The transfer of frozen embryos (FET), known as delayed embryo transfer, consists of using the embryos created in a previous cycle of in vitro fertilisation (IVF) that were frozen at the time through the process of embryo vitrification.
For this, it is only necessary to prepare the woman's endometrium so that it is receptive to the implantation of the embryo.
One of the main fears of transferring previously vitrified embryos is the success rate. However, the probability of pregnancy is practically the same as when using fresh embryos.
Provided below is an index with the 10 points we are going to expand on in this article.
- 1.
- 2.
- 2.1.
- 2.2.
- 2.3.
- 3.
- 4.
- 5.
- 6.
- 6.1.
- 6.2.
- 6.3.
- 7.
- 7.1.
- 7.2.
- 7.3.
- 7.4.
- 7.5.
- 7.6.
- 8.
- 9.
- 10.
What is a FET?
In fresh IVF cycles, the intended mother's ovaries are stimulated artificially in order to produce a higher number of mature eggs. Then, they are retrieved through a procedure called follicular puncture or ovum pick-up (OPU), and finally they are fertilized in the lab using the husband's sperm or donated sperm.
After 3-5 days, the resulting embryo(s) are transferred back to the IM's uterus. The remaining viable embryos that have not been used, referred to as spare, surplus or unused embryos, are cryopreserved in liquid nitrogen at -196 °C until a decision about their fate is made.
There exist 4 possible options as regards their fate:
- Cryopreservation for later use
- Donation to other women or couples. This option is possible only if certain requirements are met (e.g. being 35 or younger)
- Donation for stem cell research
- Destruction
Both the first and the second options lead to the same thing, that is, a Frozen Embryo Transfer. In both cases, cryopreservation is used for reproductive purposes.
FET step by step
An IVF-FET cycle involves just two steps. Simply put, it works as if a conventional IVF cycle was split into two major parts. On the one hand, creating the embryos (ovarian stimulation, egg retrieval, and fertilization), and on the other, endometrial preparation and embryo transfer.
The parties involved in each party can be the same from beginning to end, or be different, as in the case of embryo donation cycles. Learn more: What is Embryo Donation & Adoption?
In any case, the patient who is undergoing the second part should prepare her endometrial lining adequately to increase the chances for embryo implantation, thereby increasing the likelihood of getting pregnant.
The protocol to follow in FET cycles is more comfortable and simpler than in conventional cycles. Daily injections or regular monitoring is unnecessary, and the same happens with surgical procedures or uncomfortable side effects.
The following are the main steps:
Endometrial preparation
Firstly, the IM takes GnRH analogs to block the natural regulation of hormones, and control her cycle artificially. This can be achieved using oral contraceptives as well.
Then, the medical treatment to follow includes administering estrogens orally or in patches. Additionally, about 3-5 days before the transfer, she has to take progesterone (pills or vaginal pessaries).
These medications should be taken from the first or third day of menstruation, that is, at the beginning of the cycle, until the day of the embryo transfer (in total, 10-15 days in a row). During this time period, you will have to visit your doctor to check your endometrium via ultrasound once or twice.
When the endometrial is receptive, that is, it has a triple line pattern and its thickness ranges between 7 and 10 mm, the transfer day is scheduled, and a protocol for the intake of progesterone is established.
Embryo thawing
When the embryo transfer day is set, the embryos are thawed considering the day when they were transferred. Simply put, if they were frozen on day 3 of development and you want to transfer them on day 3, they will be thawed on the transfer day. If you want to transfer them on day 5 but they were frozen on day 3, they will be thawed two days before the transfer, and cultured in the meanwhile to monitor their development.
Checking their growth between the thawing and the transfer days can be beneficial when it comes to choosing the best embryo to transfer.
Embryo transfer
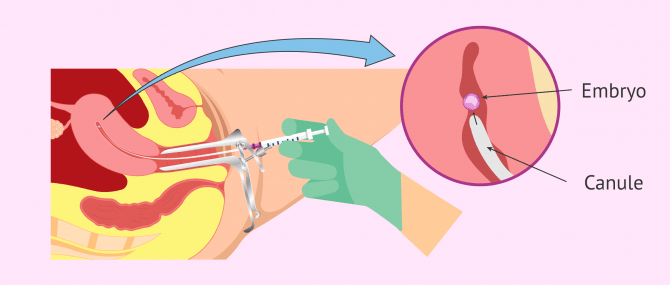
The transfer is actually a quick, simple, and painless procedure that is usually done at the doctor's office or surgery room. In fact, anesthesia is not required.
