When a woman is pregnant, it is common for her to worry about possible complications that may occur during pregnancy. These problems can affect both the pregnant woman and her baby, or even both.
Complications during pregnancy may arise as an aggravation of a disease already existing in the woman before pregnancy. However, there are certain problems that appear for the first time in the pregnancy period.
Provided below is an index with the 7 points we are going to expand on in this article.
- 1.
- 2.
- 2.1.
- 2.2.
- 2.3.
- 2.4.
- 2.5.
- 2.6.
- 2.7.
- 2.8.
- 2.9.
- 3.
- 4.
- 4.1.
- 4.2.
- 4.3.
- 5.
- 6.
- 7.
Why are there complications during pregnancy?
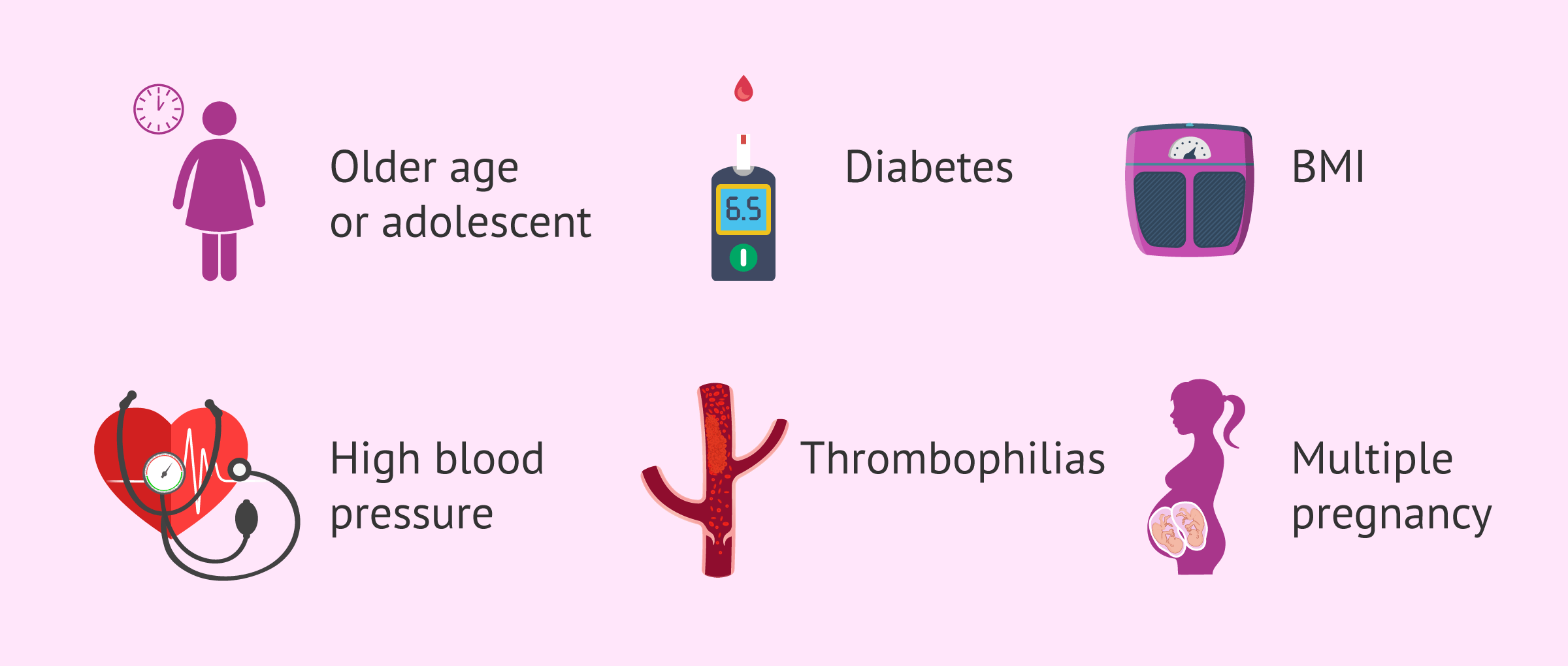
The causes of pregnancy complications will depend on the particular problem the woman is experiencing. However, there are certain circumstances that would be associated with an increased risk of obstetric complications. Some of them are mentioned below:
- Advanced maternal age or adolescent mother.
