When a couple does not manage to get pregnant after a year of unprotected sex, fertility treatment may be necessary to have a baby.
There are various human assisted reproduction techniques that can be classified into two groups:
- Low-complexity techniques
- timed intercourse, sperm capacitation, artificial insemination, sperm freezing, etc.
- High-complexity techniques
- in vitro fertilization, intracytoplasmic sperm injection, preimplantation genetic diagnosis, vitrification, etc.
Each of these techniques is composed of protocols and methods that may have different degrees of difficulty.
Provided below is an index with the 7 points we are going to expand on in this article.
- 1.
- 2.
- 2.1.
- 2.2.
- 3.
- 3.1.
- 3.2.
- 3.3.
- 3.4.
- 4.
- 4.1.
- 4.2.
- 4.3.
- 4.4.
- 4.5.
- 4.6.
- 4.7.
- 5.
- 6.
- 7.
Choosing the right technique
Fertility experts decide what type of technique is most appropriate for each patient depending on several factors such as the degree of infertility or age. It is also important to value the sum of the reproductive potential of both members of the couple: the man and the woman.
In addition, several combined techniques may be necessary to treat the sterility. For example, in vitro fertilization with preimplantation genetic diagnosis and/or embryo vitrification.
Low-complexity techniques
In an assisted reproduction clinic, fertility treatments with low-complexity techniques are defined as those that do not pose any risk or great discomfort to patients.
Methods without great technical difficulty for medical specialists or laboratory staff are also considered low-complexity methods.
Assisted procreation, as any other medical treatment, requires that you rely on the professionalism of the doctors and staff of the clinic you choose. Obviously, each clinic is different. Get now your Fertility Report, which will select several clinics for you out of the pool of clinics that meet our strict quality criteria. Moreover, it will offer you a comparison between the fees and conditions each clinic offers in order for you to make a well informed choice.
There are many techniques that meet these requirements in assisted reproduction. However, we will deal with the most relevant ones below.
Intrauterine inseminaton (IUI)
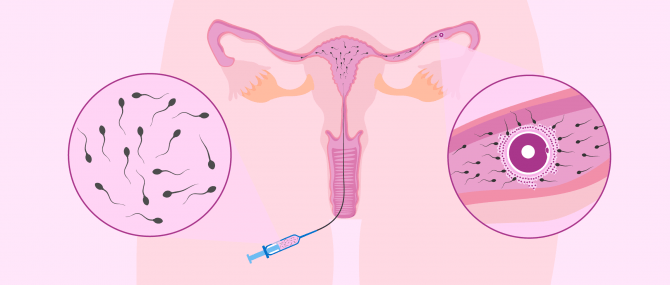
IUI, or artifical insemination (AI), is a very simple technique used to achieve a pregnancy and the first choice if the minimum age, Fallopian tube patency and seminal quality are met.
This reproductive option consists of depositing sperm in an artificial way in the woman's reproductive system. The most usual is to deposit sperm into in the uterus, although it is also possible to do intravaginal or intratubal AI.
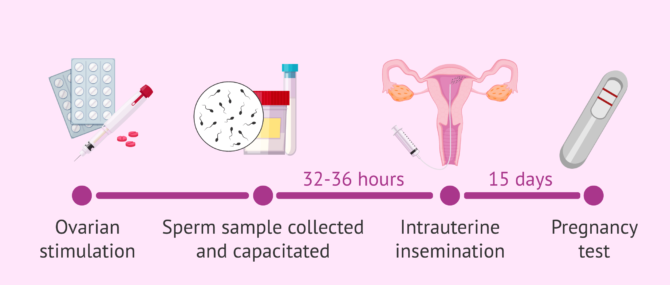
During the procedure, the woman's ovarian cycle is stimulated and ovulation is controlled. Then, when 1 -2 follicles are correctly developed, ovulation is induced and the insemination is programmed for 32 - 36 hours afterwards.
The sperm sample for insemination is collected by masturbation and capacitated in the laboratory. The sperm capacitation process consists of preparing a medium enriched with the best quality spermatozoa, which will then be introduced into the woman with an insemination cannula. The IUI technique is painless so does not require anesthesia.
