It is very common for couples starting assisted reproduction treatment to have doubts about whether having sexual intercourse during treatment can affect the outcome of the treatment in any way.
What is certain is that there may be a variety of opinions among assisted reproduction specialists as to whether sexual intercourse near embryo transfer has advantages or disadvantages in the outcome of fertility treatment.
Provided below is an index with the 6 points we are going to expand on in this article.
- 1.
- 1.1.
- 1.2.
- 1.3.
- 2.
- 3.
- 3.1.
- 3.2.
- 3.3.
- 3.4.
- 3.5.
- 4.
- 5.
- 6.
Sexual intercourse and embryo transfer
A common question when undergoing fertility treatment is whether or not the couple can have sexual intercourse.
Therefore, we are going to talk about the possible disadvantages and possible benefits of having sexual intercourse close to the time of the embryo transfer.
Possible disadvantages
In principle, it is possible to think that uterine contractions from intercourse and orgasm may affect implantation. However, this is not always the case. Couples seeking pregnancy naturally can have sex after conceiving, without knowing it, and it does not seem to affect the achievement of pregnancy.
However, it is recommended not to have sexual intercourse from before the ovarian puncture and up to one week after the embryo transfer. Some specialists advise abstinence until the pregnancy test.
The reason for this recommendation, rather than affecting the outcome of the cycle, is the increase in size of the ovaries with ovarian stimulation. This can make sexual intercourse painful and also increases the risk of complications such as ovarian torsion.
Ovarian torsion is a complication that can arise because the ovary turns and rotates its position. This makes it difficult for blood to enter the ovary and requires emergency surgery to resolve the situation.
In addition, in an assisted reproduction treatment that has not required ovarian stimulation (frozen embryo transfer, embryoadoption, ovodonation), it is also recommended to wait 2-3 days before having sexual intercourse after the transfer. In this case, the explanation is that the transfer has damaged the cervical mucus barrier to the entry of microorganisms into the uterus. Therefore, there could be an increased risk of infection with sexual intercourse.
On the other hand, the risk of multiple pregnancy may also be increased if sexual intercourse takes place during assisted reproduction treatment.
Finally, another potential drawback is that, if the IVF result is negative, the couple may feel guilty. In this situation, it is common to look for any specific event that may have led to the undesirable outcome.
Potential benefits
Despite the above, some studies show that sexual intercourse during an IVF cycle may be beneficial. This benefit could be attributed to the fact that the presence of seminal plasma in the female reproductive tractor could favor embryo development and implantation.
One of the possible reasons is that the presence of certain substances in the seminal plasma could favor maternal immunological tolerance towards the embryo (which only shares half of its genetic material and requires this tolerance to avoid an adverse maternal immune response).
Thus, some argue that sexual intercourse in the days leading up to embryo transfer may improve the likelihood of successful implantation and early embryo development.
However, more research is needed. However, in the case of sexual intercourse, it must be taken into account that the time of ejaculatory abstinence (2-5 days) must be respected before submitting the seminal sample for IVF. Thus, the seminal quality of the sample is intended to be optimal, as this could be affected by higher or lower abstinence.
General recommendations
Generally, it is recommended that the couple abstain from sexual intercourse before and after the embryo transfer. The possible risks, the lack of solid scientific evidence to support its benefits, and the possible guilt that the couple may feel in the event of a negative outcome, make avoiding sexual intercourse during assisted reproduction treatment the most common option.
Sexual intercourse during pregnancy
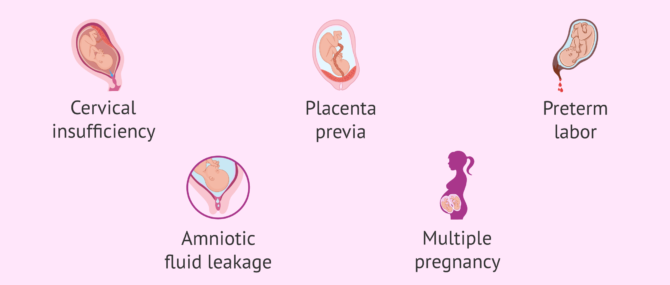
During pregnancy, sexual intercourse is possible if both partners feel comfortable and desire it. However, there may be certain situations in pregnancy when it is preferable to avoid sexual intercourse. Among them are:
- Cervical insufficiency.
- Placenta previa.
- History or risk of preterm delivery.
- History or risk of miscarriage.
- Vaginal bleeding of which the cause is unknown.
- Loss of amniotic fluid.
- Multiple pregnancy.
Therefore, the most prudent thing to do is to always consult with the specialist who is handling the pregnancy. He is the one who best knows each particular situation and will be able to advise the couple on a case-by-case basis.
FAQs from users
When is it possible to have sexual intercourse after a negative IVF?
After a negative IVF, there is no contraindication for not being able to have sexual intercourse. It is important to note that, despite having had a period after a negative pregnancy test, the ovaries may still be slightly enlarged, so it is recommended to avoid very intense physical activity, including during intercourse.
Otherwise, intercourse after a negative IVF is not contraindicated.
Is it possible to have sexual intercourse during an IVF pregnancy?
Dr. Antonio Forgiarini, gynecologist at Next Fertility Valencia, answers us in this video. As the doctor tells us:
Yes, of course. Generally, we advise to avoid sexual intercourses during the first two weeks after the embryo transfer, okay? Because, if we stimulate the uterus, the uterus will contract and it can make the implantation harder, but normally it's not a problem and if the woman is healthy (she's not bleeding, she's not having any problem) it's possible to maintain sexual intercourses.
