The concept of preterm birthor preterm birth according to the World Health Organization (WHO) refers to a birth that occurs before the 37th week of pregnancy.
Generally, the more developed the newborn is, the fewer the consequences and complications of premature birth. This means that a preterm delivery at 36 weeks carries less danger to the baby than one that occurs at 34 weeks.
Provided below is an index with the 11 points we are going to expand on in this article.
- 1.
- 2.
- 3.
- 3.1.
- 3.2.
- 4.
- 5.
- 5.1.
- 5.2.
- 6.
- 7.
- 8.
- 8.1.
- 8.2.
- 8.3.
- 8.4.
- 8.5.
- 8.6.
- 8.7.
- 9.
- 10.
- 11.
What is preterm labor?
A premature birth is a complication at the obstetrical and neonatal level since it can cause serious health problems in the mother and the newborn. In the most severe cases, extreme premature delivery can lead to neonatal death.
Depending on the time of pregnancy at which it occurs, preterm deliveries are classified as follows:
- Extreme prematurity: premature birth before 28 weeks.
- Severe preterm labor: between 28 and 31 weeks of gestation.
- Moderate prematurity: delivery between 32 and 33 weeks.
- Borderline or mild preterm labor: from 34 to 36 weeks.
Causes of preterm labor
It is estimated that about 5-10% of births occur prematurely. Although in some cases the cause of preterm labor may be suspected, in most cases the exact etiology is quite unclear.
Some of the most common causes related to the birth of a premature baby are:
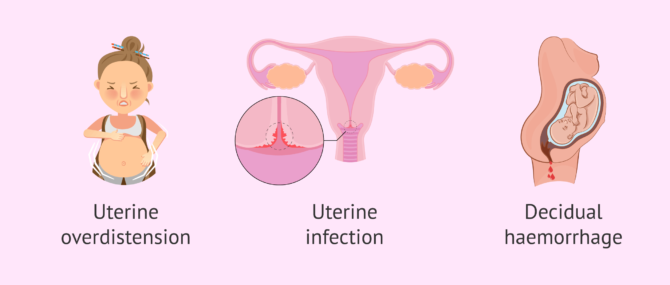
- Uterine overdistension: loss of muscle tone of the uterus that prevents the uterus from regaining its natural size.
- Uterine infection or inflammation: certain bacterial components can damage the fetal membranes, causing them to rupture and triggering preterm labor. An infection that specifically affects the uterus can also cause preterm labor.
- Decidual hemorrhage is a type of vaginal bleeding that can occur during pregnancy.
Even if a woman does not present any complications during gestation and follows all the necessary care during pregnancy, it is possible that a premature delivery may occur, because unfortunately this complication can occur spontaneously.
Risk Factors
There are a number of known risk factors that can increase the likelihood of preterm birth. However, it is believed that more than half of such deliveries occur in pregnancies with no identifiable risk factors.
It is important to analyze the risk factors according to the nature of each of them: maternal or gestational.
Maternal risk factors
Certain conditions in the pregnant woman may increase the threat of preterm labor. Some of them are:
- Unhealthy lifestyle habits in pregnancy.
- Obesity or excessive weight gain in pregnancy.
- Suffering infectious processes.
- Previous preterm labor.
- History of cervical surgery or conization.
- Arterial hypertension.
- Belonging to the black or Hispanic race.
In addition, social factors such as economic status and education, as well as psychosocial factors such as stress, can increase the risk of preterm birth. However, this does not mean that the presence of some of these factors necessarily implies prematurity.
Gestational risk factors
Some conditions during gestation may facilitate preterm delivery, such as:
- Multiple pregnancy.
- Polyhydramnios: excessive presence of amniotic fluid.
- Premature bag rupture.
- Cervical insufficiency: the cervix does not remain closed.
- Bleeding in the first trimester.
- Placental defects: premature detachment or placenta previa.
A history of miscarriage in the second trimester of gestation, i.e., beyond the 16th week of pregnancy, is also associated with an increased risk of preterm delivery.
