Cryptorchidism or undescended testicle is a congenital anomaly in the male. It is characterized by one or both testicles not descending correctly, remaining in the abdominal cavity or inguinal canal instead of reaching the scrotum.
This anomaly is common in premature infants and, in most cases, is right unilateral cryptorchidism. In adults, cryptorchidism may result in impaired male fertility.
Provided below is an index with the 9 points we are going to expand on in this article.
- 1.
- 2.
- 3.
- 4.
- 5.
- 5.1.
- 6.
- 6.1.
- 6.2.
- 6.3.
- 6.4.
- 6.5.
- 6.6.
- 7.
- 8.
- 9.
What is cryptorchidism?
Cryptorchidism is the absence of at least one of the two testicles in the scrotum due to an altered descent of the testicles during fetal development. It is the most common congenital malformation of the external male genitalia. Cryptorchidism is asymptomatic, that is, it does not cause symptoms. The only thing the patient may notice is the empty scrotal sac.
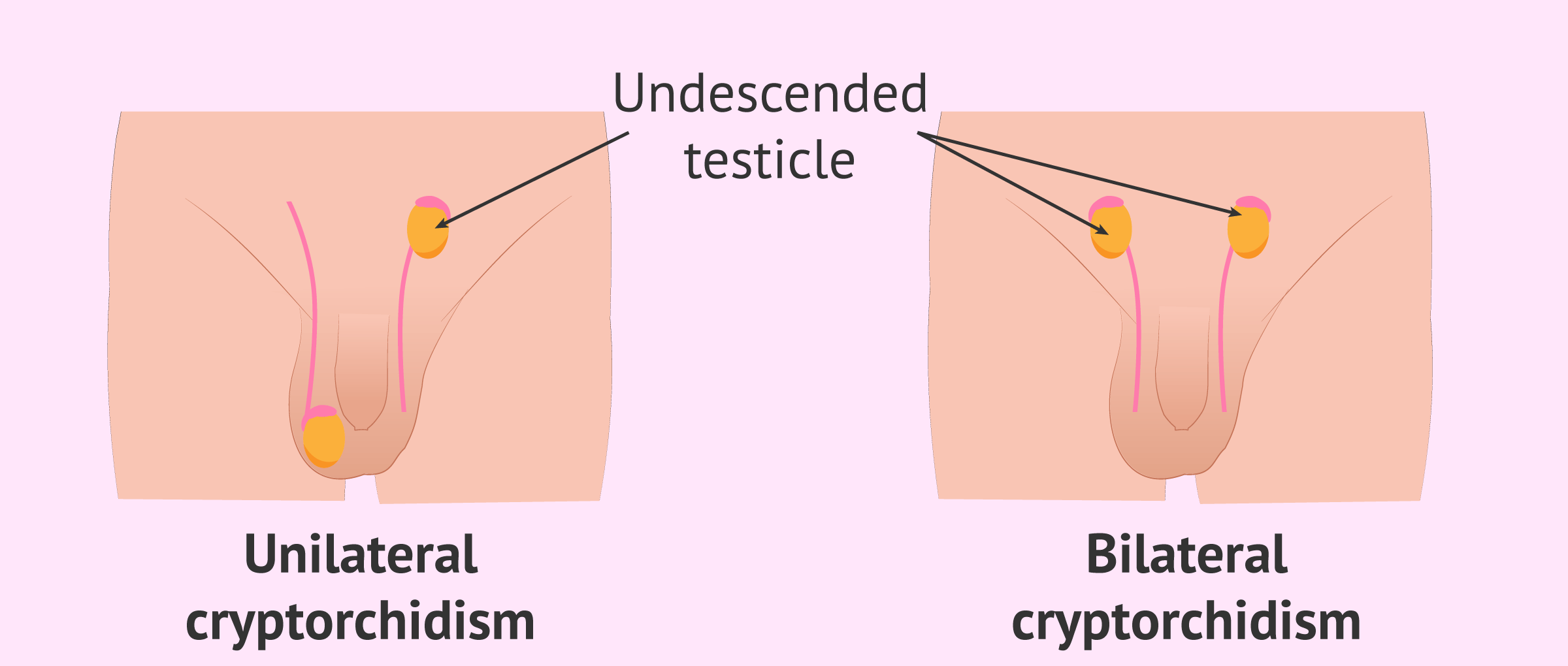
Two types of cryptorchidism are distinguished:
- Unilateral cryptorchidism
- only one of the two testicles does not descend correctly. This is the most common form, accounting for 85% of cases. In addition, it is more frequent that the right testicle is affected. Approximately 70% of cryptorchidism cases are unilateral.
