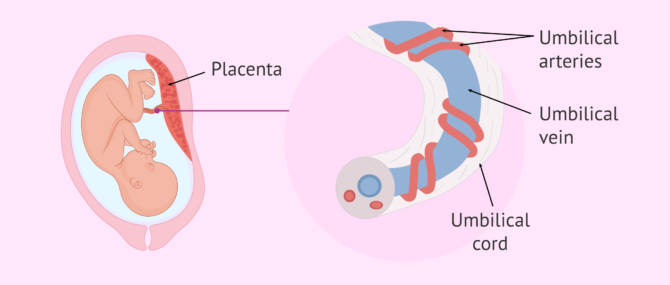
The umbilical cord has the important job of connecting the placenta to the baby. In this way, it is responsible for supplying the fetus with the blood with the oxygen and nutrients it needs and for removing waste products back to the placenta.
Although in many pregnancies it goes unnoticed and is not given importance, several anomalies can occur in the umbilical cord. Some of them can be a serious complication, especially when blood flow (and therefore oxygen flow) is compromised.
Provided below is an index with the 11 points we are going to expand on in this article.
- 1.
- 2.
- 3.
- 4.
- 5.
- 6.
- 7.
- 8.
- 8.1.
- 8.2.
- 9.
- 10.
- 11.
How important is the umbilical cord?
The umbilical cord is a flexible, helical, tubular structure that acts as a link between mother and baby during pregnancy. For this purpose, it extends from the placenta to the baby's future navel. Its formation begins around 4-5 weeks of gestation and it usually measures about 50-65 cm (although there can be much variation in its length).
The main function of the umbilical cord is to provide oxygen and nutrients to the baby, as well as to remove waste products generated by the fetus. To carry out these functions, the umbilical cord consists of three blood vessels that are surrounded by the so-called wharton's jelly:
- Umbilical vein: for the transport of oxygen and nutrients in the placenta-fetus direction.
- Umbilical arteries: there are two of them and they are in charge of removing waste substances in the feto-placental direction.
Thus, because the umbilical cord has such an important function, a disruption affecting the flow of oxygen and nutrients could cause serious problems.
Nuchal umbilical cord or umbilical cord return
Nuchal umbilical cord refers to the situation in which the umbilical cord is wrapped around the baby's neck, giving one or more turns. It can occur in approximately one in every four or five births, making it a common occurrence.
Cord twisting may be detected on ultrasound during pregnancy, but this situation does not necessarily lead to complications. The umbilical cord may even unwind on its own due to the baby's movements and turns.
When the nuchal umbilical cord is present at the time of delivery, it is quite possible that a vaginal delivery can be carried out without problems. In any case, if the baby shows an abnormal heart rate during delivery, a cesarean section will be performed.
Finally, it is important to mention that the umbilical cord may be detected by ultrasound to be wrapped around some other part, such as the baby's hands. Generally, this situation does not compromise the flow of nutrients and oxygen to the baby.
True knot in the umbilical cord
Occasionally, the umbilical cord may have knots that form when the fetus passes through a loop of the cord. This happens especially in the first stage of pregnancy, when the baby is smaller and moves very freely inside the uterus. In addition, it may be favored if a long umbilical cord is present.
The main problem with knots in the umbilical cord is that they become tight. If this occurs, the knot can become so tight that blood flow and, therefore, the delivery of oxygen and nutrients to the fetus is impeded or prevented. Therefore, it is related to the risk of loss of fetal well-being and even intrauterine or perinatal death.
The specialist can look for knots in the umbilical cord by means of ultrasound (color Doppler), especially if there is any risk factor such as polyhydramnios (increased volume of amniotic fluid). Sometimes, however, the knot (or knots) in the umbilical cord is not discovered until the time of delivery.
Similarly, the fetal heart rate will also be monitored. Therefore, although vaginal birth is possible, if an alteration in the heart rate is detected, an emergency cesarean section may be necessary.