What are the symptoms of preterm labor?
For the diagnosis of preterm labor, it is important for the pregnant woman to be alert to any warning signs. If you experience any of these conditions before 37 weeks, it is important to contact your health care provider:
- Regular contractions of 15 seconds to two minutes every 15 minutes or less.
- Expulsion of the mucus plug.
- Increase and/or changes in vaginal discharge.
- Vaginal bleeding.
- Abdominal pain.
- Increased pressure in the pelvic area.
On certain occasions, the woman may have a feeling of anxiety or uneasiness along with chills or even an increase in body temperature.
In any case, it is important that nervousness does not take over the situation and, in case of any suspicious symptom, consult your gynecologist or midwife.
Diagnostic Tests
When a woman has symptoms of preterm labor or is at risk of preterm labor, there are two medical tests that can be performed to confirm the diagnosis:
Measurement of the cervix
The cervix is a small cylinder-shaped canal that connects the uterine cavity to the vagina. As the pregnancy develops, it becomes shorter and shorter, measuring an average of 25 mm, until it "disappears" in the moments prior to delivery.
When the physician suspects that the patient may be at risk of preterm labor, he or she may proceed to measure the length of the cervical canal by transvaginal ultrasound, which allows a more accurate visualization and measurement of cervical length.
If the length of the cervix is reduced and there is no urgency to advance labor, the obstetrician may consider administering progesterone vaginally and/or performing a cervical cerclage to obstruct the area.
Fetal fibronectin detection
Fetal fibronectin is a protein produced by fetal membranes that allows them to adhere to the uterine wall. For the measurement of this protein, a vaginal smear is performed.
If the test detects that the amount of fetal fibronectin is normal, delivery will probably not occur within the next two weeks.
If, on the other hand, the fibronectin concentration is abnormally high, there is a risk of premature delivery. However, the detection of fetal fibronectin is not a definitive test and it is important to take into account other factors such as gestational age or size of the baby in order to establish a treatment.
Treatment for possible preterm labor
Whenever possible, the first strategy is to delay birth so that the fetus can continue to grow and develop normally. However, many preterm deliveries are unavoidable and are induced to avoid worse consequences.
In the event of a slight threat of premature labor, absolute rest is recommended for the pregnant woman, since staying in bed reduces the pressure on the uterus and cervix and the probability of contractions.
It is recommended that the woman try to stay hydrated to increase the concentration of blood in her body and try to reduce stressful situations or activities. In the most risky cases, where the woman is admitted to the hospital, intravenous fluids are administered to keep her as well hydrated as possible. In addition, the physician may give drugs called tocolytics to slow down labor.
Regarding the infant, one of the most common complications in the birth of a premature baby is that its lungs are still too immature and can suffer serious respiratory problems. To prevent this, glucocorticoids are administered to the pregnant woman to stimulate the maturation and growth of the fetal lungs. It is necessary that the gestation has exceeded at least 24 weeks of development to be able to administer this medication.
Premature babies and special care
An early birth can pose certain health and developmental problems for premature babies, as the last 8 weeks of pregnancy are the key period during which the fetus experiences its greatest growth.
As mentioned above, respiratory system problems are the most common in this type of newborn, since the lungs are one of the last organs to develop. It is also common that they may present problems in the digestive, renal or immune system, as well as in vision.
Because of all this, premature babies need special care such as assisted ventilation, heat application (because of their prematurity they have problems retaining body heat) or receiving food intravenously, since they do not coordinate sucking, swallowing and breathing correctly.
For this reason, it is not possible for a premature baby to receive nursing care at home, as medical equipment is needed and this implies the baby's stay, for a more or less prolonged period, in the neonatal ICU. If you want to know more about the characteristics of premature babies, visit this link: Preterm infants.
FAQs from users
Is a preterm birth more likely with twins?
