One of the stages of in vitro fertilization (IVF) treatment is the evaluation of the quality of embryos in the laboratory.
Not all embryos generated are suitable for transfer or vitrification, as their viability may be compromised. Therefore, it is necessary to follow morphological criteria that help specialists in the choice of embryos of optimal quality.
The main purpose of embryo selection is to identify the embryo with the greatest possible implantation capacity to be transferred to the uterus of the mother-to-be.
Provided below is an index with the 7 points we are going to expand on in this article.
- 1.
- 2.
- 2.1.
- 2.2.
- 2.3.
- 2.4.
- 3.
- 4.
- 4.1.
- 4.2.
- 4.3.
- 4.4.
- 4.5.
- 4.6.
- 5.
- 6.
- 7.
Parameters of embryo quality
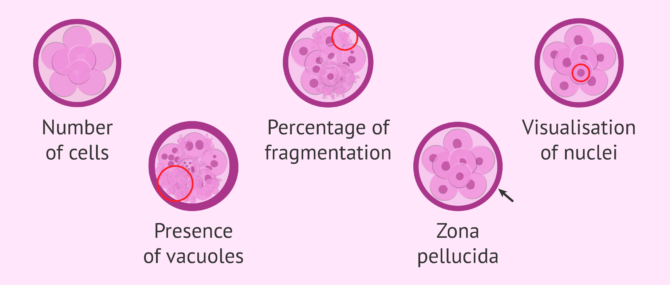
In order to determine which embryos are of good quality during their development in culture, the parameters set by ASEBIR (Association for the Study of Reproductive Biology) are taken into account. These are as follows:
- Number of cells or blastomeres and division rate
- Percentage and type of cell fragmentation
- Symmetry: size of blastomers according to stage
- Visualization of nuclei and multinucleation (more than one nucleus per cell)
- Presence of cytoplasmic halo or vacuoles in the cytoplasm
- Zona Pellucida(ZP)
- Compaction degree
These parameters are routinely checked visually under the microscope on the second and third day of embryonic development (day 2 and day 3, respectively).
This is what embryologist Edurne Martínez says on this matter:
There are criteria that help us select embryos. For the most part, these criteria are morphokinetic, which means that we have to check that they are dividing at the time they have to divide and in the number of cells that have to divide.
Day 3 embryo classification
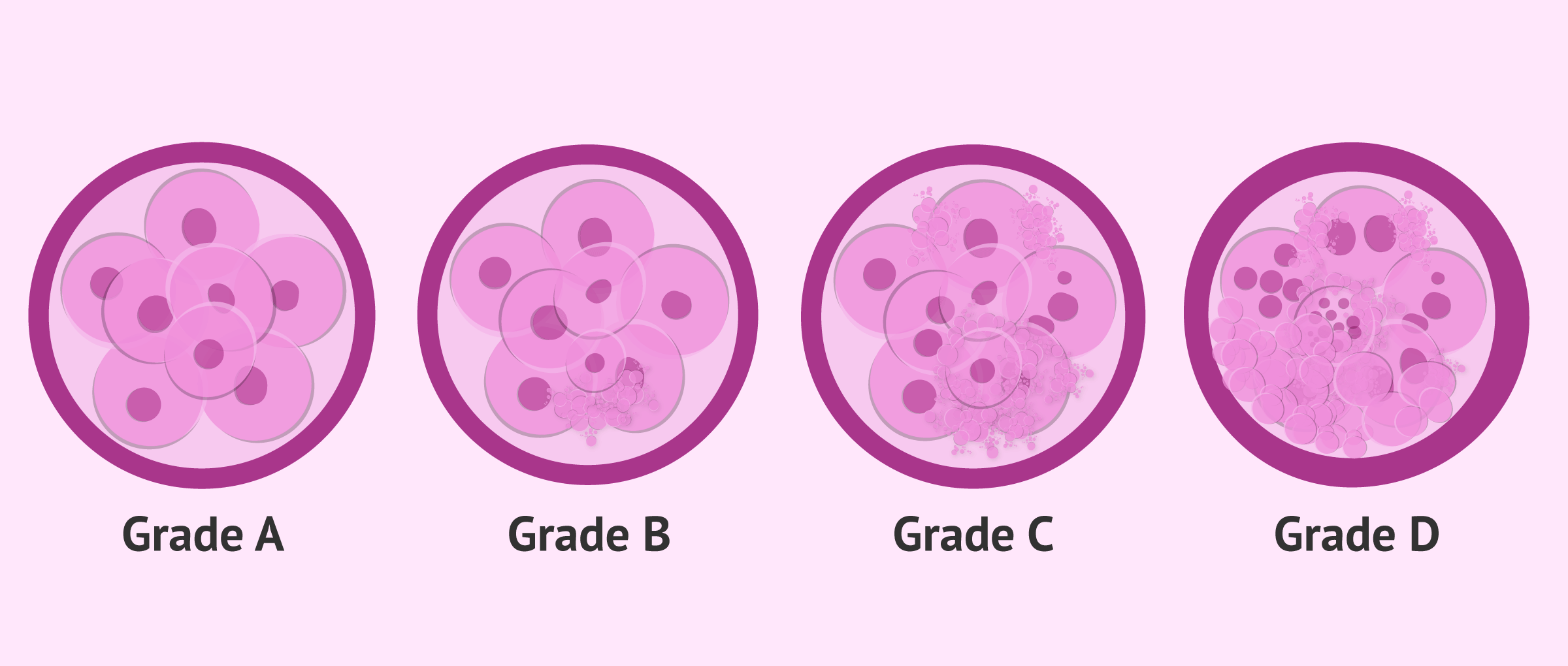
Embryologists classify embryos into different grades or categories according to the parameters observed, so that A grade embryos are of the highest quality and D grade embryos are of the lowest quality.