Short umbilical cord
The umbilical cord is said to be short when it measures less than 35 cm, which happens in 6% of the cases.
In addition to the baby having less freedom to move around in the uterus, a short umbilical cord may affect the baby's development and may be related to fetal malformations. However, it can also produce other obstetric complications such as placental abruption.
The umbilical cord is difficult to measure in an ultrasound, but, in the event that it is detected during pregnancy that the umbilical cord is short, the woman may have to go to check-ups more frequently. Similarly, if any complication occurs, the baby will usually have to be delivered by emergency cesarean section.
Umbilical cord prolapse
Umbilical cord prolapse occurs when the cord comes out of the birth canal before the baby does. Therefore, this situation may cause the umbilical cord to be compressed when the baby's body emerges. If this occurs, the proper flow of blood through the vessels of the umbilical cord would be impeded.
This umbilical cord-related complication may be present in 1-6 out of 1000 deliveries, being more common, for example, if the baby is breech or if there is premature rupture of membranes.
Limiting the infant's blood supply of oxygen and nutrients can cause a slowing of the heart rate and serious complications (such as brain damage) and can even be fatal. Therefore, the most common procedure is an emergency cesarean section, so that this lack of blood flow does not harm the baby.
Single umbilical artery
In this anomaly, the umbilical cord has one vein and a single artery (instead of one vein and two arteries). Single umbilical artery occurs in 1% of singleton pregnancies and in 5% of multiple pregnancies.
It is possible that the single umbilical artery is present along with other problems such as renal or cardiac malformations or genetic alterations. Therefore, if the specialist detects a single umbilical artery in a pregnancy control ultrasound, some tests may be requested to check these aspects.
In addition, the single umbilical artery would be related to low birth weight and preterm delivery, so revisions may be more frequent.
Previous Vasa
Vasa previa is a condition in which the blood vessels do not directly join the umbilical cord and the placenta. In vasa previa, these blood vessels escape from the umbilical cord and, unprotected, pass over the cervix or very close to it through the membranes surrounding the baby.
Thus, when the woman's water breaks, hemorrhage may occur due to the rupture of these blood vessels. The baby may lose a large amount of blood, which can be life-threatening, and the woman will experience painless bleeding after her membranes rupture.
Given its importance, the pregnant woman with vasa previa will attend frequent fetal heart rate checks. The woman may even be hospitalized in late pregnancy to monitor the baby more closely.
In addition, corticosteroids are most commonly administered to accelerate fetal lung maturation and a cesarean section is scheduled around 35 weeks gestation (or earlier if there is any risk).
FAQs from users
What are the risk factors for cord prolapse?
Umbilical cord prolapse is a complication related to the umbilical cord, when the umbilical cord comes out into the vagina before the baby does. This situation may be increased when certain risk factors are present, such as:
- Premature rupture of membranes.
- Low birth weight (less than 2500 grams).
- Breech baby or other abnormal presentations.
- Multiple pregnancy.
- Polyhydramnios.
In addition, other maternal factors, such as multiparity and uterine abnormalities or fibroids, may also be associated with an increased risk of umbilical cord prolapse.
Is it possible that the umbilical cord is tangled in two turns?
Yes, the umbilical cord can be wrapped around the baby's neck twice or even three times. Although cord wraps or cord circles are much feared, the truth is that the baby can be born vaginally without any problems and, if any complications arise, a caesarean section would be performed to avoid risks.
Suggested for you
On the other hand, if you want to learn more about cesarean delivery, you can read this article: Cesarean section: how is it performed and what care is needed?
