies between patients, because depending on the size of the hydrocele, the existence or not of complications, the speed of healing, etc. the postoperative will be more or less long.
In any case, it does not usually last longer than 2-3 weeks.
Can homeopathy cure hydrocele?
Homeopathy can help the hydrocele disappear on its own, which is what happens in most cases. However, if the hydrocele does not disappear, a hydrocelectomy will be necessary.
Can hydrocele cause complications?
Hydrocele is a benign process and no complications are generally associated with it. However, on rare occasions, testicular ischemia may occur. This is a deficit in the blood supply to the testicle, which would lead to impair its function.

In addition, if the hydrocele is operated, a hematoma may appear in the scrotal area, infection of the wound or even reproduction of the hydrocele.
Suggested for you
In addition to hydrocele, there are other pathologies that affect testicular function and can affect infertility. If you want to know more about this topic, we recommend you read the following post: Male infertility due to testicular factor.
If you're interested in the tests that are used to evaluate male fertility, don't miss this article: What are male fertility tests?
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
Gaku Yamamichi, Koichi Tsutahara, Takuya Okusa, Ayumu Taniguchi, Nozomu Kishimoto, Go Tanigawa, Tetsuya Takao, Seiji Yamaguchi. Traumatic Testicular Rupture Complicated with Hydrocele: A Case Report. Hinyokika Kiyo. 2015 Oct;61(10):411-3.
Irene Chen, Sohrab Arora, Kenan Alhayek, David Leavitt, Ali Dabaja. Diagnosis and management of testicular compartment syndrome caused by tension hydrocele. Urol Case Rep. 2022 Apr 25;43:102091. doi: 10.1016/j.eucr.2022.102091 (View)
Jerzy Niedzielski, Maciej Nowak, Piotr Kucharski, Katarzyna Marchlewska, Jolanta Słowikowska-Hilczer. Testicular, Epididymal and Vasal Anomalies in Pediatric Patients with Cryptorchid Testes and Testes with Communicating Hydrocele. J Clin Med. 2022 May 26;11(11):3015. doi: 10.3390/jcm11113015 (View)
K Suzuki, Y Shioji, T Morita, A Tokue. Primary testicular plasmacytoma with hydrocele of the testis. Int J Urol. 2001 Mar;8(3):139-40. doi: 10.1046/j.1442-2042.2001.00269.x (View)
Ioannis Patoulias, Efstathios Koutsogiannis, Ioannis Panopoulos, Panagiota Michou, Thomas Feidantsis, Dimitrios Patoulias. Hydrocele in Pediatric Population. Acta Medica (Hradec Kralove). 2020;63(2):57-62. doi: 10.14712/18059694.2020.17 (View)
Martin Kaefer, Deepak Agarwal, Rosalia Misseri, Benjamin Whittam, Katherine Hubert, Konrad Szymanski, Richard Rink, Mark P Cain. Treatment of contralateral hydrocele in neonatal testicular torsion: Is less more? J Pediatr Urol. 2016 Oct;12(5):306.e1-306.e4. doi: 10.1016/j.jpurol.2015.07.009. Epub 2015 Sep 5 (View)
FAQs from users: 'I have hydrocele - will I be sterile?', 'Does hydrocele affect male fertility?', 'What is spermatic cord hydrocele?', 'Are varicocele, spermatocele and hydrocele the same things?', 'How long after the hydrocele procedure can I have sex?', 'Can homeopathy cure hydrocele?' and 'Can hydrocele cause complications?'.