Puerperal fever is the clinical manifestation of an infection in women after childbirth.
This puerperal infection is due to injuries or complications caused to the genital tract during childbirth. In the past, puerperal fever was one of the leading causes of maternal death.
Today, postpartum infections are well controlled. The administration of antibiotics has been successful in reducing the frequency and severity of puerperal fever.
Provided below is an index with the 8 points we are going to expand on in this article.
- 1.
- 2.
- 3.
- 3.1.
- 4.
- 5.
- 5.1.
- 5.2.
- 5.3.
- 6.
- 7.
- 8.
Diagnosis of puerperal infection
The appearance of fever in the days following delivery is not always indicative of puerperal infection or sepsis. To be considered as such, the following requirements must be met:
- Fever is equal to or higher than 38 °C on at least 2 occasions separated by an interval of 6 hours.
- Fever appears between 24 hours after delivery and the following 6 weeks, a period known as puerperium.
In the first 24 hours after the birth of the baby, the temperature must be above 38.5 °C to be considered clinically relevant.
The milk surge may also cause the mother's temperature to rise for a few hours, but does not qualify as puerperal sepsis.
During the diagnosis of a puerperal infection, it is necessary to identify the source of infection on the one hand, and the causative agent on the other, i.e. the infectious microorganisms.
For this, the physician will have to assess the possible intrinsic risk factors of the mother, as well as the risk factors related to childbirth. In addition, he or she will perform a thorough physical examination, including breast and vaginal examination.
He will also order any necessary complementary tests: blood tests, blood culture, urine culture, endometrial culture, etc. It is very important to be able to identify the microorganisms causing the infection in order to apply the most appropriate treatment.
What are the symptoms of puerperal fever?
Obviously, fever is the main symptom of an infection during the postpartum period. However, there are other manifestations that indicate that something is wrong with women who have just given birth.
We will now discuss the possible signs and symptoms of a puerperal infection:
- General malaise
- Pallor
- Cold sweats
- Chills
- Tachycardia
- Headache
- Abundant and foul-smelling lochia (vaginal secretions typical of the puerperium)
- Abdominal pain
However, sometimes the only clinical manifestation of puerperal fever is low-grade fever.
Causes of puerperal fever
In general, puerperal infections are the consequence of a lack of hygienic care during labor or the puerperium, although it can also happen that a part of the placenta remains inside the uterus and causes complications.
The following are the main causes of puerperal fever:
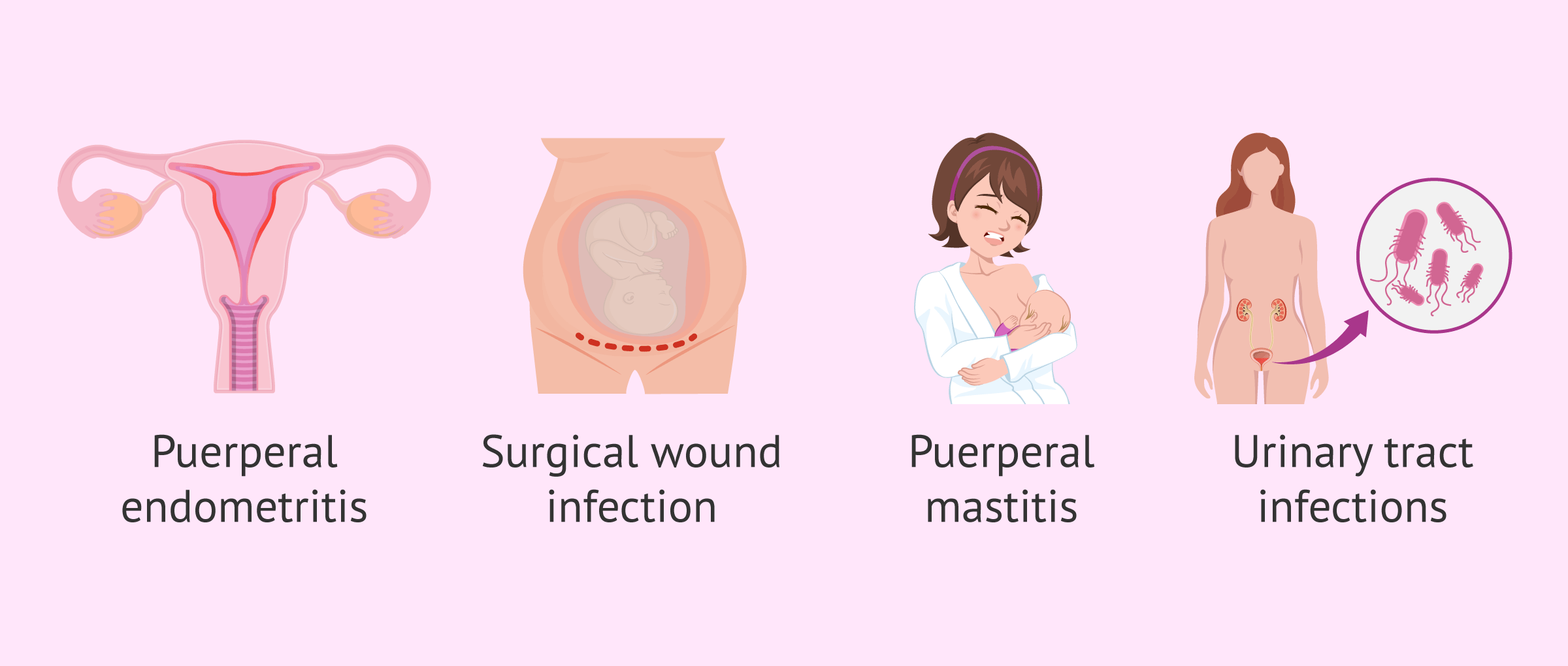
- Puerperal endometritis
- is a bacterial infection found inside the uterus, specifically in the endometrium, where the placenta has been anchored during the 9 months of gestation. In addition to fever, she usually presents with lower abdominal pain, enlarged and painful uterus, continued bleeding and foul-smelling discharge (lochia). Only 15% of the cases are late, debuting from the first week postpartum.