- Diabetes.
- Arterial hypertension.
- Obesity or underweight.
- Sexually transmitted diseases (STDs).
- Autoimmune diseases.
- Thrombophilias.
- Previous pregnancy with complications.
- Multiple pregnancy
- Consumption of alcohol, tobacco and/or drugs.
- Other diseases: cardiac, metabolic (e.g. thyroid), asthma, epilepsy...
For this reason, it is very important (and increasingly frequent) to go for consultation when a woman is planning to become pregnant. In this way, the specialist will be able to assess your medical history and whether certain risks are increased. Thus, the pregnant woman would be forewarned about them and more controlled to avoid their appearance or to detect them as soon as possible.
In addition, if the woman is under pharmacological treatment for any disease prior to pregnancy, the physician should assess whether it is necessary to suspend or modify it. Some drugs are not suitable for pregnancy and could pose risks to the fetus and to the proper development of the pregnancy.
On the other hand, this consultation will also be useful for the specialist to indicate, if necessary, some nutritional supplements that the woman should take, such as folic acid.
Possible complications
Among the different complications that may arise in pregnancy, we will mention some of the most common ones.
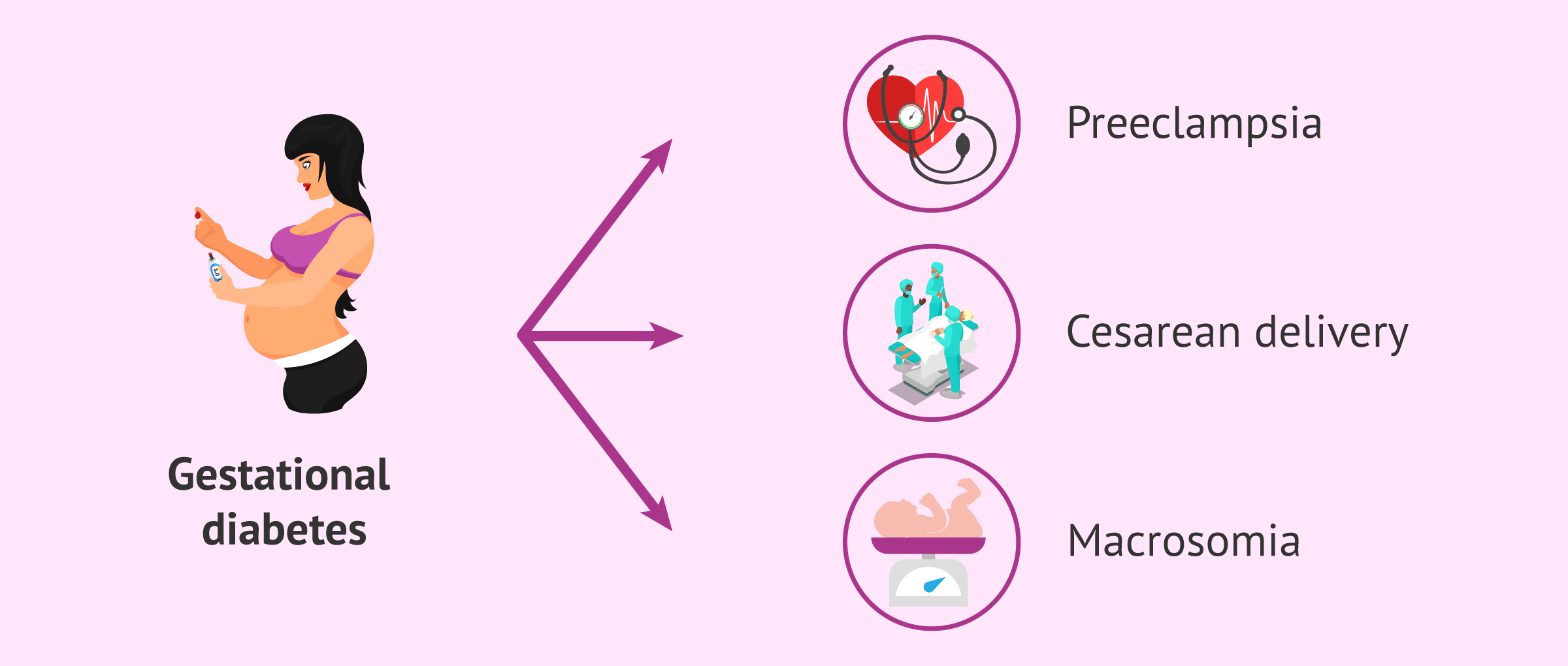
Gestational diabetes
In this case, diabetes appears or is detected in pregnancy and is characterized by elevated blood glucose levels(hyperglycemia) during pregnancy. Generally, this situation resolves once the woman gives birth, although she may develop type 2 diabetes in the future.
Gestational diabetes may increase rates of preeclampsia and cesarean delivery. This type of diabetes is also related to macrosomia (birth weight greater than 4 or 4.5 kg). In addition, hyperglycemia during pregnancy can also have long-term consequences for the baby, such as an increased risk of obesity and type 2 diabetes.
The ideal is to keep maternal blood glucose levels under control, with nutritional intervention accompanied by exercise and, if necessary, drugs.
If you are interested in reading more about this topic, we recommend the following article: What is gestational diabetes - Causes, symptoms, and treatment?
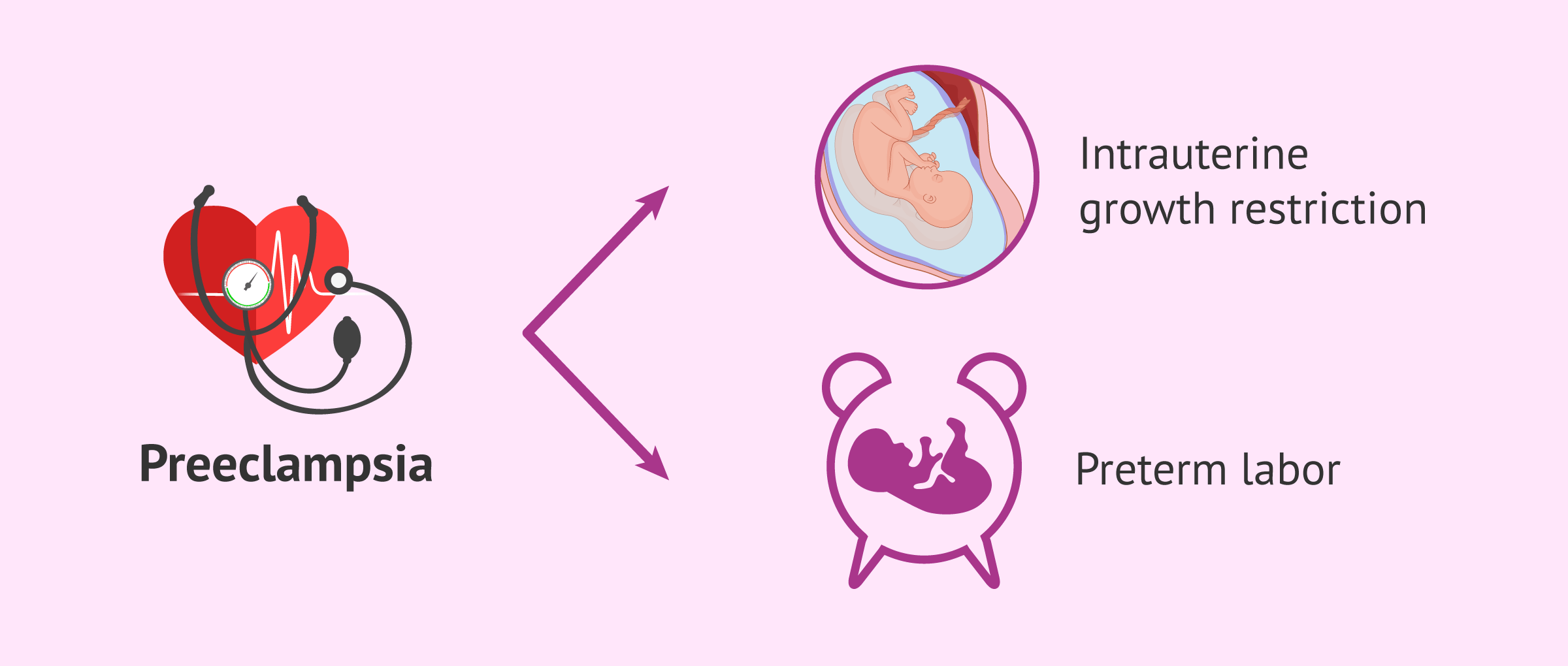
Preeclampsia.
Preeclampsia is a complication that can appear from the 20th week of gestation or in the first weeks after delivery. This complication is associated with hypertension and the presence of protein in the urine(proteinuria). However, this disorder can also involve other organs, i.e., it is multisystemic.
