One of the most controversial issues of In Vitro Fertilization (IVF) procedures is the question concerning the number of embryos to transfer. This decision should be made bearing in mind the chances of success, but at the same time aiming to reduce the risk of multiple birth.
Currently, there seems to be a consensus between experts in the field: the general recommendation is one embryo per transfer, both in fresh and frozen cycles, irrespective of whether own or donated eggs are used.
Thanks to advances in the field of assisted reproduction, embryo selection in the laboratory is much more precise. Therefore, it is preferable to transfer a single embryo of good quality.
For this reason, the first embryos to be transferred will be those of A quality, while the last embryos to be transferred will be those classified as D quality.
Provided below is an index with the 7 points we are going to expand on in this article.
- 1.
- 1.1.
- 1.2.
- 1.3.
- 2.
- 3.
- 4.
- 4.1.
- 4.2.
- 4.3.
- 4.4.
- 4.5.
- 4.6.
- 4.7.
- 4.8.
- 5.
- 6.
- 7.
How to decide how many embryos to transfer
Multiple embryo transfers are directly linked to higher chances of getting pregnant, but also of multiple pregnancy (twins or triplets). There are risks of this type of multiple pregnancy for both the mother and the babies.
Embryologist Aitziber Domingo explains that they never transfer more than one or two embryos per patient. She agrees with this topic being one of the most controversial ones in the field of Assisted Reproduction. However, determining if 1 or 2 embryos should be transferred depends on the peculiarities of each couple.
Depending on the patient, particularly factors like age and embryo quality, we can make the right decision. Nowadays, the trend is to transfer a single embryo, something favored by the embryo vitrification technique to a large extent. Almost 90% of embryos survive this technique. By doing this, we reduce the chance of multiple pregnancy, as the embryos are transferred one by one.
Advances in reproductive technologies
A few years ago, the most common practice was to transfer two or even three embryos per cycle. But presently, the outcomes of fertility treatments have increased so much that specialists almost never transfer three embryos in a single cycle. Instead, transferring a single embryo is increasingly becoming the most common practice.
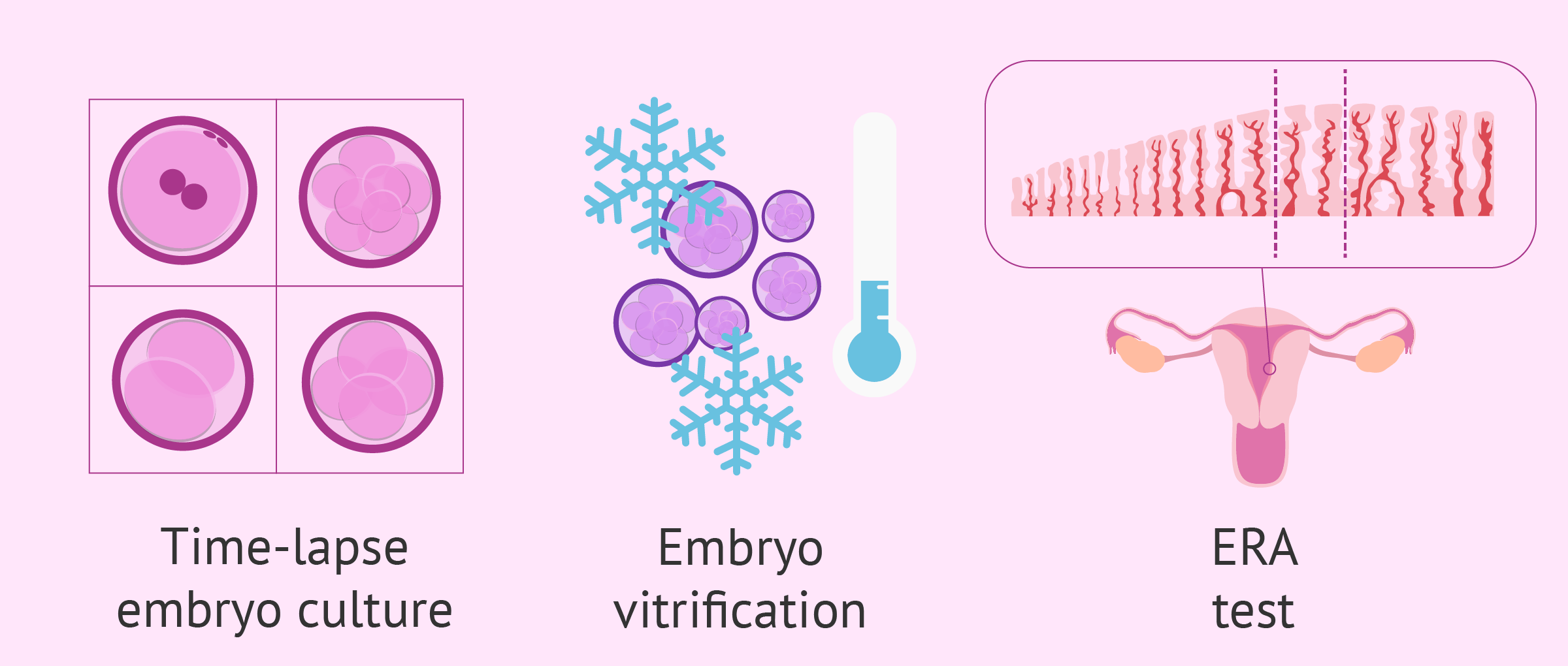
This change is due to the improvements achieved in this field, including:
- Optimization of embryo culture systems
- Time-lapse monitoring systems
- Optimization of embryo vitrification technique (embryo freezing)
- Endometrial Receptivity Array (ERA) Test
These advancements have enable the availability of a higher amount of good quality embryos to choose from, which allows the embryologist to select the best ones with more accuracy. Also, it allows us to predict the moment of optimal endometrial receptivity, and to schedule the embryo transfer for that day in order to maximize the chances of success.
Criteria used to make a decision
When making the decision of how many embryos to transfer, the following aspects should be taken into consideration:
- Embryo quality
- Stage of embryo development (day 2, day 3 or blastocyst)
- Maternal age
- Previous cycle failure (implantation failure, recurrent miscarriage, etc.)
- Cause of infertility
- Endometrial receptivity
- Uterine anomalies