- Bilateral cryptorchidism
- neither testicle descends into the scrotum. Cases of bilateral cryptorchidism are less common, accounting for only 15%.
This anomaly is found with a frequency of 3 to 9% in term newborns and approximately 30% in premature infants. In most cases, the descent of the testicle will occur spontaneously before the first 12 months of the baby's life. In fact, in up to two-thirds of the cases, they descend before 4 months of age. Only 0.8-2% of children have cryptorchidism after the first year of life.
Most commonly, the testicle is found along the path it should have followed to descend into the scrotum, the most common location being the inguinal region (80% of cases).
Why does cryptorchidism occur?
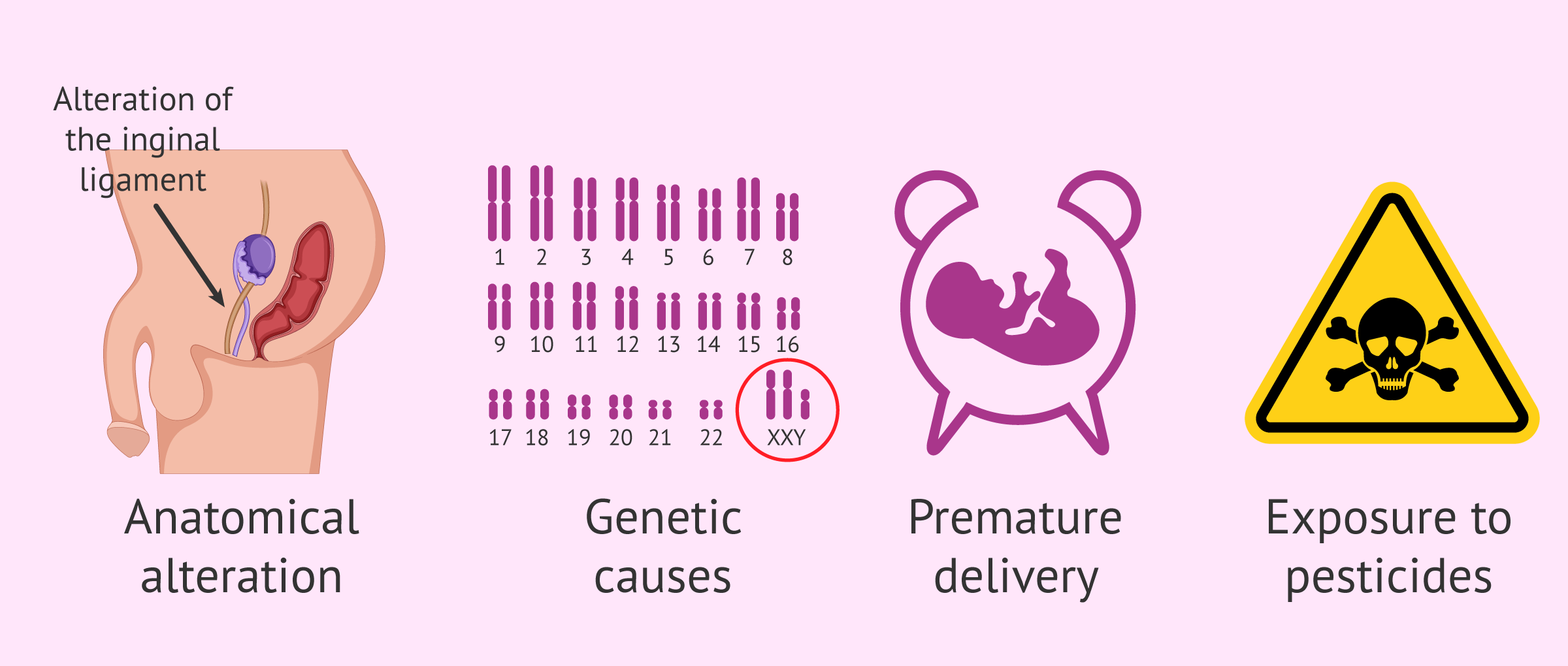
Cryptorchidism or occult testicle can have different origins, many of them hereditary. The main causes of cryptorchidism are listed below:
- An anatomical alteration, such as an anomaly of the gubernaculum testis (scrotal ligament).