Preeclampsia, because it can affect the placenta, may cause intrauterine growth restriction or premature delivery.
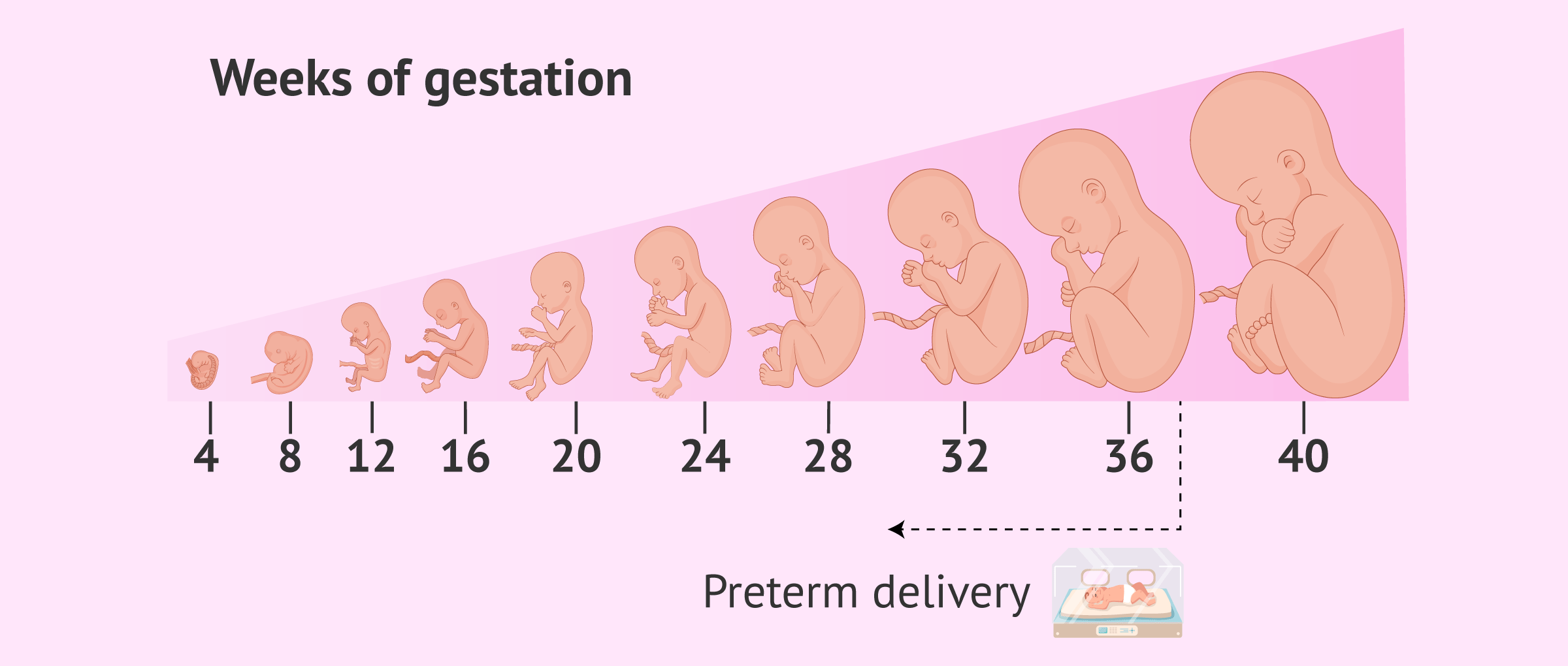
Premature delivery
Generally, preterm labor is referred to as preterm labor when it occurs before 37 weeks of gestation. Premature birth can have important consequences for the baby, since, for example, its respiratory system will not be mature.
Therefore, the earlier the delivery occurs with respect to the term delivery date, the more complications the baby may have.
If you want to know more in-depth about preterm labor, you can continue reading on the following link: What causes preterm labor - Risks, causes, and symptoms.
Spontaneous miscarriage
This is the involuntary loss of a pregnancy before the 20th week of gestation. Most often, miscarriages occur in the first trimester of pregnancy and sometimes when the woman is not even aware that she is pregnant.
Symptoms of a threatened miscarriage include vaginal bleeding and abdominal pain. If a woman has these symptoms, it is best to consult a gynecologist immediately so that he or she can quickly assess the situation. Although it is sometimes unavoidable, it is important to mention that not all threatened miscarriages end with a gestational loss.
You can read much more information about miscarriage in the following article: Miscarriage: symptoms, causes, and consequences.
