Gestational diabetes is a mild type of diabetes that develops in some women during late pregnancy.
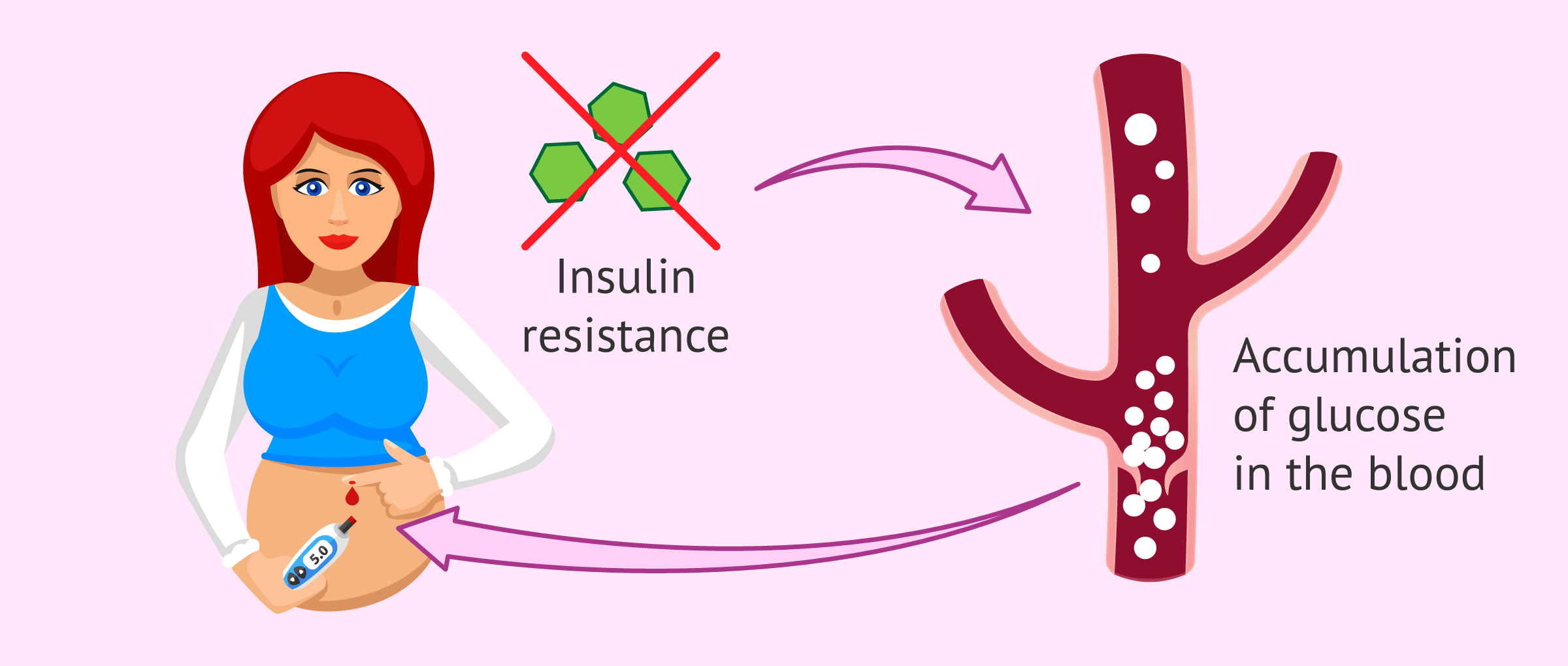
Unlike the other types of diabetes, gestational diabetes is not caused by a lack of insulin, but by the blockage of its functioning due to the hormones generated during pregnancy.
About 10% of pregnant women develop gestational diabetes, although most of them have no symptoms. This is why it is necessary to perform glucose controls in order to detect it.
Provided below is an index with the 9 points we are going to expand on in this article.
- 1.
- 2.
- 2.1.
- 3.
- 4.
- 5.
- 6.
- 6.1.
- 6.2.
- 6.3.
- 6.4.
- 6.5.
- 7.
- 8.
- 9.
Diabetes in pregnancy
Diabetes is a pathology characterized by abnormally high blood sugar levels. There are two main types of diabetes:
- Type I diabetes mellitus
- is due to insulin deficiency because the pancreas does not produce insulin and is usually caused by autoimmune factors.
- Type II diabetes mellitus
- is characterized by insulin resistance. The body's cells are not able to respond to insulin in order to utilize glucose and glucose accumulates in the bloodstream.