Your gynecologist uses a cannula that contains the embryo(s) to transfer. He or she inserts it gently in your uterus while you are in the lithotomy position.
When he or she reaches the uterine fundus, taking care not to damage the walls of the uterus, the embryos are placed in the uterine cavity. It is an ultrasound-guided procedure, which means you can follow the pathway of the cannula from beginning to end of the process.
Finally, you will have to lie flat on the stretcher for about 10-15 minutes. After this rest time, you can continue with your normal lifestyle, but avoiding major physical efforts.
Please note that you cannot use make-up or perfumes on the transfer day. Moreover, you should have a full bladder, which makes it easier for everyone to see your uterus via ultrasound scan.
Natural vs. stimulated cycle
The treatment explained above refers to what we usually know as stimulated IVF cycle.
The reason for this name is due to the fact that we are stimulating or replacing the natural menstrual cycle of the woman using artificial hormones, including GnRH analogs, estrogen, and progesterone. By doing this, we simulate the behavior of a natural cycle but controlling it to enhance the chances of pregnancy.
A frozen embryo transfer can be done in a natural cycle, though. In this case, we take advantage of the natural endometrial growth that occurs in women monthly.
In natural cycles, the ovulation cycle of the patient is examined via ultrasound in order to make it coincide with the IVF procedure. Thus, if we have a day-3 frozen embryo, it will be transferred back three days after ovulation.
Once the embryo has been transferred, the woman must continue administering progesterone pessaries to maintain her endometrial lining in an optimal state.
As one shall see, the difference between both transfer protocols is the way in which endometrial growth is triggered by using the natural estrogens released from the ovary, or by blocking this natural release and administering them artificially.
Get more info by clicking the following link: Natural Cycle of Embryo Transfer.
Success rates
The chances of getting pregnant after a FET depend highly on the quality of embryos after going through the thawing process, and the particularities of the IM's uterus.
The embryo vitrification technique reaches high survival rates. Thus, individualizing the endometrial preparation protocol on a case-by-case patient and keeping a close eye on how the uterine lining progresses is crucial.
In any case, although the success rates of delayed embryo transfer are high, they are generally somewhat lower than the rates obtained in an IVF cycle with fresh transfer.
In the case of women or couples who had a child after their previous cycle, the chances for them to get pregnant in a second cycle using their unused embryos is high, as the fact that they led to a pregnancy the first time confirms. However, as indicated above, it may vary with time and is subject to the survival potential of the embryos.
Advantages of using frozen embryos
According to Dr. Gorka Barrenetxea, Obstetrician & Gynecologist, there is a huge difference between conventional embryo freezing procedures and embryo vitrification. With the latter, the risk of late Ovarian Hyperstimulation Syndrome (OHSS) decreases, which is a major advantage.
Also, in the word of Dr. Barrenetxea, the success rates with frozen embryos are actually higher. The reason for this increased rates may be due to better preparation of the endometrium, since it is not so overstimulated, and also because the levels of progesterone are not so high as in fresh cycles.
Finally, as regards the question if the transfer with frozen embryos should be done on day 3 or day 5, embryologist Edurne Martínez states that it is actually a controversial question. However, she is in favor of sequential culture as long as possible and provided that the conditions of the lab are adequate for it.
Cost
The cost of embryo thawing for use in a FET cycle is cheaper than a complete IVF cycle, given that there is no need for the patient to undergo ovarian stimulation and in vitro fertilization again. The cost, however, varies from clinic to clinic.
IVF with frozen embryos, as any other reproductive technology, requires that you rely on the professionalism of the doctors and staff of the clinic you choose. Obviously, each clinic is different. Our Fertility Report selects several clinics for you out of the pool of clinics that meet our strict quality criteria. Moreover, it will offer you a comparison between the fees and conditions each clinic offers in order for you to make a well informed choice.