If donor sperm is used, it will be frozen. Therefore, it is necessary to perform a semen thawing prior to the AI.
Approximately two weeks after the IUI, the woman will take a blood pregnancy test to see if the process has been successfully completed.
If you want to dive deeper into the topic of IUI, have a look at the following post: What is artificial insemination?
Fertility preservation
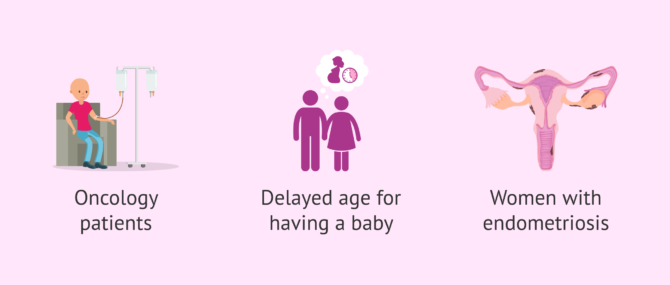
Fertility preservation is a technique that consists of freezing eggs and/or sperm. In this way, the cells can be kept undisturbed for an indefinite amount of time until you wish to have children.
It is a technique that is indicated in oncological patients, in women who wish to delay motherhood, or who suffer from endometriosis. Furthermore, men can also preserve their fertility to become parents in the future.
We recommend taking a look at the following article if you are interested in reading about this topic in more detail: What is fertility preservation?
Sperm freezing
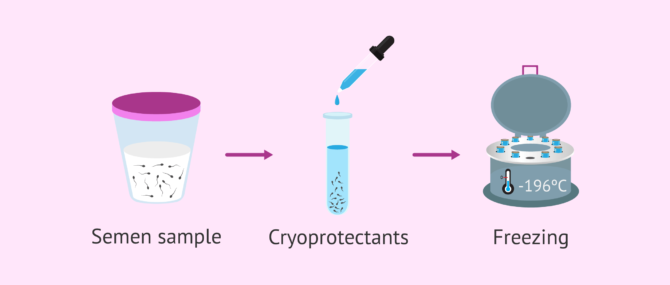
Sperm freezing is a quick and simple technique that also offer many advantages. For example, it allows the preservation of fertility in cancer patients who are about to undergo chemotherapy.
It has also allowed for the development of sperm donation, as donor sperm samples must be frozen for at least 6 months in order to confirm that they are HIV-free.
In particular, sperm cryopreservation is carried out by a slow freezing process. This requires mixing the sperm sample with cryoprotectants to prevent damage to the sperm. The temperature of the sample is then gradually lowered depending on the type of technique (vapours, dry ice, etc.) and finally introduced into liquid nitrogen at -196°C.
For more information on the type of techniques and how the process works, please visit the following post: Sperm freezing.
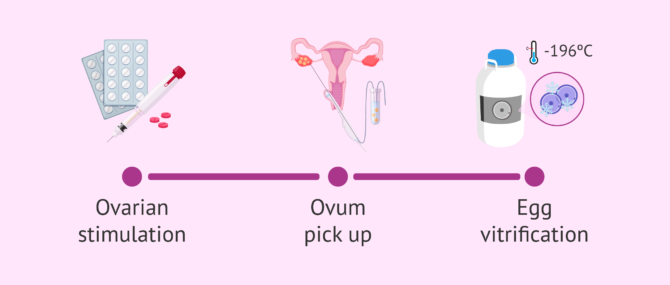
Egg vitrification
The preservation of fertility in women is carried out through the vitrification of eggs, i.e. by ultra-fast freezing of the eggs from 15ºC to -196ºC. In this way, the eggs are maintained without suffering physical or functional alterations for an unlimited period of time.
In contrast to slow freezing, vitrification does not generate ice crystals. As such the survival rate of the oocytes is greatly increased and allows motherhood to be delayed with high probabailities of success.
Patients who wish to vitrify their eggs need to administer hormonal medication in a controlled manner to make several eggs mature. Subsequently, the follicular puncture (ovum pick-up) is performed to obtain the eggs. These are then vitrified and stored in a liquid nitrgoen bank until their future use.