Is it advisable to have sex after an embryo transfer? Is it advisable to have sex after an embryo transfer?
Most specialists advise against sexual intercourse after the transfer, either because it produces uterine contractions that would affect implantation, or because it generates a physical effort that would impede embryo implantation, or others.
There are also other currents that attribute beneficial effects to sexual intercourse, for example by stimulating the immunological tolerance necessary for the embryo to implant after the transfer. There are few serious scientific studies on this subject and, therefore, they have little scientific evidence.
In general, sexual intercourse is usually forbidden in most centers, rather than on the basis of scientific evidence, in order to safeguard the psychological well-being of the couple in case of an undesired outcome. Couples who experience miscarriages or negative outcomes after transfers often look for specific facts and even blame in order to explain the adverse outcome. In many occasions the feeling of guilt is towards the partners, which is tremendously harmful in a fertility process.
Is sexual intercourse possible after AI?
Artificial insemination (AI) with either partner sperm or donor sperm does not contraindicate sexual intercourse after insemination, as long as it has been carried out with a spontaneous cycle. On the other hand, if a stimulated cycle has been performed, it is necessary to differentiate between AI with conjugal sperm and AI with donor sperm.
Read more
Is it possible to have sexual intercourse after embryo transfer or do I have to rest?
The most common recommendation is not to have sexual intercourse until one week after the embryo transfer (or until the pregnancy test).
However, this does not mean that you should rest after the embryo transfer. It is best for the woman to lead a normal life, following her usual routine, but avoiding heavy physical exertion.
Suggested for you
If you want to know much more about the embryo transfer process, we recommend you to read the following article: Embryo transfer: when and how it is done.
On the other hand, if you are interested in learning more about frozen embryo transfer in particular, you can visit this link: Frozen Embryo Transfer: What are its Success Rates?
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
Aoki Y, Kumakiri J, Itakura A, Kikuchi I, Takahashi N, Satoru T. Should sexual intercourse be avoided during the embryo transfer cycle? Life-threatening ruptured heterotopic pregnancy after single thawed embryo transfer: case report and review of the literature. Clin Exp Obstet Gynecol. 2017;44(3):489-491. (View)
Ata B, Abou-Setta AM, Seyhan A, Buckett W. Application of seminal plasma to female genital tract prior to embryo transfer in assisted reproductive technology cycles (IVF, ICSI and frozen embryo transfer). Cochrane Database Syst Rev. 2018 Feb 28;2(2):CD011809. (View)
Barad DH. Hypothesis: does exposure to sperm lead to pregnancy? BJOG. 2019 Jan;126(2):226. (View)
Crawford G, Ray A, Gudi A, Shah A, Homburg R. The role of seminal plasma for improved outcomes during in vitro fertilization treatment: review of the literature and meta-analysis. Hum Reprod Update. 2015 Mar-Apr;21(2):275-84. (View)
Hosoya S, Kasahara Y, Komazaki H, Kishi H, Takano H, Okamoto A. A rare case of heterotopic pregnancy after a single embryo transfer: A case report and literature review. J Obstet Gynaecol Res. 2021 Oct;47(10):3707-3711. (View)
Mains L, Ryan G, Sparks A, Van Voorhis B. Sextuplets: an unusual complication of single embryo transfer. Fertil Steril. 2009 Mar;91(3):932.e1-2. (View)
Milki AA, Hinckley MD, Grumet FC, Chitkara U. Concurrent IVF and spontaneous conception resulting in a quadruplet pregnancy. Hum Reprod. 2001 Nov;16(11):2324-6. (View)
Nawroth F, von Wolff M. Seminal Plasma Activity to Improve Implantation in In Vitro Fertilization-How Can It Be Used in Daily Practice? Front Endocrinol (Lausanne). 2018 Apr 27;9:208. (View)
Ola B, Hammadieh N, Papaioannou S, Afnan M, Sharif K. The effect of intercourse on pregnancy rates during assisted human reproduction. Hum Reprod. 2001 Sep;16(9):2029-30. (View)
Saccone G, Di Spiezio Sardo A, Ciardulli A, Caissutti C, Spinelli M, Surbek D, von Wolff M. Effectiveness of seminal plasma in in vitro fertilisation treatment: a systematic review and meta-analysis. BJOG. 2019 Jan;126(2):220-225. (View)
Tremellen KP, Valbuena D, Landeras J, Ballesteros A, Martinez J, Mendoza S, Norman RJ, Robertson SA, Simón C. The effect of intercourse on pregnancy rates during assisted human reproduction. Hum Reprod. 2000 Dec;15(12):2653-8. (View)
von Wolff M, Rösner S, Germeyer A, Jauckus J, Griesinger G, Strowitzki T. Intrauterine instillation of diluted seminal plasma at oocyte pick-up does not increase the IVF pregnancy rate: a double-blind, placebo controlled, randomized study. Hum Reprod. 2013 Dec;28(12):3247-52. (View)
FAQs from users: 'When is it possible to have sexual intercourse after a negative IVF?', 'Is it possible to have sexual intercourse during an IVF pregnancy?', 'Is it advisable to have sex after an embryo transfer? Is it advisable to have sex after an embryo transfer?', 'Is sexual intercourse possible after AI?' and 'Is it possible to have sexual intercourse after embryo transfer or do I have to rest?'.
Authors and contributors