Repeated miscarriage also called recurrent miscarriage, is defined as the gestational loss of 3 or more pregnancies before 20 weeks. In this case, the couple is not sterile because they are able to conceive, but there is a problem of infertility because they are unable to carry the pregnancies to term.
Repeated miscarriages have a great emotional consequence on expectant parents, as the disappointment of not having a baby adds to the frustration of having lost several pregnancies.
The causes of repeated miscarriage are very diverse, sometimes unknown, which aggravates the situation of infertility and increases the waiting time to find the appropriate treatment to have a child.
Provided below is an index with the 8 points we are going to expand on in this article.
- 1.
- 2.
- 2.1.
- 2.2.
- 2.3.
- 2.4.
- 3.
- 4.
- 5.
- 5.1.
- 5.2.
- 5.3.
- 5.4.
- 5.5.
- 5.6.
- 5.7.
- 6.
- 7.
- 8.
What are the repeated miscarriages?
According to the World Health Organization (WHO), an abortion is defined as the spontaneous termination of pregnancy before the fetus is viable (weighing less than 500 grams or 20-22 weeks of gestation). If, in addition, we attach the tag "repeat", it means that 3 or more consecutive gestational losses have occurred before the 20th week.
On the other hand, suffering repeated miscarriages does not mean that it is not possible to have a viable pregnancy and a healthy child between gestational losses. Depending on the cause of the miscarriages, the probability of suffering a new loss may be higher or lower, but there is a chance of achieving a live newborn.
Recurrent miscarriage can be primary, when the woman has failed to carry a pregnancy to term, or secondary, when the woman or couple has previously had a child.
Therefore, even if the definition of repeat miscarriage specifies that gestational losses are consecutive, if there have been 3 or more miscarriages during the woman's entire reproductive life, one must already think that there is an underlying problem.
Obviously, only spontaneous abortions are counted for the diagnosis of recurrent abortion. In no case will voluntary and induced abortions are included as a woman's decision.
Finally, it should be noted that the American College of Obstetricians and Gynecologists( ACOG) already consider recurrent miscarriage when there are 2 consecutive gestational losses, although there is no clear consensus on this.