According to the World Health Organization (WHO), a preterm birth occurs when the child is born before the week 37 of pregnancy. Some of the most common causes of preterm birth are:
- Overdistention of the uterus: loss of tone in the uterine musculature that prevents this organ to recover its normal size.
- Infection or uterine inflammation: certain bacteria can damage fetal membranes by causing its rupture and triggering a preterm birth. An infection that affects the uterus directly may lead to preterm birth as well.
- Decidual bleeding: a type of vaginal bleeding that may occur while a woman is pregnant.
There exist many risk factors that can lead to premature birth, including obesity, high blood pressure, etc. A multiple pregnancy is one of these factors.
Is premature birth more common in an IVF process?
There is no direct association between assisted reproduction treatment and preterm birth. It is common to find gynaecological pathologies (myomas, uterine malformations...) in women with sterility or infertility. These pathologies can cause premature birth, but not the technique itself.
What should a premature baby be fed?
According to experts, breast milk is the best food for newborns, especially premature infants. However, in the case of premature babies, since they cannot suckle properly, it is necessary to introduce food through nasogastric or stomach tubes. Sometimes, due to the sequelae of prematurity at birth, it is necessary to supplement their diet with iron.
Do you get the same sick leave when you give birth prematurely?
Generally, yes, the same leave is granted after a normal birth or premature birth. However, a threatened premature birth is a reason for sick leave, which can be extended by maternity leave.
What was the weight of the world's smallest premature baby?
There are many cases of premature babies in the world who, fortunately, have managed to survive. One of the most shocking cases is that of a girl, Amilia Taylor, who was born in a Miami hospital at 22 weeks gestation and weighing 280 grams.
Can a premature baby be delivered naturally?
Yes, it is possible for an early delivery to occur through the vaginal canal. That is, it is not always necessary to have a cesarean section in the case of preterm labor.
What are the consequences of premature birth?
Preterm births can be a danger to the health of both mother and baby. Depending on how early in the pregnancy the baby is born, different problems will develop.
Babies born early may have health problems. For example, many premature babies have respiratory disorders and brain damage, among others.
For this reason, strict medical control is essential to ensure the correct development of the baby and to reduce possible sequelae as much as possible.
Suggested for you
Being prepared to give birth is very important. If you are interested in knowing what you can do, we recommend you to visit the following article: How is childbirth preparation - Theory and practice.
In addition, during pregnancy, some complications may arise and it is essential to detect them in time. If you want to know more information about this topic, you can access this link: What are the most common pregnancy complications?
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
Eduardo B da Fonseca, Rievani Damião, Daniela Aires Moreira. Preterm birth prevention. Best Pract Res Clin Obstet Gynaecol. 2020 Nov;69:40-49 (View)
Joshua P Vogel, Saifon Chawanpaiboon, Ann-Beth Moller, Kanokwaroon Watananirun, Mercedes Bonet, Pisake Lumbiganon. The global epidemiology of preterm birth. Best Pract Res Clin Obstet Gynaecol. 2018 Oct;52:3-12 (View)
Margie A Ream, Lenora Lehwald. Neurologic Consequences of Preterm Birth. Curr Neurol Neurosci Rep. 2018 Jun 16;18(8):48. doi: 10.1007/s11910-018-0862-2.
Robert L Goldenberg, Jennifer F Culhane, Jay D Iams, Roberto Romero. Epidemiology and causes of preterm birth. Lancet. 2008 Jan 5;371(9606):75-84. doi: 10.1016/S0140-6736(08)60074-4 (View)
Wanda D Barfield. Public Health Implications of Very Preterm Birth. Clin Perinatol. 2018 Sep;45(3):565-577. doi: 10.1016/j.clp.2018.05.007 (View)
FAQs from users: 'Is a preterm birth more likely with twins?', 'Is premature birth more common in an IVF process?', 'What should a premature baby be fed?', 'Do you get the same sick leave when you give birth prematurely?', 'What was the weight of the world's smallest premature baby?', 'Can a premature baby be delivered naturally?' and 'What are the consequences of premature birth?'.
Authors and contributors