It should be kept in mind that age is a very important factor in fertility preservation. Dr. Sergio Rogel, a fertility expert and assisted reproduction specialist at the Alicante General Hospital in Spain tells us:
The best age for freezing eggs is the youngest possible age. Obviously, women should be over 18 but the younger the better.
We could define the best age for freezing eggs as between 20 and 30 years old.
For more information on egg vitrification we recommend reading this article: What is meant by egg vitrification and what are its advantages?.
High-complexity techniques
Highly complex techniques are performed with high-tech instruments and by more specialized personnel. Normally, they are done in the embryology laboratory and in the operating theatre, which must meet the conditions of maximum sterility.
These are more expensive treatments with higher risks. However, they offer higher success rates than low-complexity techniques.
Conventional in vitro fertilization (IVF)
IVF is a technique that consists of the extraction of the woman's eggs by puncturing the ovarian follicles and fertilizing them with the male's sperm in the laboratory. The embryos obtained are then transferred to the mother's uterus to achieve pregnancy.
This procedure consists of several steps, which are detailed below:
- Ovulation induction
- Hormonal medications to induce ovulation are administered, to control the menstrual cycle and trigger the maduration of various egg cells.
- Follicular puncture
- depending on the size of the follicles and the levels of estradiol in the blood, the hormone hCG is injected to trigger ovulation and the puncture for ovum pick-up is scheduled about 34-36 hours later. This is done under light sedation or local anesthesia.
- IVF
- in the laboratory the egg and sperm are incubated together for about 19 hours. After this time we can observe if fertilization has been achieved when two pronuclei appear.
- Embryo culture
- the embryos obtained are kept in culture and their development is observed through their cell divisions. Over 5 days, the embryos go through the zygote, 4 and 8 cell, morula and blastocyst stages.
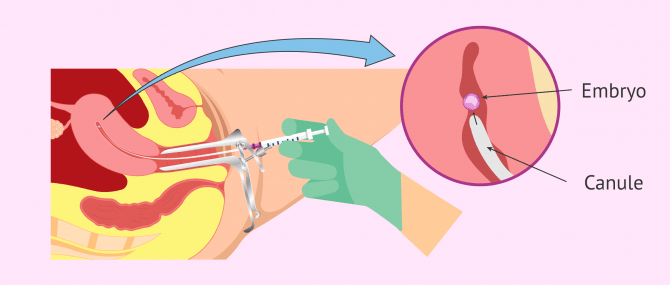
- Embryo transfer
- can be done after 3 or 5 days of development. The specialist introduces a cannula, previously loaded with the embryo, into the uterus.
Embryos that are not transferred to the woman can be cryopreserved through a process known as vitrification. This way, the woman will not have to go through the whole process of ovarian stimulation again if shes a second attempt or wants another child after a few years.
Intracytoplasmic Sperm Injection (ICSI)
ICSI is a variation of IVF with step in fertilizing the eggs being more complex.
The eggs are obtained in the same way as IVF: by ovum pick up. However, fertilization does not take place naturally. Instead, a sperm is selected under the microscope and inserted into the egg by means of a micro-needle. As such, this technique requires further intervention by specialist personnel.
The subsequent embryo development, quality assessment and embryo transfer are carried out in the same way as in conventional IVF.
The advantage of this technique is that it offers very good results in cases of poor male prognosis, that is, when the male's sperm are not able to fertilize the eggs by themselves because of their poor motility or morphology.
Embryo transfer
This is the final process of in vitro fertilization techniques, both in conventional IVF and ICSI. The aim is to transfer the best embryo(s) so that they can implant into the uterus and give rise to a pregnancy that will continue developing.
The transfer of the embryos into the uterus can be carried out on the third or fifth day of development. This is decided on the basis of the type of infertility the couple has, the number of fertilized eggs and the evolution of the embryos in previous IVF cycles.
The day chosen for the embryo transfer has some advantages and disadvantages depending on whether it is on the 3rd or 5th day. You can continue reading about this subject in this post: Embryo transfer on day 3 or day 5?