The most common characteristics of each grade of embryo quality are detailed below.
Grade A
It corresponds to an embryo of excellent quality with maximum implantation capacity. Its morphological characteristics are as follows:
- Number of cells: 4 on DAY 2 or 7-8 on DAY 3
- There is symmetry: blastomeres of equal size.
- No fragmentation or it’s less than 10%
- There are no multinucleated blastomeres
- Smooth texture and light color
- Normal zona pellucida
Early compaction on DAY 3 is also considered a good prognostic factor, although there are specialists who prefer not to take it into account for classification.
Grade B
The quality of the embryo is still good, having implantation capacity. Its morphological characteristics are as follows:
- Quantity of cells: 4-5 on DAY 2 or 7-10 on DAY 3
- Slight asymmetry between blastomeres
- Fragmentation between 10% and 25%
- There are no multinucleated blastomeres
- Small vacuoles in the middle of the blastomeres
- Abnormal zona pellucida
The alterations in the ZP can be several, such as pigmented or thickened ZP. In this case, assisted hatching is considered prior to embryo transfer. You can find out what this technique is by clicking on the link: What is Assisted Hatching?
Grade C
The embryo is considered regular, of intermediate quality, with a lower probability of implantation. Its morphological characteristics are as follows:
- Quantity of cells: 2 or 6 blastomeres on DAY 2, or 6 or 12 blastomeres on DAY 3
- Asymmetrical blastomers
- Fragmentation between 25% and 35%
- 1 or 2 multinucleated blastomers
- Large vacuoles in the middle of the blastomeres
- Rough appearance
- Abnormal zona pellucida
It should be noted that the assignment of category to the embryo is made according to its most negative characteristic. Therefore, if the embryo has multinuclear cells even though it has good morphological parameters, he is assigned a grade C.
Grade D
The quality of the embryo is poor, with a low probability of implantation. Its morphological characteristics are as follows:
- Quantity of cells: 3 or 6 blastomeres on DAY 2, or 6 or 12 blastomeres on DAY 3
- Very asymmetrical blastomers
- Fragmentation above 35%
- 1 or 2 multinucleated blastomers
- Large vacuoles in the middle of the blastomeres
- Large cytoplasmic alterations: dark color and rough appearance
- Abnormal zona pellucida
Within this category there are several anomalies that make the probability of implantation very low. Moreover, embryos with faster or slower than normal division do not have a good prognosis, either. They tend to be at greater risk for genetic abnormalities, such as aneuploidy, so they are not normally transferred or frozen.
Which embryos are transferred and which are not?
All degrees of embryo quality are likely to be implanted, but the decision as to which embryos are transferred is ultimately made by the physician and embryologist as a whole, valuing the couple's entire medical history. It must be remembered that the possibility of pregnancy also depends on the age of the woman and the state of her uterus, not only on the embryonic quality.
Whenever possible, the quality of the embryos transferred shall be grade A or B. These are embryos of good quality and will therefore also be frozen if not transferred.
Grade C embryos have a regular quality, although they are able implant and lead to pregnancy. The decision to transfer these embryos is made when there is none of grade A or B. In general, C-grade embryos are vitrified for future embryo transfers.
Grade 4 or grade D embryos have a worse prognosis: in most cases they are discarded and not transferred. They are left in culture and their evolution up to blastocyst is observed.
Virtually all of these embryos stop developing, so it is believed that they would not have survived in the mother's womb either. If the division rhythm is recovered and the morphological characteristics are good, they can be vitrified at the blastocyst stage.
FAQs from users
What causes poor quality embryos?
This is a very common question but not an easy answer. First, the term “quality” is not well defined in reproductive medicine: is it based on appearance of the embryo?; is it the chromosomal competence of the embryo; or the structrual/genetic make-up? The first two metrics are definable – we can grade an embryo base on appearance; we can test the embryo for the chromosomal content. Neither of these qualifiers correlate well with the ability for the embryo to result in a live birth. Structural/genetic make-up is not able to be tested at this time.
Traditionally, we have considered a woman’s age as the dominant forcé contributing to egg “quality.” The percentage of chromosomally abnormal embryos increase as the woman ages. While male fertility declines with age, we do not have as much information on their contributions to embryo quality.