Gestational diabetes is included in type II diabetes mellitus and usually appears between 24-28 weeks of pregnancy. It occurs due to a blockage of the hormone insulin by pregnancy hormones and, as a consequence, blood glucose levels increase.
In most cases, glucose levels return to normal after delivery, with a prevalence of 1 to 3%.
However, women who have had diabetes during their first pregnancy are more likely to have it recur during a second pregnancy.
Causes
The rapid growth of the fetus during the third trimester of pregnancy requires large amounts of glucose, which it obtains from the mother.
To promote this glucose supply, hormones produced by the placenta block the action of insulin produced by the mother and increase the level of sugar available to the fetus.
The body's normal response to this situation of insulin resistance is for the woman's pancreas to produce more insulin during pregnancy. However, the body may not react and gestational diabetes may develop.
When insulin fails to perform its function, glucose is not converted into energy and accumulates in the blood to very high levels, known as hyperglycemia hyperglycemia.
Risk Factors
Some situations related to the woman before and/or during pregnancy may increase the risk of suffering gestational diabetes. These are discussed below:
- Pregnancy in women over 30-35 years old.
- Ethnic groups at higher risk: Hispanic American, African American, Native American, Southeast Asian or Pacific Islander.
- Family history of diabetes.
- Previous delivery of a baby weighing more than 4 kg (macrosoma) or with genetic alterations.
- Arterial hypertension.
- Polyhydramnios: excess amniotic fluid.
- Having had a miscarriage or intrauterine fetal death without apparent cause.
- Overweight before pregnancy.
- Excessive weight gain during gestation.
- Having polycystic ovarian syndrome (PCOS).
Women who present any of these risk factors will have to follow a balanced diet and control their weight to prevent the onset of gestational diabetes.
Diagnosis
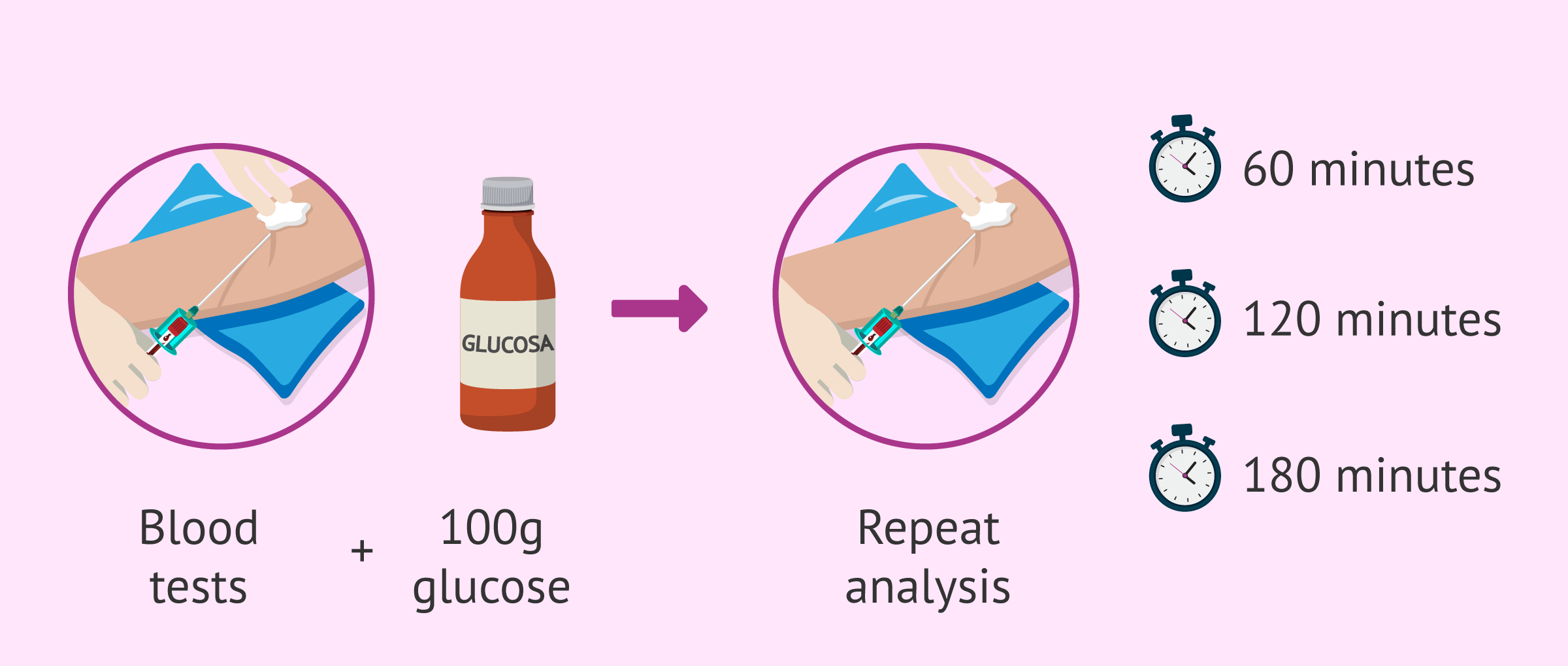
The test performed on pregnant women to determine whether they have gestational diabetes is called the O'Sullivan test o'Sullivan test. It is usually done from the 24th week of pregnancy, but if the woman has a history or risk factors it can be done as early as the first trimester.