- A mechanical obstacle encountered during testicular migration, such as sperm vessels or nerves, or a very narrow inguinal canal.
- Obstruction of the scrotal orifice.
- Hormonal defect or insufficiency, since gonadotropins are needed for the normal development of the genital tract: deficiency of AMH, hCG, LH, FSH, testosterone, etc.
- Lack of intra-abdominal pressure.
- Genetic or chromosomal causes: Klinefelter syndrome, Prader-Willi syndrome, Kallman syndrome, alterations in the Y chromosome, etc.
Apart from this, there are also factors that increase the risk of the testicles not descending. This is the case of low birth weight, alcoholism of the mother during pregnancy, smoking, exposure to toxic substances such as pesticides, etc.
Diagnosis of cryptorchidism
Generally, the diagnosis of cryptorchidism is made by palpation of the scrotal sac and subsequently of the abdominal area and the inguinal canal in search of the testicle(s). This physical examination may be performed at the time of birth or later at a routine infant checkup.
In some cases, the testicle is difficult to locate and a complementary test such as an abdominal ultrasound is required. If they are not located with this test, the following studies can be performed:
- Ultrasound or ultrasound to visualize the testicles located in the inguino-scrotal tract.
- Magnetic resonance imaging (MRI): it is especially useful to locate intra-abdominal testicles.
If the testicles cannot be located by any of these tests, surgery, usually by laparoscopy, will be necessary. Normally, this surgery is performed between the baby's first and second year of life, unless there is an associated hernia and it is necessary to intervene earlier.
In the case of bilateral cryptorchidism, it is also indicated to perform hormonal determinations and to analyze the karyotype to find the cause of this alteration.
Treatment by surgery
If the testicle does not descend spontaneously during the first 12 months of life, treatment will be necessary to prevent future injury.
There is a medical treatment with hormones, such as beta-hCG and testosterone, which stimulate the decrease. However, this strategy is falling into disuse due to its side effects.
Surgery, called orchiopexy, is the current treatment of choice for cryptorchidism orchiopexy surgery, is currently the treatment of choice for cryptorchidism. This surgery is quite effective and is usually performed before 2 years of age.
There are different studies that address the relationship of surgery with subsequent male fertility and the risk of developing a testicular tumor. In both cases, those surgeries performed at an earlier age had a better prognosis.
If orchiopexy is performed at approximately 18 months of age, it positively influences fertility, since there is a greater recovery of testicular volume and a lower risk of cancer.
Consequences of undescended testicle
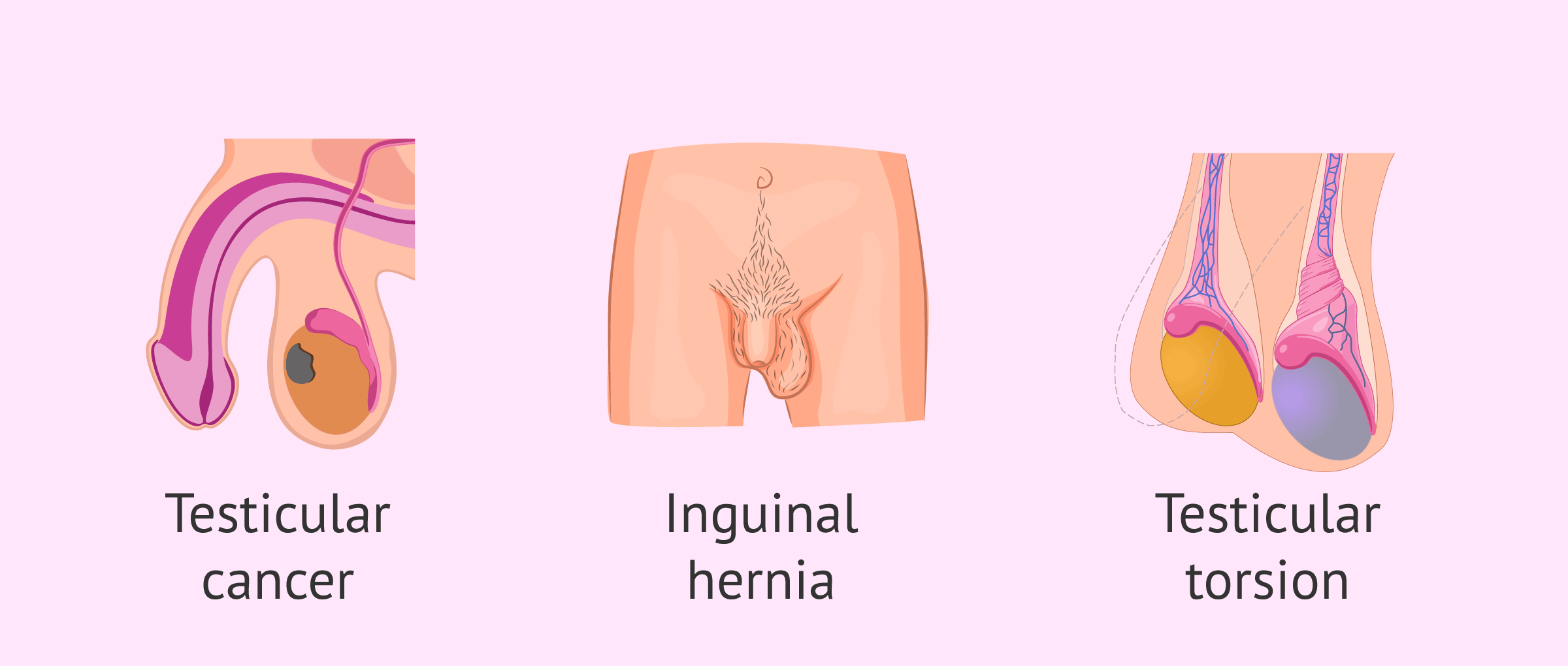
The main risks and complications derived from cryptorchidism are:
- Testicular cancer: people who have had cryptorchidism have four to five times the risk of developing a testicular tumor. There are several theories to explain this relationship. Some argue that it is due to an alteration in testicular development. Others relate it to the increase in temperature.
- Inguinal hernia: may develop in 65% of cases.
- Decreased testicular size: due to this anomaly, the testicle does not grow normally. Their growth is retarded because they are not found inside the body.
- Testicular torsion: these boys are more prone to have the spermatic cord twisted and interrupted blood supply to the testicle.
- Psychological effects on the adult male.
In addition to the consequences of undescended testicles, there are also side effects of surgery for the treatment of this disorder. It is a fairly simple surgical procedure, but like any other, bleeding, infection, injury to blood vessels, or even consequences of anesthesia may occur.
Cryptorchidism and fertility
For proper spermatogenesis (sperm production) to take place, the testicles must be at a lower temperature than body temperature. Therefore, physiologically, the testicles are located in the scrotal pouch at 33ºC.
The higher testicular temperature may cause germ cell death or failure of cell division. The consequence of both situations can be altered fertility.
The impact of cryptorchidism on fertility in the adult male depends on several factors, such as:
- Previous location of the testicle: intra-abdominal or in the inguinal canal.
- Whether it is unilateral or bilateral cryptorchidism.
- Age at which surgery is performed.
One of the most influential factors has been found to be the timing of orchiopexy. Delaying surgery significantly increases the risk that the patient's reproductive capacity will be impaired in adulthood.
Assisted procreation, as any other medical treatment, requires that you rely on the professionalism of the doctors and staff of the clinic you choose. Obviously, each clinic is different. Get now your Fertility Report, which will select several clinics for you out of the pool of clinics that meet our strict quality criteria. Moreover, it will offer you a comparison between the fees and conditions each clinic offers in order for you to make a well informed choice.
FAQs from users
Can cryptorchidism cause azoospermia?
Cryptorchidism is the incomplete descent of one or both testicles through the inguinal canal, which causes the testicles to be subjected to a higher temperature than the one existing in the scrotal sac. This increase in temperature negatively affects sperm production.
Is there a relationship between cryptorchidism and testicular cancer?
The risk of testicular cancer is 3 to 10 times higher in patients with cryptorchidism than in patients with normodescent testes, and surgical intervention to lower the testicles (orchidopexy) does not prevent future malignancy. The need for follow-up in these patients is emphasized, and removal of the testicle (orchiectomy) is recommended in post-pubertal patients.