The patient may need to be prescribed progesterone after the ovum pick-up. This is to prepare the endometrium to improve endometrial receptivity and embryo implantation.
Once it has been decided whether one or two embryos will be transferred, the ones with the best quality are selected and placed in a very fine catheter that will be introduced into the uterus via the vagina.
The embryo transfer is a simple technique that takes a few minutes. It is completely painless, does not require any type of anesthesia and the patient leaves after about 20 minutes of rest on the bed.
From the moment of the transfer, the so-called two week wait period begins until the woman can take a pregnancy test after about 15 days.
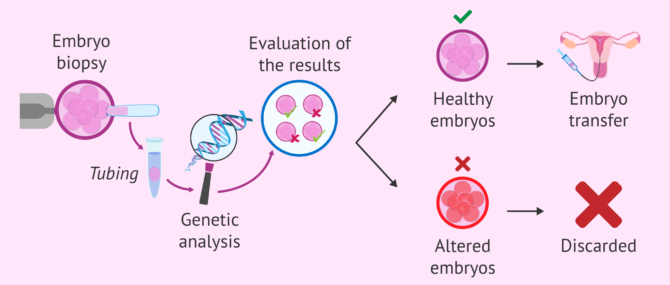
Preimplantation genetic diagnosis (PGD)
PGD is a complementary technique that can be performed after IVF or ICSI. However, it is not possible after IUI. Its purpose is to detect if any genetic abnormalities in the embryo exist.
In order to perform this test, a cell must be extracted from the embryo when it has about 8 cells. In this way, the viability of the embryo is not compromised.
Embryo biopsy does not produce any damage at this stage because the cells are totipotent. This means that they can give rise to any cell type in the human body until they form a complete organism.
Once the results of the analysis are received, the genetically healthy embryos are selected for transfer and the rest are discarded. Normally, the transfer of these embryos takes place on day 5 of development because we have to wait for the results.
Those embryos without chromosomal alterations that are not transferred can be vitrified for future use.
If you would like to continue reading about PGD then you can find more detailed information in our following post: What is preimplanation genetic diagnosis?
FAQs from users
What fertility treatments are recommended for single women?
Most single women who wish to become mothers and come to assisted reproduction centers have not tried natural reproduction, so it cannot be said that they have a sterility problem.
In these cases, the indicated reproductive technique would be artificial insemination with donor sperm (AID). However, if the results of some of the tests are altered, perhaps it would be best to resort to in vitro fertilization with donor sperm.
Read more
What is PGD used for?
Preimplantation Genetic Diagnosis (PGD) is a technique that complements IVF/ICSI and helps us detect the presence of genetic abnormalities in embryos before their transfer to the maternal uterus.
Currently, it is done by performing an biopsy to the trophoblast of a blastocyst embryo, that is, on days 5-6 of embryo culture. The cells removed can be examined to detect the presence of chromosomal abnormalities using PGS (Preimplantation Genetic Diagnosis), or genetic diseases, such as Duchenne muscular dystrophy (DMD).
Which fertility treatment is right for having twins?
The fact that the probability of twin pregnancy increases after fertility treatment is due to the transfer of two embryos instead of one. This happens with conventional in vitro fertilization or ICSI, when a greater number of embryos are obtained after stimulation.
What are the pros and cons of assisted reproductive technology (ART)?
Obviously, the main advantage of ART is that it gives you the chance to have a baby. On the other hand, the most common disadvantage is associated with fertility drugs, due to the side effects they can cause: headache, bloating, nausea, vaginal bleeding/spotting...
However, fertility drugs are commonly the first choice because of their relative convenience, especially for IVF.
Secondly, reproductive surgery, required to correct anatomical abnormalities or clear blockages in the man or the woman, are usually invasive, which increases their risk, recovery time and cost. On the other hand, they help increase the chances of getting pregnant.
Perhaps the main disadvantage of all infertility treatments is related to the financing options, since they are not always covered by insurance. Also, in the case of IVF, the likelihood of having twins is higher if multiple embryo transfers are chosen.
What types of fertility treatments for males exist?