However, specialists recommend starting studies to find out the causes of miscarriages if two pregnancy losses have already occurred.
Causes of recurrent miscarriage
Recurrent pregnancy loss occurs among 3-5% of couples or single women seeking pregnancy.
Epidemiology varies depending on maternal age. A woman under 30 years of age has only a 25% chance of a new miscarriage. On the other hand, over the age of 40, there is a 50-60% chance of a recurrence of gestational loss.
Sometimes it is difficult to know what is causing repeated miscarriages. Other times, on the other hand, it is found out after some analysis, and the necessary measures can be taken.
Below, we discuss the causes of repeat miscarriage in order of probability:
Genetic Causes
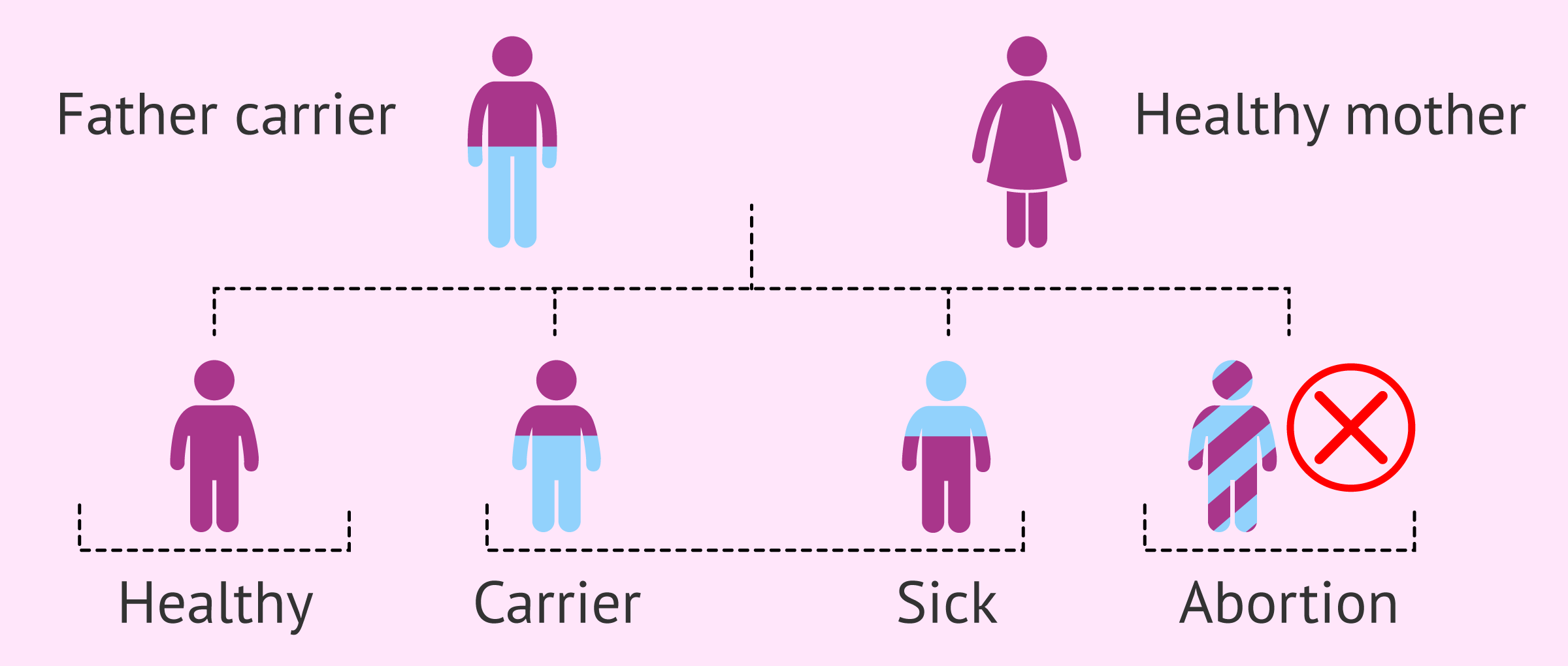
In 50% of cases of miscarriage, the origin is genetic. However, a genetic cause is attributed to only 3-8% of couples with repeated miscarriages.
The most influential factor in terms of miscarriages due to genetic causes is advanced maternal age. With the decrease in ovarian reserve and oocyte quality, the probability of fertilizing embryos with trisomies (3 chromosomes instead of 2) that are not compatible with life increases.
On the other hand, it may happen that one or both parents carry a chromosomal alteration that goes unnoticed but, when they have offspring, gives rise to non-viable embryos. This is what is known as a balanced chromosomal rearrangement, which can be of different types:
- Reciprocal translocations
- Robertsonian translocations
- Investments
Finally, it is worth noting the possible alterations in male spermatogenesis, resulting in the formation of spermatozoa with genetic alterations.
Immunological causes
Today, several factors related to the immune system have been found to be associated with repeat miscarriage. Generally speaking, we will divide them into the following two groups:
- Autoimmune causes
- here we find thrombophilias, both inherited and acquired, which translate into a state of hypercoagulability of the maternal blood, which causes clots to form that can reach the placenta and affect blood flow to the fetus, causing gestational loss.
Special attention should be paid to antiphospholipid syndrome (APS), a type of acquired thrombophilia that is responsible for 12-15% of recurrent miscarriages. As for inherited thrombophilias, the most frequent genetic mutations that cause them are Factor V Leiden and the prothrombin mutation.