Cost in the USA
In the United States, the overall cost of a Frozen Embryo Transfer is about $3,000-$5,000, and it typically includes the cost of monitoring, embryology fees, embryo thaw, and finally embryo transfer. Yearly storage fees range between $200 and $800 on average.
Cost in the UK
In the United Kingdom, the average fee for a FET is £1,400, and the cost of medications usually starts from £200.
Cost in Canada
A Frozen Embryo Transfer in Canada may cost about $1,500 Canadian dollars. Clinics typically exclude embryology fees, which can add up to $1,000 on average.
FAQs from users
How many frozen embryo transfers can be made in a row?
There is no limit, it depends on the number of the vitrified embryos available.
Can I have Ovarian Hyperstimulation Syndrome in a frozen embryo cycle?
No, it's not possible. Embryo cryotransfer is performed in an asynchronous cycle not stimulated with gonadotropins. It can be done with natural cycle in women with very regular periods or with cycles substituted with female hormones.
In case of a substituted cycle, the treatment consists of the administration of an estrogen in the first phase and the association of an estrogen and progesterone in the second phase. Both substances prepare the endometrium for implantation, but have no effect on follicular growth or ovulation. In fact, during a substituted cycle the ovary is slowed down by the effect of the hormones.
My fresh transfer has been cancelled, does the pregnancy rate drop with frozen embryos?
Nowadays, if you have a good embryology laboratory, gestation rates with thawed embryos are practically the same as with fresh embryos. There are even studies that recommend frozen transfer because the excess of medication administered during stimulation can cause a hormonal environment that is not as suitable for implantation, affecting the receptivity of the endometrium for the embryo.
When can I take a pregnancy test after a FET?
Beta-hCG testing to find out whether pregnancy has occurred or not after a Frozen Embryo Transfer can be done within 15 days approximately, which allows you to get more accurate results. If done early, the test may give you a false negative or false positive result back.
There are cases, for example when blastocyst (day 5-6 of development) embryos are used, when the test can be done as early as 10 days after the FET. In any case, the general recommendation is to wait two weeks to take a pregnancy test.
Is there any difference between a FET with donated embryos than with unused embryos from previous cycles?
Absolutely yes, the process is exactly the same. The embryos are thawed and transferred to the woman's uterus (womb). The origin of the embryos does not change the steps involved in the procedure.
When is a FET recommended?
A FET is indicated in multiple situations, including:
- Embryo donation and adoption
- Women or couples who have had children in the past, and want to have a second child using the cryopreserved embryos from previos cycles
- Women or couples who want to try again after a failed IVF cycle
- In case of cancellation of a transfer with fresh embryos due to various reasons, including inadequate endometrial preparation, waiting for the results of PGD (preimplantation genetic diagnosis), etc.
- Women or couples with recurrent implantation failure using fresh embryos, when the suspected cause has an endometrial origin.
There exist some studies indicating that FETs improve the implantation chances, as no medications for ovarian stimulation are needed. They suggest that stimulated cycles can alter the quality of the endometrial lining, thereby affecting the embryos' implantation potential.
Suggested for you
When talking about the protocol followed with frozen embryos, we have indicated that the transfer step is exactly the same as with fresh embryos. Get more info: IVF Embryo Transfer Procedure – Definition, Process & Tips.
Also, we have also mentioned that embryos can be transferred either on day 3 or on day 5. The decision will depend on a series of factors, though. Want to delve deeper into it? Click here: Day 5 vs. Day 3 Embryo Transfer - What Are the Pros & Cons?
Last but not least, we recommend that you have a look at the following guide with tips and recommendations for the post-transfer days. Although you can continue with your normal lifestyle, it is important that you learn how to deal with the common symptoms: Post Embryo Transfer Tips & Precautions – What Should You Expect?
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
Bjuresten K, Landgren BM, Hovatta O, Stavreus-Evers A. Luteal phase progesterone increases live birth rate after frozen embryo transfer. Fertil Steril 2011;95:534–7.
Eftekhar M, Rahsepar M, Rahmani E. Effect of progesterone supplementation on natural frozen-thawed embryo transfer cycles: a randomized controlled trial. Int J Fertil Steril 2013;7:13–20.