- Surgical wound infection
- either by episiotomy in vaginal delivery or by the abdominal incision of a cesarean section. In general, it occurs in approximately 5% of deliveries, debuting in the first 7 days after surgery. The microorganisms causing the infection usually come from the skin, such as Staphylococcus Aureus. It is very important to take good care of these wounds to prevent the risk of infection.
- Puerperal Mastitis
- consists of a breast infection due to lactation. The source of infection comes from microorganisms in the infant's mouth or pharynx (streptococci and anaerobes) and less frequently from the skin(Staphylococcus Aureus), so broad antibiotic treatment is necessary. It usually begins 2-3 weeks after the onset of lactation, with a frequency of 2-10% of breastfeeding mothers.
- Urinary infections
- generally due to the multiple catheterizations performed during labor associated with the epidural. They are caused by genital tract bacteria such as Staphylococcus Aureus or Escherichia coli. They appear in the first postpartum days (2-5 days).
- Other systemic infections
- pyelonephritis, cystitis, thrombophlebitis, etc.
As we have already indicated, the most frequent microorganisms causing puerperal fever are those found in the vaginal flora, on the skin or in the intestinal flora: Streptococcus agalactiae, Streptococcus pyogenes, Staphylococcus Aureus, Escherichia coli, etc.
Risk Factors
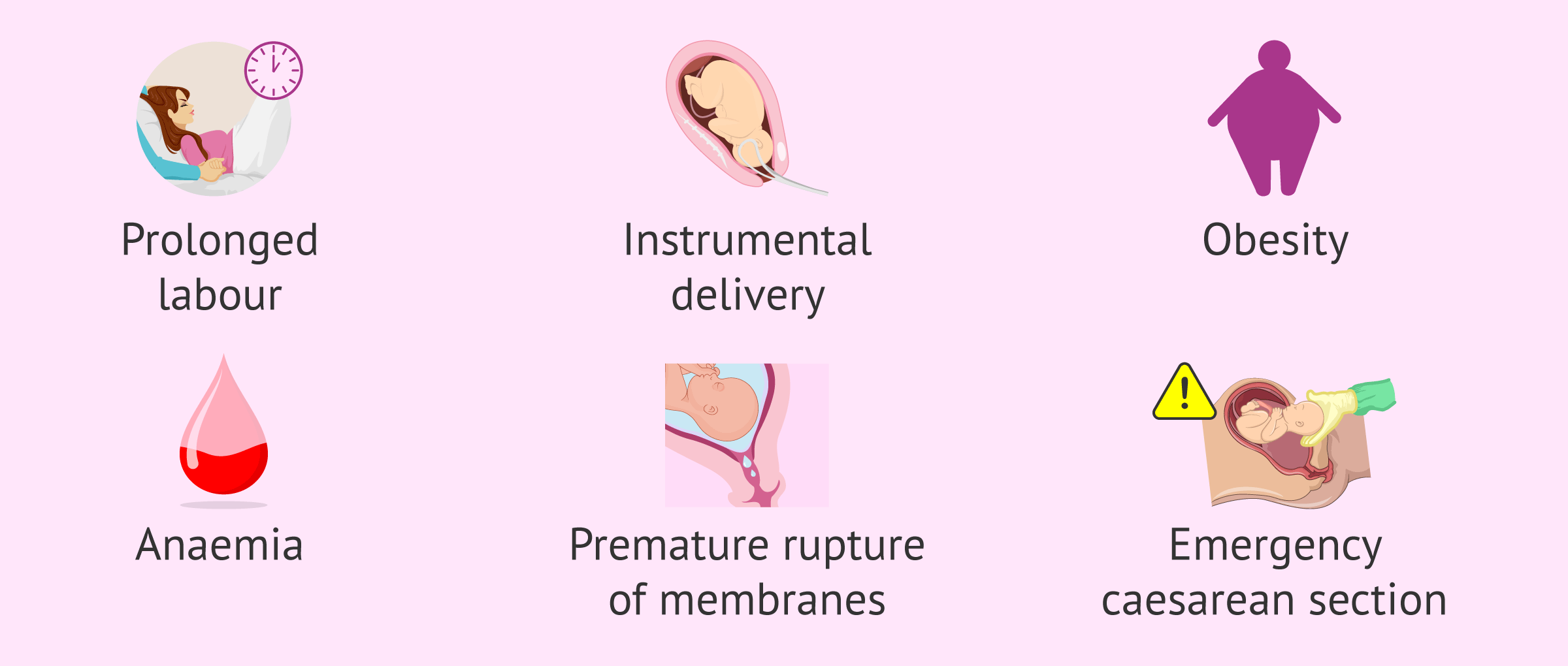
Risk factors that predispose a woman to infection after childbirth may be intrinsic (related to the woman's medical history) or extrinsic (related to the health care personnel and instruments used during delivery).