This test consists of a fasting blood test to determine blood glucose levels. The woman should then take 50 grams of glucose and repeat the test after one hour.
If the woman obtains altered results (more than 95 mg/dl fasting and more than 140 mg/dl after ingesting sugar), it is indicative of gestational diabetes and the O'Sullivan test will have to be repeated in a more complete manner.
This new test is the glucose overload test and blood glucose determinations will be made on an empty stomach, at 60, 120 and 180 minutes after having taken 100 grams of glucose.
Depending on the results obtained and the altered values in each blood draw, the specialist will prescribe the most appropriate treatment.
Symptoms and consequences in the baby
In most cases, women do not notice that they have gestational diabetes and only find out after diagnostic tests. However, some of the following discomforts may occur:
- Blurred vision
- Fatigue
- Very thirsty
- Frequent urination
- Nausea and vomiting
- Weight loss
- Urinary tract infections and vaginal candidiasis
On the other hand, since gestational diabetes occurs mainly in late pregnancy when the baby is already formed, it need not lead to serious consequences if properly controlled.
However, lack of diabetes control can still carry certain risks for both mother and baby:
- Risks for the mother
- placental abruption, preterm delivery, preeclampsia, cesarean delivery, and increased incidence of diabetes mellitus in the years following pregnancy.
- Risks to the baby
- glucose from the mother's blood can pass through the placenta to the baby, convert to fat and generate macrosomia, i.e. a high birth weight baby. After delivery, the baby may suffer hypoglycemic crises, shortness of breath, and jaundice. There is also a greater tendency to suffer from diabetes and obesity in adulthood.
All these complications can be avoided if diabetes is diagnosed early and the woman follows all medical indications.
Diet and treatment
In mild cases of gestational diabetes, when only one or two of the sugar curve values are altered, it will be sufficient to follow a specific diet to control sugar levels.
Below, we are going to detail some recommendations on nutrition during pregnancy in women with gestational diabetes:
- It is necessary to spread meals throughout the day and avoid fasting. In general, eat about 6 meals with an interval of approximately 3 hours. In the evening, try not to allow more than 8 hours between dinner and breakfast.
- Consume foods rich in fiber: vegetables, fruits, whole grains and legumes. All in the recommended amounts.
- Avoid pastries and foods with a high glycemic index, such as soft drinks, honey, chocolate, sweets, etc.
- Do not consume saccharin. The sweeteners allowed in pregnancy are aspartame and acesulfame K.
- Decrease salt consumption.
- Control the amounts of carbohydrate-containing foods.
- Avoid fried foods, battered foods, etc. It is preferable to steam, bake or grill.
In general, the aim of the diet is for the woman to maintain balanced blood glucose levels throughout the day.
It is also important that the woman receives the necessary calorie intake, which should be between 30-40 kcal per kg of weight per day, in order to gain the necessary weight during pregnancy.
In addition, moderate exercise can help process glucose and maintain proper glucose levels. Daily walking is highly recommended for women with gestational diabetes unless otherwise indicated by the physician.
To monitor blood glucose levels regularly, a woman will need to purchase a blood glucose meter.
If elevated glucose values are detected for 1 to 2 weeks, insulintreatment will have to be applied.
Finally, it is advisable to perform monthly ultrasounds from the 28th week of pregnancy in order to detect the appearance and evolution of fetal macrosomia.
FAQs from users
Is the O'Sullivan test performed on all pregnant women?