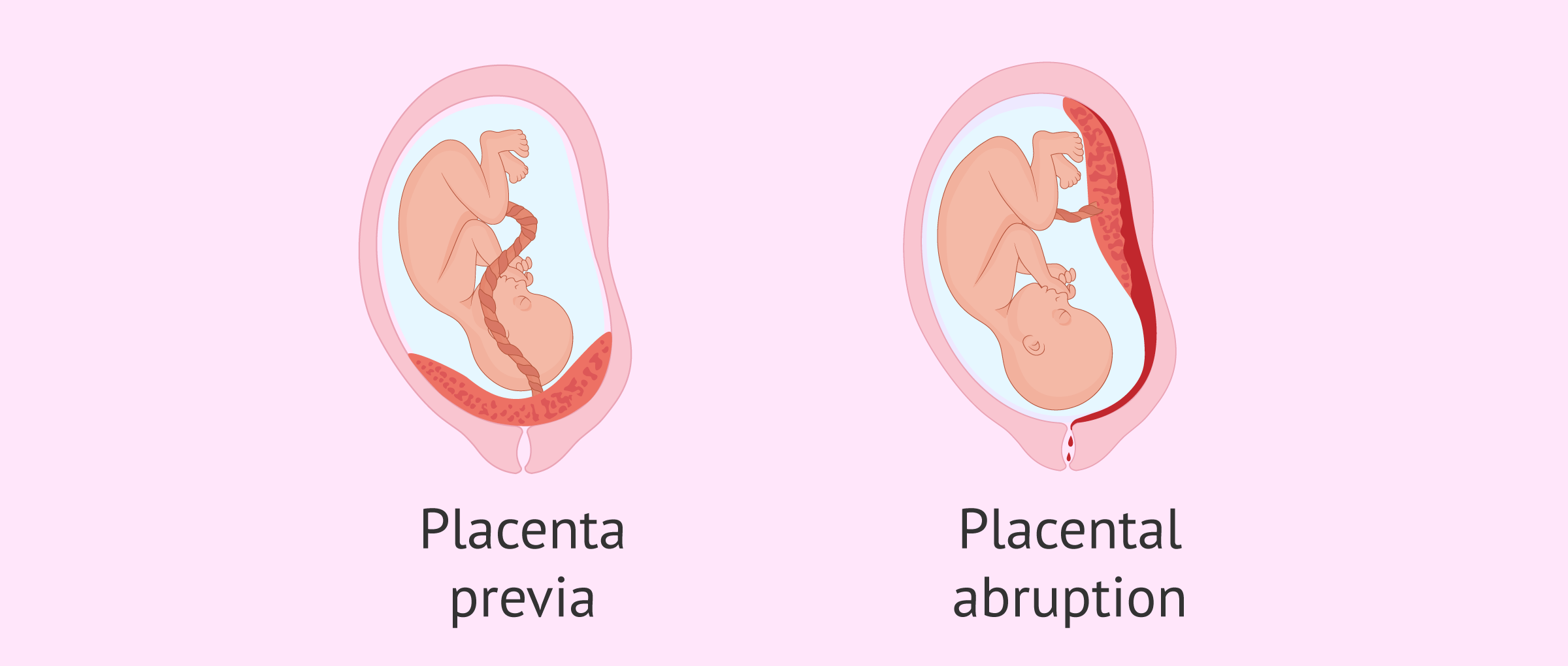
Problems with the placenta
During pregnancy, certain problems related to the placenta may also occur, such as placenta previa or premature detachment.
Placenta previa refers to a placenta that completely or partially covers the opening of the cervix and thus the birth canal. When diagnosed early in gestation, placenta previa may resolve. Otherwise, the pregnant woman will most likely give birth by cesarean section.
Premature detachment of the placenta is a complication in which the placenta "detaches", which leads to the baby receiving less oxygen and nutrients and the mother may suffer hemorrhage.
Hyperemesis gravidarum
Hyperemesis gravidarum is the constant presence of nausea and vomiting during pregnancy. It is, therefore, a more severe form of nausea and vomiting that many women experience in the first trimester of pregnancy. This situation leads to dehydration, malnutrition, and weight loss in pregnant women.
Symptoms of hyperemesis gravidarum are most noticeable and significant at 12 weeks, but usually, improve after 20 weeks of gestation.
As for the effects on the baby, hyperemesis gravidarum would be related to premature delivery, small-for-gestational-age baby, and low birth weight.
Anemia
Iron deficiency anemia or iron deficiency anemia can be common in pregnant women since iron needs are greater during pregnancy.
Iron is part of hemoglobin, which is essential for the transport of oxygen in our blood (in red blood cells). Thus, if hemoglobin is found at low levels, it could be related to preterm delivery and low birth weight. However, high hemoglobin levels would also be associated with adverse outcomes.
For this reason, the specialist will assess the pregnant woman's iron levels and will indicate the appropriate supplementation and dosage if deemed appropriate.
Postpartum depression.
The pregnant woman may feel empty or sad and even have mixed feelings for a few days after delivery, which may be related to the hormonal changes she has experienced.
However, the woman may present symptoms of depression on a more prolonged basis (postpartum depression). Among these symptoms can be found:
- Sadness.
- Crying.
- Impotence, tiredness.
In addition, there may be a lack of interest in the baby. Thus, this situation leads to an affectation in the mother-child relationship, involving not only the mother but also the baby's health and care.
It is very important to detect postpartum depression as soon as possible and see a specialist. He will determine the best way to help the woman, either through therapy or, if he deems it appropriate, with the administration of certain drugs.