- Own or donated eggs
- Egg quality
The number of embryos to transfer will be determined considering all the factors listed above, especially embryo quality to determine the implantation potential. The decision should be made on a case-by-case basis, always with the ultimate goal of achieving a singleton pregnancy.
For example, imagine a young patient with three class A embryos (optimal quality) available, without previous IVF failure. The embryologist will recommend that she opts for a single embryo transfer, as she has a good prognosis, that is, the chances for embryo implantation to occur are high.
Conversely, if we consider the case of a patient who is over the age of 35, with embryos of class B and C quality (medium to poor quality) and previous failed IVF cycles, she may require a two-embryo transfer, as the chances for both embryos to attach to the uterus are lower.
If you need to undergo IVF to become a mother, we recommend that you generate your Fertility Report now. In 3 simple steps, it will show you a list of clinics that fit your preferences and meet our strict quality criteria. Moreover, you will receive a report via email with useful tips to visit a fertility clinic for the first time.
You can find more information about embryo quality in this article: Embryo Classification According to Their Quality.
Guidelines given in the USA, UK and Spain
In most countries, the regulatory bodies establish guidelines for the number of embryos to be transferred in IVF.
American Society for Reproductive Medicine (ASRM) guidelines for number of embryos that should be transferred depends on if they are on day 3 or day 5. However, they recommend single embryo trasnsfer in younger women, rising to 2 or even possibly 3 as the maternal age increases and favorable prognosis decreases.
The HFEA, Human Fertilisation and Embryology Authority in the UK, recommends that in the case of good quality embryos, only one is transferred. This is called elective single embryo transfer or eSET. Two or more may be advisable in cases of advancing maternal age.
The Spanish Fertility Society, SEF guidelines are along the same lines. They favour a single embryo transfer for quality embryos and younger women, with two embryos in older women. Three embryos are only recommended if the quality is poor and the mother is older.
Risk of multiple pregnancy
For couples who have been trying to conceive for a long time, the desire to have a baby is so strong that sometimes they find shelter in the fact that chances of getting pregnant increase if more than a single embryo is transferred. The problem is, most of them do not take into account the risk of multiple births it entails.
However, when it comes to making the decsion on how many embryos to transfer, the risks associated with multiple births should be considered.
The likelihood of preterm birth (before week 37) is higher in these type of pregnancies and, sometimes, they can even lead to extreme preterm birth (before week 26 of pregnancy). Additionaly, multiple pregnancies are associated with a higher chance of premature rupture of membranes (PROM), gestational diabetes, hypertension, and other problems associated with pregnancy, such as anemia.
Finally, the likelihood of requiring a C-section is higher, as is the risk of miscarriage.
Find more information about this topic in the following article: What Are the Risks of Multiple Births?