The highest risk cases are those in which the testicle has remained inside the abdomen. The lowest risk cases are those in which the testicle was already in the groin canal, almost in the pouch, and which have undergone surgery.
It is important to diagnose the disease early. To do this, testicular self-examination should be performed, palpating the testicles in search of nodules. It is recommended to visit the family doctor or urologist once a year to perform an analysis of tumor markers that can give the alarm signal of a tumor at birth. On many occasions an abnormal result may appear without there being a tumor, so the analysis should be repeated after a few weeks and, if the abnormality persists, an ultrasound scan of the testicles should be requested.
Does unilateral cryptorchidism also affect fertility?
Yes, although the effect is less than if bilateral cryptorchidism is present. In cases where surgery is not performed, 51% of patients with unilateral cryptorchidism present alterations in the values of the seminogram (semen analysis). If surgery is performed, this percentage decreases to approximately 25%.
Is prevention of cryptorchidism possible?
Cryptorchidism cannot be prevented, as it is a developmental disorder that occurs before birth. However, its consequences can be prevented by early surgical treatment: thanks to surgery in the first year of life, the negative impact of cryptorchidism on fertility and the risk of testicular cancer can be reduced.
What types of cryptorchidism are there?
We differentiate between different types of cryptorchidism depending on its origin and the abnormal position in which the testicle is found:
- Congenital undescended testes
- Absent testicle or anorchia
- Ectopic testicle
- Acquired undescended testes
- Testicle in elevator
Is cryptorchidism hereditary?
Cryptorchidism can have different origins and among them are genetic causes. In addition, there are risk factors such as family history, low birth weight or premature delivery that are associated with an increased likelihood of cryptorchidism.
Recommended readings
As we have explained, cryptorchidism can affect male fertility. If you want to know other causes of male infertility, we recommend you to access the following link: Main types and causes of male infertility.
On the other hand, the way to evaluate the effect of cryptorchidism on male fertility is by seminogram. In this article, we explain what it consists of: What is a basic semen analysis and how is it done step by step?
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
B Gill, S Kogan. Cryptorchidism. Current concepts. Pediatr Clin North Am. 1997 Oct;44(5):1211-27. doi: 10.1016/s0031-3955(05)70554-x.
D Cortes. Cryptorchidism--aspects of pathogenesis, histology and treatment. Scand J Urol Nephrol Suppl. 1998;196:1-54.
Dina Cortes, Rune Holt, Victoria Elizabeth de Knegt. Hormonal Aspects of the Pathogenesis and Treatment of Cryptorchidism. Eur J Pediatr Surg. 2016 Oct;26(5):409-417. doi: 10.1055/s-0036-1592415.
Gilvydas Verkauskas, Dalius Malcius, Darius Dasevicius, Faruk Hadziselimovic. Histopathology of Unilateral Cryptorchidism. Pediatr Dev Pathol. Jan-Feb 2019;22(1):53-58. doi: 10.1177/1093526618789300
Hadley M Wood, Jack S Elder. Cryptorchidism and testicular cancer: separating fact from fiction. J Urol. 2009 Feb;181(2):452-61. doi: 10.1016/j.juro.2008.10.074. Epub 2008 Dec 13.
Marko Kaleva, Jorma Toppari. Cryptorchidism: an indicator of testicular dysgenesis? Cell Tissue Res. 2005 Oct;322(1):167-72. doi: 10.1007/s00441-005-1143-3.
Peter A Lee, Christopher P Houk. Cryptorchidism. Curr Opin Endocrinol Diabetes Obes. 2013 Jun;20(3):210-6.
FAQs from users: 'Can cryptorchidism cause azoospermia?', 'Is there a relationship between cryptorchidism and testicular cancer?', 'Does unilateral cryptorchidism also affect fertility?', 'Is prevention of cryptorchidism possible?', 'What types of cryptorchidism are there?' and 'Is cryptorchidism hereditary?'.
Authors and contributors

More information about Cristina Algarra Goosman







Hi, I was diagnosed with cryptorchidism on one side only, I imagine it to be unilateral after reading this article. I wonder, will I have any problem having children? I had surgery quite a few years ago
Hi Cody,
If after the diagnosis of unilateral cryptorchidism corrective surgery was performed there is a 25% chance of seminal disruption. If you are thinking of seeking pregnancy I recommend that you have a semen analysis to establish your semen quality.
I hope this has helped you.