Infections
An infection in the mother can be transmitted to the baby during pregnancy, delivery, or breastfeeding. Therefore, it is especially important to check, before becoming pregnant, whether the woman has an infection that could affect the fetus, as well as whether she is immunized against certain infections. In this way, the woman can receive some type of treatment if necessary or, perhaps, the administration of a vaccine may be advisable.
On the other hand, it will be important to avoid contracting infections during pregnancy. The pregnant woman should take into account certain recommendations such as:
- Be especially careful when cooking meat, as it should not be consumed raw or undercooked. Fish, seafood, and eggs should not be consumed raw.
- Wash all fruits and vegetables, especially if they are to be eaten raw.
- Do not drink milk or cheeses that are not pasteurized.
- Wash hands immediately after touching raw food, the utensils with which they have been handled (and wash them properly), and also after touching animals.
In addition, the pregnant woman should be careful with cats and their feces, as well as when cleaning her litter box. The woman should wear gloves to do this and it is even better if someone else can change the sand for her. This reduces the risk of the pregnant woman contracting toxoplasmosis.
Other pregnancy complications
Despite the above, pregnant women may also be more susceptible to other complications, such as gum problems or hemorrhoids.
Hormonal changes during pregnancy lead to an increase in gum inflammation in pregnant women. In addition, periodontal disease may be related to adverse effects in pregnancy such as preterm delivery, low birth weight, and preeclampsia.
On the other hand, it is also common for pregnant women to suffer from constipation, which favors the appearance of hemorrhoids. Therefore, it is recommended that women eat a diet that includes fiber and drink enough water.
FAQs from users
What should I do if I suspect I have a urinary tract infection in pregnancy?
The ideal is to consult a doctor. A urine culture should be performed and if it is positive, antibiotics should be started. With the result of the urine culture, check whether the germ is sensitive or not to the antibiotic.
If the urine culture is normal but the patient has urinary symptoms, treatment should also be given.
Any urinary tract infection in a pregnant woman should be well treated to avoid possible complications.
What is a high-risk pregnancy?
A high-risk pregnancy is a pregnancy in which the woman has an increased risk of presenting complications during gestation, and therefore requires greater control by specialists during pregnancy, childbirth, and the postpartum period. Thus, an attempt will be made to prevent the appearance of these complications, to keep them under control, or to detect them early, in order to avoid problems for the woman or the baby.
Although care should be personalized according to the particular situation of the pregnant woman, in this type of pregnancy physical activity is often limited and rest is recommended. In addition, it will be essential to attend all the appointments scheduled by the specialist.
What complications can a pregnancy have if the woman is Rh-negative?
If the woman is Rh negative (i.e. her red blood cells do not have the Rh factor), she may detect the fetus' red blood cells as foreign if they do have the Rh factor. This situation can occur if the fetus has inherited the Rh factor from its other parent, thus being Rh positive.
Thus, the Rh-negative mother would produce antibodies against these fetal red blood cells, which she does not recognize as her own, upon contact during pregnancy or delivery.
However, during the first pregnancy with this condition, the antibodies created usually only "sensitize" the mother to the condition. However, it is more common that complications can occur in subsequent pregnancies, if the fetus is also Rh positive, as the amount of antibodies produced would be greater. These antibodies can cross the placental barrier and attack the red blood cells of the fetus.
One of the main consequences would be fetal anemia, which can have different repercussions depending on its severity.
However, these problems can be avoided by administering Rh immunoglobulins to the woman in situations where indicated.
Recommended readings
If you are pregnant, you may want to learn more about the first month of pregnancy. To do so, you can visit the following link: The first month of pregnancy: first symptoms and care for the mother.
On the other hand, if you are interested in learning more about care during pregnancy, we recommend you read the following article: Health in pregnancy: nutrition, care, and possible problems.