Yes, it should be performed on all pregnant women between 24-28 weeks of gestation.
This test is an analytical test, which is a screening test for gestational diabetes mellitus. It evaluates carbohydrate metabolism by testing blood glucose.
What is the best treatment for gestational diabetes?
Gestational diabetes is a common endocrine pathology in pregnancy that develops due to an increase in placental hormones that can block the action of insulin resulting in a metabolic state of insulin resistance that will lead to an increase in blood glucose levels. Therefore, the treatment of gestational diabetes is focused on maintaining normal blood glucose levels, which is determined by blood glucose testing before and after meals.
Treatment must be individualized according to the characteristics of each patient. In most cases, blood glucose levels can be controlled with moderate physical exercise and a specific diet with a menu focused on avoiding sudden increases in blood glucose levels. Likewise, in overweight and obese patients, exercise and a healthy diet will improve the metabolic environment, reducing the risk of suffering this pathology.
Finally, in cases where blood glucose levels cannot be controlled with diet and exercise, the patient will be evaluated by an endocrinology team to begin treatment with injectable insulin, regulating the dose and type of insulin necessary to avoid episodes of hyperglycemia.
What care should be followed in pregnancy with gestational diabetes?
Gestational diabetes can be controlled by diet and exercise. The most advisable thing to do is to visit a specialized nutritionist for a proper diet.
Moderate exercise is also highly recommended to maintain adequate blood sugar levels. For example, going for a 30-minute walk or swimming every day.
What complications can arise in childbirth with gestational diabetes?
The main risk when giving birth in women with gestational diabetes is that the baby will have macrosomia (larger than normal size).
These babies can suffer injuries and trauma during vaginal delivery, such as shoulder dystocia. Therefore, a cesarean section may be necessary for the mother.
Can I still have diabetes after delivery?
In most women, diabetes disappears after giving birth, although they will have a higher risk of developing type II diabetes mellitus later in life or in a second pregnancy.
To reduce the risk of diabetes after childbirth, women are advised to breastfeed their babies to lose weight more easily, to follow a healthy and balanced diet, and to have all the glucose controls indicated by the doctor.
Recommended readings
As we have said, the most important thing to prevent gestational diabetes is for the woman to take care of her health and maintain good eating habits throughout her pregnancy. If you are interested in reading more about this, you can access the following post: Health in pregnancy.
If you want to know more tests that are performed throughout the pregnancy, as well as all the follow-up during the 40 weeks of gestation, you can continue reading here: Prenatal pregnancy control.
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
FAQs from users: 'Is the O'Sullivan test performed on all pregnant women?', 'What is the best treatment for gestational diabetes?', 'What care should be followed in pregnancy with gestational diabetes?', 'What complications can arise in childbirth with gestational diabetes?' and 'Can I still have diabetes after delivery?'.
Authors and contributors

More information about Cristina Algarra Goosman



Your work speaks volumes, a much-needed effort towards internet blogging. Commendable.
Hello, I have a family history of diabetes and I knew I had all the chances of having gestational diabetes but I didn’t know it would be so difficult. My doctor told me to follow a diet, is there anything else I can do? Thank you
Hi Callie,
Pregnant women with gestational diabetes should try to keep glucose values within normal parameters. To do this, the most recommended is to follow a diet low in sugars and carbohydrates which will facilitate the levels are maintained. Moderate physical exercise can also help to reduce them.
In any case, if the levels are not lowered for a couple of weeks, a pharmacological treatment should be taken to lower them, since high values can have a negative effect on both the mother and the baby.
I hope everything is going well!
Hi, I had the Osullivan test last week, my level was 90 on arrival and 200 after taking the liquid. I have been told that I have to do another one, they have not told me anything else but I am scared.
Hi Cece,
Your basal level is within normal values but the value after the test is a bit elevated as the ideal value after one hour of taking the shot is less than 190.
To determine if there is a problem or if it was a punctual elevated value, they will perform a second test in which they will observe how the sugar curve changes over 3 hours by obtaining a blood sample in the first hour, in the second hour, and in the third hour, in which the levels should go down.
I hope everything goes well,
Best regards
Hi there! I’m 37 weeks pregnant and after my last visit to my GYN/OB, they told me that I have excessive amniotic fluid (polyhydramnios), but when I was 33 weeks pregnant it was okay 🙁 How is this possible? What are the consequences? I’m excessively concerned, does it lead to miscarriage? For my own peace of mind, give me an answer ASAP! Thanks