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
Hasegawa J. Ultrasound screening of umbilical cord abnormalities and delivery management. Placenta. 2018 Feb;62:66-78. doi: 10.1016/j.placenta.2017.12.003. Epub 2017 Dec 7. PMID: 29405969. (View)
Mitchell SJ, Ngo G, Maurel KA, Hasegawa J, Arakaki T, Melcer Y, Maymon R, Vendittelli F, Shamshirsaz AA, Erfani H, Shainker SA, Saad AF, Treadwell MC, Roman AS, Stone JL, Rolnik DL. Timing of birth and adverse pregnancy outcomes in cases of prenatally diagnosed vasa previa: a systematic review and meta-analysis. Am J Obstet Gynecol. 2022 Aug;227(2):173-181.e24. doi: 10.1016/j.ajog.2022.03.006. Epub 2022 Mar 10. PMID: 35283090. (View)
Pavalagantharajah S, Villani LA, D'Souza R. Vasa previa and associated risk factors: a systematic review and meta-analysis. Am J Obstet Gynecol MFM. 2020 Aug;2(3):100117. doi: 10.1016/j.ajogmf.2020.100117. Epub 2020 Apr 15. PMID: 33345868. (View)
Peesay M. Nuchal cord and its implications. Matern Health Neonatol Perinatol. 2017 Dec 6;3:28. doi: 10.1186/s40748-017-0068-7. PMID: 29234502; PMCID: PMC5719938. (View)
Pergialiotis V, Fanaki M, Bellos I, Tzortzis A, Loutradis D, Daskalakis G. Evaluation of umbilical cord entanglement as a predictive factor of adverse pregnancy outcomes: A meta-analysis. Eur J Obstet Gynecol Reprod Biol. 2019 Dec;243:150-157. doi: 10.1016/j.ejogrb.2019.10.038. Epub 2019 Nov 1. PMID: 31704532. (View)
Petrikovsky BM. Prevention of umbilical cord prolapse in high-risk patients. Am J Obstet Gynecol. 2022 Dec;227(6):928-929. doi: 10.1016/j.ajog.2022.07.008. Epub 2022 Jul 13. PMID: 35841940. (View)
Rabe H, Mercer J, Erickson-Owens D. What does the evidence tell us? Revisiting optimal cord management at the time of birth. Eur J Pediatr. 2022 May;181(5):1797-1807. doi: 10.1007/s00431-022-04395-x. Epub 2022 Feb 2. Erratum in: Eur J Pediatr. 2022 Feb 14;: PMID: 35112135; PMCID: PMC9056455. (View)
Santana EFM, Castello RG, Rizzo G, Grisolia G, Araujo Júnior E, Werner H, Lituania M, Tonni G. Placental and Umbilical Cord Anomalies Diagnosed by Two- and Three-Dimensional Ultrasound. Diagnostics (Basel). 2022 Nov 16;12(11):2810. doi: 10.3390/diagnostics12112810. PMID: 36428871; PMCID: PMC9689386. (View)
Sayed Ahmed WA, Hamdy MA. Optimal management of umbilical cord prolapse. Int J Womens Health. 2018 Aug 21;10:459-465. doi: 10.2147/IJWH.S130879. PMID: 30174462; PMCID: PMC6109652. (View)
Villani LA, Pavalagantharajah S, D'Souza R. Variations in reported outcomes in studies on vasa previa: a systematic review. Am J Obstet Gynecol MFM. 2020 Aug;2(3):100116. doi: 10.1016/j.ajogmf.2020.100116. Epub 2020 Apr 16. PMID: 33345867. (View)
Wong L, Kwan AHW, Lau SL, Sin WTA, Leung TY. Umbilical cord prolapse: revisiting its definition and management. Am J Obstet Gynecol. 2021 Oct;225(4):357-366. doi: 10.1016/j.ajog.2021.06.077. Epub 2021 Jun 26. PMID: 34181893. (View)
FAQs from users: 'What are the risk factors for cord prolapse?' and 'Is it possible that the umbilical cord is tangled in two turns?'.






Hello, I’m 26 and my boyfriend is 28. He’s a marijuana addict and we’re planning to have baby soon. I’d like to know if during pregnancy I could have any complication related to his addiction or something like that. Will my baby develop a cord knot? Thank you very much
Dear Adele78,
The following topic may be of interest: Marijuana, pregnancy and male infertility.
Should you have any further question, do not hesitate to ask.
Best wishes