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
Austin K, Wilson K, Saha S. Hyperemesis Gravidarum. Nutr Clin Pract. 2019 Apr;34(2):226-241. (See)
Boelig RC, Barton SJ, Saccone G, Kelly AJ, Edwards SJ, Berghella V. Interventions for treating hyperemesis gravidarum. Cochrane Database Syst Rev. 2016 May 11;(5):CD010607. (See)
Brannon PM, Taylor CL. Iron Supplementation during Pregnancy and Infancy: Uncertainties and Implications for Research and Policy. Nutrients. 2017 Dec 6;9(12):1327. (See)
Brown B, Wright C. Safety and efficacy of supplements in pregnancy. Nutr Rev. 2020 Oct 1;78(10):813-826. (See)
De Haro K, Toledo K, Fonseca Y, Arenas D, Arenas H, Leonher K. Hiperemesis gravídica: manejo y consecuencias nutricionales; reporte de caso y revisión de literatura [Hyperemesis gravidarum: management and nutritional implications; case report and review of literature]. Nutr Hosp. 2014 Oct 3;31(2):988-91. Spanish. (See)
Dewey KG, Oaks BM. U-shaped curve for risk associated with maternal hemoglobin, iron status, or iron supplementation. Am J Clin Nutr. 2017 Dec;106(Suppl 6):1694S-1702S. (See)
Duley L, Henderson‐Smart DJ, Walker GJA. Interventions for treating pre‐eclampsia and its consequences: generic protocol. Cochrane Database of Systematic Reviews 2009, Issue 2. Art. No.: CD007756. (See)
Raju K, Berens L. Periodontology and pregnancy: An overview of biomedical and epidemiological evidence. Periodontol 2000. 2021 Oct;87(1):132-142. (See)
Tieu J, McPhee AJ, Crowther CA, Middleton P, Shepherd E. Screening for gestational diabetes mellitus based on different risk profiles and settings for improving maternal and infant health. Cochrane Database Syst Rev. 2017 Aug 3;8(8):CD007222. (See)
Zito G, Della Corte L, Giampaolino P, Terzic M, Terzic S, Di Guardo F, Ricci G, Della Pietà I, Maso G, Garzon S. Gestational diabetes mellitus: Prevention, diagnosis and treatment. A fresh look to a busy corner. J Neonatal Perinatal Med. 2020;13(4):529-541. (See)
FAQs from users: 'What should I do if I suspect I have a urinary tract infection in pregnancy?', 'What is a high-risk pregnancy?' and 'What complications can a pregnancy have if the woman is Rh-negative?'.
Authors and contributors
More information about Cristina Algarra Goosman




Hello, I did the 1h glucose test and I got some strange values, I have been told that I have to repeat it, I may have gestational diabetes? What should I do?
Hello Selina32,
Generally, when glucose testing is performed in pregnant women, the assimilation of large amounts of sugar over the course of an hour is observed. If the results are inconclusive it may be due to some problem in performing the test. For this reason, they usually repeat the test with a greater control or perform a more extensive test with a duration of about 3 hours.
In the event of a positive result and a diagnosis of gestational diabetes, the doctor would prescribe a low-sugar diet and more extensive gestational controls.
I hope everything goes well!
Best regards.
Hi, I’m pregnant and these last few weeks I’ve been having trouble going to the bathroom, and I think it’s possible that I may have gotten sores or even hemorrhoids. Is there any solution for them? What can I do, I’m afraid they will be there for life.
Hello Ella,
Hemorrhoids that appear during pregnancy or childbirth tend to disappear within a couple of weeks. It is true that not all hemorrhoids remit as there are degrees of hemorrhoids, for the more severe ones if a small surgical intervention would be recommended to remove them.
During the rest of your pregnancy, I recommend you eat a diet rich in fiber and stay hydrated to avoid constipation and limit the pressure in the area.
I hope I have helped you,
Best regards.