These are as follows:
- Prolonged labor
- Instrumental delivery
- Woman with a history of urinary tract or vaginal infections
- Obesity
- Anemia or malnutrition
- Premature rupture of membrane
- Manual removal of placenta
- Emergency cesarean section
- Sexual intercourse in the days prior to delivery
It should be noted that not all women with any of these conditions will have a puerperal infection. In order to prevent it, it will be necessary to take extreme hygienic care of the intimate area during pregnancy and after childbirth.
Treatment
Treatment of puerperal sepsis should always be carried out under medical supervision.
In general, antipyretics and analgesics are prescribed to reduce fever and pain.
The administration of antibiotics is then essential to act on the infectious microorganisms. If the specific causative agent is unknown, a broad-spectrum antibiotic such as amoxicillin will be used.
Depending on the results of the cultures and the antibiogram, the antibiotic may be modified to cure the infection.
On the other hand, it is essential to maintain good intimate hygiene throughout the postpartum period.
It is best to wash and disinfect the external genitalia at least 2 or 3 times a day. The most severe cases of puerperal infection require hospitalization of the woman.Therefore, if the symptoms mentioned in this article appear, it is advisable to go to the emergency room as soon as possible.
FAQs from users
Is puerperal fever serious?
Puerperal fever is defined as the presence of a temperature higher than 38ºC from 24 hours after delivery until six weeks later.
In most cases, these infectious processes are limited by the use of antibiotics (in the order of 7-10 days) that limit the situation. In some cases it is necessary to complete the treatment surgically, as in the case of mastitis with an aspiration curettage, or with the drainage of the surgical wound of the cesarean section or the drainage of a breast abscess in the case of mastitis.
Is puerperal fever the same as puerperal infection?
Usually, both concepts are used synonymously, although it would be more correct to use the terms puerperal infection or sepsis to refer to this condition in women, since puerperal fever is a sign of infection that only refers to the increase in temperature.
What nursing care does puerperal sepsis require?
After delivery and especially in the event of puerperal infection, it is very important to wash and disinfect the episiotomy or cesarean section wound, as the case may be. Soap should not be applied directly to this area. It is best to use a solution of pharmaceutical disinfectant and pour it over the area. The wound should then be dried with a clean cloth and covered with a new sterile dressing.
Suggested for you
We have said that puerperal infection can be a consequence of some complications at the time of delivery. If you want to know this procedure in detail, we recommend you to continue reading here: Childbirth: preparation, types and possible complications.
Puerperal mastitis usually appears 2-3 weeks after the onset of lactation. If you are interested in learning more about how to breastfeed your baby and some of the advantages, you can click here: Breastfeeding: What Is the Best Method For My Baby?
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
CHRISTINE HALLETT. The Attempt to Understand Puerperal Fever in the Eighteenth and Early Nineteenth Centuries: The Influence of Inflammation Theory. Med Hist. 2005 Jan 1; 49(1): 1–28 (View)
E Barrajón, C Khouri. J. Sánchez, JJ. Escribano Tórtola. Fiebre… ¿puerperal? Rev. chil. obstet. ginecol. vol.84 no.5 Santiago oct. 2019 (View)
Marina Boushra, Omar Rahman. Postpartum Infection. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan.2023 Jul 10 (View)
Susannah L Woodd, Ana Montoya, Maria Barreix, Li Pi, Clara Calvert, Andrea M Rehman, Doris Chou, Oona M R Campbell. Incidence of maternal peripartum infection: A systematic review and meta-analysis (View)
FAQs from users: 'Is puerperal fever serious?', 'Is puerperal fever the same as puerperal infection?' and 'What nursing care does puerperal sepsis require?'.
Authors and contributors