When a man is diagnosed with some kind of fertility issue after a semen analysis, the doctor may prescribe vitamin supplements or a special diet to be followed before turning to infertility treatments.
While trying to boost sperm quality through natural remedies, avoiding the consumption of saturated fats is of utmost importance. In case there exist one or various seminal alterations (low sperm count, low sperm motility...), multivitamin supplements is recommended.
In the case that it is caused by an infection (presence of leukocytes in the semen sample), antibiotics may be prescribed as well. If it does not work or is a case of non-obstructive azoospermia, maybe you should consider IVF/ICSI.
To learn more about this topic, do not miss this post: Foods to boost sperm quality.
Can fertility treatments be done at home?
No, fertility treatments are carried out at a fertility clinic or medical facility. In the case of AI, it can be done at the gynecologist's office, due to the simplicity of the technique. Conversely, special equipment is required for all of the IVF steps involved to be carried out properly.
There is, however, an alternative to artificial insemination which is known as at-home artificial insemination. It is mainly a do-it-yourself version of AI in which the woman can get herself inseminated with donor or partner sperm by just buying an insemination kit at the pharmacy.
It should be taken into account that its chances of success are exactly the same as those you would achieve through natural conception. Besides, it involves a series of health risks, as the equipment has not been previously sterilized and therefore the risk of introducing germs into the vaginal tract is higher.
Are there consequences of assisted reproduction techniques?
One of the possible consequences of assisted reproduction is the possibility of having a multiple pregnancy. However, this is becoming less and less common since fertility treatments are perfectly controlled and the transfer of a single embryo is usually chosen to avoid a multiple pregnancy.
Another possible consequence of assisted reproduction, especially IVF, is the development of ovarian hyperstimulation syndrome. This means that the ovaries respond in an exaggerated manner to the hormonal medication administered during the stimulation phase.
Recommended reading
One of the most discussed issues in a laboratory when doing an IVF treatment is the number of embryos to be transferred. If you are interested in this topic, you can read more here: How many embryos should be transferred?
If you're thinking about getting fertility treatment, you can find out what the prices are for these techniques in the next article: Costs in assisted reproduction.
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
Edwards, RS (1995). Principles and practice of Assisted Human Reproduction. Brody SA eds. Philadelphia: W.B. Saunders Co.
Grupo de Interés de Centros de Reproducción Humana Asistida del Sistema Nacional de Salud (2002). Criterios para la utilización de los recursos del Sistema Nacional de Salud Español en técnicas de reproducción humana asistida Rev Iberoam Fertil; 19(1): 5-31.
Ley 14/2006, de 26 de mayo, sobre técnicas de reproducción humana asistida. Jefatura del Estado «BOE» núm. 126, de 27 de mayo de 2006 Referencia: BOE-A-2006-9292 (View)
Matorras R. (2002). La reproducción asistida en el sistema sanitario público español. Rev Iberoam Fertil; 19 (2): 103-108.
Matorras R, Hernández J (eds) (2007). Estudio y tratamiento de la pareja estéril: Recomendaciones de la Sociedad Española de Fertilidad, con la colaboración de la Asociación Española para el Estudio de la Biología de la Reproducción, de la Asociación Española de Andrología y de la Sociedad Española de Contracepción. Adalia, Madrid.
National Callaborating Center for Women’s and Children’s Health. Fertility: assessment and treatment for people with fertility problems. Clinical Guideline February 2004. Recuperado el 22 de agosto de 2018 de http://www.rcog.org.uk (View)
Pellicer A, Alberto Bethencourt JC, Barri P, Boada M, Bosch E, Hernández E, Matorras R, Navarro J, Peramo B, Remohí J, Riciarelli E, Ruiz A y Veiga A (2000). Reproducción Asistida. En: Documentos de Consenso SEGO; 9-51.