Single Embryo Transfer (SET)
For all the reasons explained above, assisted reproduction specialists have reached a consensus whereby a SET is the option of choice as long as it is possible.
By doing this, we increase the chances of success per transfer, due to elevated embryo quality, thereby preventing the risk of multiple birth.
In addition, if the transfer of this single embryo is at day 5 of development or at the blastocyst stage, the probability of pregnancy will be much higher.
FAQs from users
Does the probability of pregnancy increase with the number of transfers?
No, pregnancy rates do not increase with the number of embryo transfers. In general, pregnancy rates per transfer in IVF/ICSI cycles are 60% (depending on the age of the patient) with a cumulative pregnancy rate of 90% on the fourth attempt. This does not mean that in the fourth attempt there is a 90% pregnancy rate, but rather that, of all the patients/couples that do IVF/ICSI cycles, 90% of them achieve pregnancy in the fourth attempt, considering that, per attempt, it is 60%.
Similarly, in cycles with donated eggs, pregnancy rates can be 70% with a cumulative pregnancy rate of 99% in a fourth attempt.
It is important to note that, if after a second transfer of good quality embryos pregnancy is not achieved, we must perform a study to determine the cause of the failure (Implantation Failure, etc).
Do you follow the same procedure with fresh and frozen embryos?
The treatment to follow varies depending on whether it is a fresh embryo transfer (after an IVF cycle) or a frozen embryo transfer.
With fresh embryos, patients follow a hormonal treatment based on applying injections to stimulate the ovaries during 10 days approximately. After retrieving the eggs, the patient starts taking progesterone vaginally or subcutaneosly.
With frozen embryos, patients have to prepare during 2 weeks with estrogens (in patches or tablets). Depending on the day of the embryo transfer, progesterone may be prescribed as well. In some cases, the patient follows a natural cycle, without using estrogens.
Does the number of embryos transferred have an influence on the endometrial preparation process?
The endometrium can be stimulated either naturally, by the woman’s ovarian estradiol, or artificially, by applying estradiol usually in the form of tablets or transdermal patches to obtain adequate endometrial lining thickness by ultrasound measurement.
Unless a woman ovulates, the hormone progesterone is administered by the woman vaginally or by intramuscular injection to achieve optimal endometrial preparation for embryo implantation. Alternatively, following natural ovulation, the woman’s ovaries produce progesterone to accomplish this same purpose toward embryo transfer. Either natural or artificial method occurs without regard to the number of embryos planned for transfer.
How can multiple pregnancy from assisted reproductive technology be prevented?
There are lots of actions to be taken, most of them being implemented with increasing success.
As for in vitro fertilisation, a three-embryo transfer should be avoided: cases with a good prognosis should bet on a single embryo transfer instead. This requires a process of raising awareness not only by the couple undergoing the treatment but also by the professional team.
The “success” of an assisted reproductive treatment does not consist only on achieving pregnancy. More and more, we need to be aware that the ultimate aim should be having a healthy baby, that is to say, that the child is not born too early.
Even though changing this mindset may be difficult, we insist on the need of it to prevent multiple births.
Some patients think that transferring multiple embryos increases the chances for success. Are they right?
Yes, technically they are right. By transferring two embryos instead of a single embryo, the chances for pregnancy are greater. The importance of a good embryo freezing programme is that it allows the chances to be the same if we compare performing a two-embryo transfer at the same time with performing a two-embryo transfer in two different cycles, one of them after being frozen. The concept is “1 + 1 = 2″.
Should the quality of the gametes be taken into account when choosing how many embryos to transfer?
Yes, when a fertility treatment is performed using poor quality gametes, it is more likely, for example, that there will be chromosomal alterations that will limit the chances of success of the treatment, as well as the implantation of the embryo in the uterus.
On the other hand, if, for example, donor eggs are used, they are usually of high quality because they come from young women. Therefore, there will be a greater probability that the resulting embryo will be of better quality and will implant in the uterus, resulting in an evolutionary pregnancy.
Does the day of embryo transfer influence how many embryos to transfer?
Yes, since blastocysts (day 5-6 after fertilization) are more likely to attach to the uterine lining, as they are synchronized with the uterine lining and allows for a more accurate selection process. Thus, if we transfer two class A blastocysts, they will have higher chances of implanting than two class A embryos on day 3.
Read more: Day 5 vs. Day 3 Embryo Transfer – What Are the Pros & Cons?
Is it possible to predict which embryos will implant and which don't?