Can you pregnant with C and D scored embryos?
Yes, although the chances are quite low.
When we classify embryos according to their quality at the lab, we do so by evaluating their implantation potential, that is, trying to "guess" which ones have greater chances for attaching tot he uterus, and which don't. C and D scored embryos are embryos of moderate-to-low quality, which means that a C or D scored embryo has a reduced chance of implantation if compared to a B or A scored embryo. In any case, however, whenever we select an embryo for the transfer, it's because it has been observed that its implantation potential is a good one.

What is the usual quality of frozen embryos?
The quality of the embryos is the same at the moment of freezing as once thawed, that is to say, they present the same morphological characteristics. What can happen is that, when they continue their development after a few hours, these may change. For example, compaction, multinucleation, fragmentation, etc., may appear, so the embryo would have to be assigned another category.
What is the quality of embryos after ICSI?
In general, the quality of the embryos is the same after IVF or ICSI. It depends more on the quality of the egg than on the technique used for in vitro fertilisation.
What is the quality of egg donation embryos?
Embryos obtained from an egg donation programme come from the eggs of a young, healthy woman, so the vast majority will be grade A or B embryos with a high probability of implantation. There is also the possibility of some grade C embryos.
What is a grade 2 blastocyst?
A grade 2 blastocyst, also called cavitated blastocyst (CB) is that embryo on day 5 in which it is possible to differentiate the trophectoderm and the inner cell mass (ICM). Therefore, in this type of blastocyst, each of the parts that form it is perfectly differentiated.
Suggested for you
If you want to continue reading about embryo quality, consult the link Classification of embryos, where you will also find the criteria used for the evaluation of blastocyst stage embryos. To learn more about how and when embryo transfer takes place, read on here: What happens in embryo transfer?
In the following post you will find the criteria used to decide the number of embryos to be transferred in each IVF cycle: How many embryos must be transferred?
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
Mantikou E, Youssef MA, van Wely M, van der Veen F, Al-Inany HG, Repping S, et al. Embryo culture media and IVF/ICSI success rates: a systematic review. Hum Reprod Update 2013;19:210–20 (View)
Mauri AL, Petersen CG, Baruffi RL, Franco JG Jr. A prospective, randomized comparison of two commercial media for ICSI and embryo culture. J Assist Reprod Genet 2001;18:378–81 (View)
Parinaud J, Veiga A, Vieitez G, Busquets A, Milhet P, Calderon G, et al. Randomized comparison of three media used for embryo culture after intracytoplasmic sperm injection. Hum Reprod 1998;13(Suppl 4):212–7 (View)
Paternot G, Debrock S, D’Hooghe TM, Spiessens C. Early embryo development in a sequential versus single medium: a randomized study. Reprod Biol Endocrinol 2010;8:83.
Pool TB, Schoolfield J, Han D. Human embryo culture media comparisons. Methods Mol Biol 2012;912:367–86 (View)
Pool TB. Development of culture media for human assisted reproductive technology. Fertil Steril 2004;81:287–9 (View)
Quinn P. Culture systems: sequential. Methods Mol Biol 2012;912: 211–30. Sepulveda S, Garcia J, Arriaga E, Diaz J, Noriega-Portella L, Noriega-Hoces L. In vitro development and pregnancy outcomes for human embryos cultured in either a single medium or in a sequential media system. Fertil Steril 2009;91:1765–70 (View)
Summers MC, Bird S, Mirzai FM, Thornhill A, Biggers JD. Human preimplantation embryo development in vitro: a morphological assessment of sibling zygotes cultured in a single medium or in sequential media. Hum Fertil (Camb) 2013;16:278–85 (View)
Swain JE. Decisions for the IVF laboratory: comparative analysis of embryo culture incubators. Reprod Biomed Online 2014;28:535–47 (View)
Swain JE. Is there an optimal pH for culture media used in clinical IVF? Hum Reprod Update 2012;18:333–9 (View)
Van Langendonckt A, Demylle D, Wyns C, Nisolle M, Donnez J. Comparison of G1.2/G2.2 and Sydney IVF cleavage/blastocyst sequential media for the culture of human embryos: a prospective, randomized, comparative study. Fertil Steril 2001;76:1023–31 (View)
Zollner KP, Zollner U, Schneider M, Dietl J, Steck T. Comparison of two media for sequential culture after IVF and ICSI shows no differences in pregnancy rates: a randomized trial. Med Sci Monitor 2004;10:CR1–7 (View)
FAQs from users: 'What causes poor quality embryos?', 'Can you pregnant with C and D scored embryos?', 'What is the usual quality of frozen embryos?', 'What is the quality of embryos after ICSI?', 'What is the quality of egg donation embryos?' and 'What is a grade 2 blastocyst?'.











I recently had a DE-IVF cycle in the Czech Republic. We ended up with two Grade 1 embryos, and one Grade 3 embryo. We transferred one of the Grade 1 embryos, and froze the other two. What do you think our chances are with the Grade 3? We will likely transfer both frozen embryos when we go back.