Santamaría Solís, L. (2000). Técnicas de reproducción asistida. Aspectos bioéticos. En: Cuadernos de Bioética/1ª. Asociación Española de Bioética y Ética Médica (AEBI) (View)
Schmidt L, Münster K. Infertility, involuntary infecundity, and the seeking of medical advice in industrialized countries 1970-1992 (1995): a review of concepts, measurements and results. Hum Reprod; 10: 1407-18 (View)
Sociedad Española de Fertilidad (SEF) (febrero de 2012). Saber más sobre fertilidad y reproducción asistida. En colaboración con el Ministerio de Sanidad, Política Social e Igualdad del Gobierno de España y el Plan de Calidad para el Sistema Nacional de Salud.
The ESHRE Capri Workshop Group. Intrauterine insemination. Human Reproduction Update, 2009; 15 (3): 265–277.64 (View)
Vayena E, Rowe PJ, Griffin PD, (eds.) (2002). Current Practices and Controversies in Assisted Reproduction. Report of a meeting on "Medical, Ethical and Social Aspects of Assisted Reproduction", World Health Organization, Geneva.
Zegers-Hochschild F, Adamson GD, de Mouzon J, Ishihara O, Mansour R, Nygren K, Sullivan E, Vanderpoel S, for ICMART and WHO. Glosario de terminología en Técnicas de Reproducción Asistida (TRA). Versión revisada y preparada por el International Committee for Monitoring Assisted Reproductive Technology (ICMART) y la Organización Mundial de la Salud (OMS). Red Latinoamericana de Reproducción Asistida en 2010 Organización Mundial de la Salud 2010 (View)
FAQs from users: 'What fertility treatments are recommended for single women?', 'What is PGD used for?', 'Which fertility treatment is right for having twins?', 'When is it time to see a fertility specialist?', 'What are the pros and cons of assisted reproductive technology (ART)?', 'How long after fertility treatment can you adopt?', 'What are the long-term side effects of fertility treatments?', 'What types of fertility treatments for males exist?', 'Can fertility treatments be done at home?' and 'Are there consequences of assisted reproduction techniques?'.
Authors and contributors

More information about Michelle Lorraine Embleton









Hi. I have had 3 rounds of insemination and failed to get pregnant. We are considering IVF, but not sure if it available on the NHS? We live in Bristol. Thanks
Hi VictoriaMac
According to the National Institute for Health and Care Excellence (NICE) fertility guidlines, for women under 40, they can be offered 3 cycles of IVF if they have been unable to get pregnant through regular unprotected sex for 2 years and unable to get pregnant after 12 cycles of artificial insemination, with at least 6 of the cycles using a method called intrauterine insemination (IUI).
Women aged 40-42 would only be eligible for 1 cycle of IVF.
For more details on the criteria in your particular area you can consult the NHS wesbite.
I hope this information helps and all the best in TTC.
Great post. It’s a fact that your blog posts are so unique and interesting. I have always admired your site. Thanks for the great tips and work
Best Fertility Centre
Test tube baby treatment in Hydetrabad
Hello! My name is Lorena and I’m 31 years old, I want to be a single mother, I don’t have a boyfriend or a partner, can I get inseminated to get pregnant? My dream is to be a mother even if I’m alone without a partner. Could you tell me everything I need to do? Thank you
I’m 29 years old and I don’t have a baby. I would like to know how I know if I am fertile and if I can conceive, since I am interested in having a baby. Please, I would like to know if everything is okay with my health. Thank you.
Hi!
After repeated miscarriages and misconduct on behalf of our fertility clinic, I’m looking into safe options. Which clinic can you recommend me in regards to transparency? I’d also love to get information about success rates.
Hi Clara,
I’m very sorry to hear this. Transparency in both procedure and success rates is key when it comes to a successful fertility clinic.
This is why we have implemented a set of rigorous criteria which a clinic must fulfil in order to be recommended by us. This fertility report will list you all clinics that have been analyzed by our invitRA team and that adapt to your needs.
Hope this helps,
Wish you the best!
Hello, wondering if anybody has experienced more or less the same as I do… I started an IVF treatment using my own eggs two years ago and it was unsuccessful, so I’m considering starting a repeated IVF cycle by using donor eggs, but I wonder if maybe there is some country where success rates of IVF with donor eggs are higher, does anyone have the slightest idea? Thanks!!