Glujovsky D, Pesce R, Fiszbajn, G, Sueldo C, Hart RJ, Ciapponi A. Endometrial preparation for women undergoing embryo transfer with frozen embryos or embryos derived from donor oocytes. Cochrane Gynaecology and Fertility Group 2010.
Groenewoud ER, Cantineau AE, Kollen BJ, Macklon NS, Cohlen BJ. What is the optimal means of preparing the endometrium in frozen-thawed embryo transfer cycles? A systematic review and meta-analysis. Hum Reprod Update 2013;19:458–70.
Mounce G, McVeigh E, Turner K, Child TJ. Randomized, controlled pilot trial of natural versus hormone replacement therapy cycles in frozen embryo replacement in vitro fertilization. Fertil Steril 2015;104:915–20.e1.
Ortega I, Garcia Velasco JA. Progesterone supplementation in the frozen embryo transfer cycle. Curr Opin Obstet Gynecol 2015;27:253–7
Reproducción Asistida ORG. Original video: Transferencia de embriones congelados (Frozen Embryo Transfer), by Dr. Gorka Barrenetxea and Edurne Martínez Sanz. [See original video in Spanish].
Robert F, Casper MD, Elena H, Yanushpolsky MD. Optimal endometrial preparation for frozen embryo transfer cycles: window of implantation and progesterone support. Fertil Steril 2016;105:867–72.
Tomás C, Tikkinen K, Tuomivaara L, Tapanainen JS, Martikainen H. (2002). The degree of difficulty of embryo transfer is an independent factor for predicting pregnancy. Hum Reprod; 17:2632–5.
William B. Schoolcraft, M.D., for the ASRM American Society for Reproductive Medicine (April 2016). Importance of embryo transfer technique in maximizing assisted reproductive outcomes. Vol. 105, No. 4. Colorado Center for Reproductive Medicine, Lone Tree, Colorado.
FAQs from users: 'How many frozen embryo transfers can be made in a row?', 'Can I have Ovarian Hyperstimulation Syndrome in a frozen embryo cycle?', 'My fresh transfer has been cancelled, does the pregnancy rate drop with frozen embryos?', 'When can I take a pregnancy test after a FET?', 'Is there any difference between a FET with donated embryos than with unused embryos from previous cycles?' and 'When is a FET recommended?'.
Authors and contributors














Hello, we are blessed that almost 4 years ago we did IVF, everything went well and I have a little girl of three and a half years. My question is that I am almost 40 years old, we would like to try again next year, we have frozen embryos but I am anxious to see if nothing will happen to them because of my age and the embryos are 4 years old, is there anything wrong with that? Thank you.
Don’t worry about it. The fact that your embryos are frozen for 4 years makes them the same quality as when you were 36. For them, time has not passed and, therefore, they can have a better implantation rate than the embryos you can get now. Besides, freezing hardly affects their viability.
I wish you the best of luck.
Regards
Hello, on May 18 I had the frozen embryo transfer, the midwife left me with the same medications, primaquin 2mg and I am progining 400 mg via the vagina, they told me I had to go on June 1 for the beta test. Before I went for the test, I had run out of the progestogen. I thought I would have to use it until I ran out. I stopped using it for about 4 days, when I went to take the beta test I told the midwife, she told me I didn’t have to stop using it, I got more and I put it on, that day I stained a little brown after putting it on, the next day I had blood, the third day I had more blood and I started throwing clots about 5 times in high quantity and I had a lot of pain in my ovaries. I started taking viadil for the pain, it calmed down but I keep bleeding and stop, I called the midwife, she told me absolute rest and tomorrow they are going to do the pregnancy test again, I am very worried, I hope for some answer, thank you.
Good evening,
on June 16, 2018, I had my puncture. Today I have been assured that there are 2 high-quality embryos. Last week, I was told that in this cycle they could not do the transfer as I have very high estrogen levels and there is no optimal environment for pregnancy. I have an appointment for July 13, 2018. My next period is on June 9, 2017. Will I be able to have the transfer in my next cycle and is there anything I can do to help lower my estrogen? Thank you very much and good luck to you all!
Hi Misty
Don’t worry about it. In the next cycle you will be given the right hormonal medication to prepare the endometrium and to be able to make the transfer in optimal conditions.
I wish you all the best.