In spite of the progress made in reproductive technologies already explained, we still cannot predict with 100% accuracy which embryo will be able to implant.
However, it is possible to predict which one will have higher chances of implanting. Implantation is a complex process where the endometrial lining plays a major role. In this sense, the relationship between endometrial thickness and embryo implantation is crucial.
Check out this for information: What Is Embryo Implantation? – Process & Stages.
Recommended reading
Throughout this post, we have made several references to the technique of embryo transfer. If you would like to read more about this then please visit the following link: Embryo transfer: when and how?
What happens to the embryos that are not transferred? To find out we recommend reading this article: What is the fate of unused embryos.
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
Forman EJ, Hong KH, Ferry KM, Tao X, Taylor D, Levy B, et al. In vitro fertilization with single euploid blastocyst transfer: a randomized controlled trial. Fertil Steril 2013;100:100–7.e1 (View)
McLernon DJ, Harrild K, Bergh C, Davies MJ, de Neubourg D, Dumoulin JC, Gerris J, Kremer JA, Martikainen H, Mol BW, Norman RJ, Thurin-Kjellberg A, Tiitinen A, van Montfoort AP, van Peperstraten AM, Van Royen E, Bhattacharya S: Clinical effectiveness of elective single versus double embryo transfer: meta-analysis of individual patient data from randomized trials. BMJ 2010, 341:6945 (View)
Montag M, Toth B, Strowitzki T. (2013). New approaches to embryo selection. Reprod Biomed Online;27:539–46 (View)
Pandian Z, Marjoribanks J, Ozturk O, Serour G, Bhattacharya S: Number of embryos for transfer following in vitro fertilisation or intra-cytoplasmic sperm injection. Cochrane Database Syst Rev 2013, 7:CD003416 (View)
Practice Committee of American Society for Reproductive Medicine; Practice Committee of Society for Assisted Reproductive Technology: Criteria for number of embryos to transfer: a committee opinion. Fertil Steril 2013, 99:44–46 (View)
Practice Committee of the Society for Assisted Reproductive Technology and Practice Committee of the American Society for Reproductive Medicine: Elective single-embryo transfer. Fertil Steril 2012, 97:835–842 (View)
Tomás C, Tikkinen K, Tuomivaara L, Tapanainen JS, Martikainen H. (2002). The degree of difficulty of embryo transfer is an independent factor for predicting pregnancy. Hum Reprod; 17:2632–5 (View)
Vilska S, Tiitinen A, Hyden-Granskog C, Hovatta O. Elective transfer of one embryo results in an acceptable pregnancy rate and eliminates the risk of multiple births. Hum Reprod 1999;14:2392– 2395 (View)
William B. Schoolcraft, M.D., for the ASRM American Society for Reproductive Medicine (April 2016). Importance of embryo transfer technique in maximizing assisted reproductive outcomes. Vol. 105, No. 4. Colorado Center for Reproductive Medicine, Lone Tree, Colorado (View)
FAQs from users: 'Does the probability of pregnancy increase with the number of transfers?', 'Do you follow the same procedure with fresh and frozen embryos?', 'Does the number of embryos transferred have an influence on the endometrial preparation process?', 'How can multiple pregnancy from assisted reproductive technology be prevented?', 'Some patients think that transferring multiple embryos increases the chances for success. Are they right?', 'In the United States, for instance, there is no limit regarding the number of embryos to transfer. Where do you stand on this?', 'How do we decide on number of embryos to transfer in IVF?', 'Should the quality of the gametes be taken into account when choosing how many embryos to transfer?', 'Why do we want reduce the possibility of multiple pregnancy in IVF?', 'Does the day of embryo transfer influence how many embryos to transfer?', 'What is meant by Single Embryo Transfer (SET)?', 'Is it possible to predict which embryos will implant and which don't?', 'In embryo transfer, is it the same process for fresh and frozen embryos?' and 'Is it possible to predict which embryos will implant into the uterus?'.
Authors and contributors

More information about Michelle Lorraine Embleton















Hi, I had two embryos transferred on the 23rd. I have been getting pain in the stomach on and off since then. But suddenly after two days the pain stopped completely. I am really worried, is everything ok inside???
Hello Binny,
the pain you felt in the stomach is a common symptom post embryo transfer. Given that you had it transferred on March, 23rd, it is likely to be due to ovulation induction drugs. Don’t panic, because it is a common symptom and does not indicate the transfer has been unsuccessful at all. Be patient during the 2WW. Hoping for the best!
Regards