- Alloimmune causes
- in this case, miscarriages occur because the body does not recognize the fetus as its own structure and, as a consequence, produces antibodies to reject it. This involves the so-called Natural Killer (NK) cells, a type of lymphocyte with the capacity to destroy organisms that it does not recognize as part of the woman's body, and its KIR receptors, which are responsible for identifying and recognizing the fetus as its own or foreign.
So that this immunological rejection does not occur in all pregnancies, women have an immunological tolerance mechanism that allows embryo implantation without problems. When this immunosuppression mechanism fails, pregnancy loss occurs.
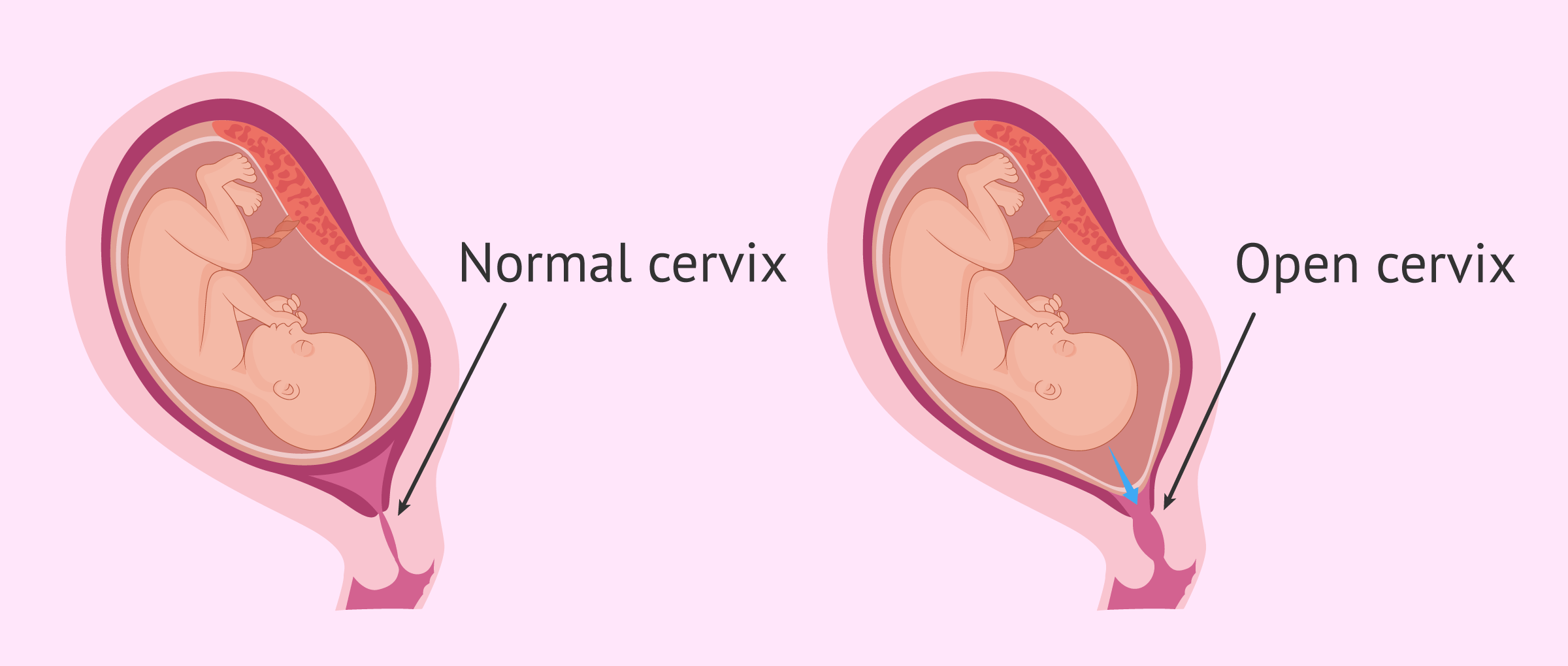
Anatomical causes
They refer to malformations or other alterations that the woman's uterus may have where gestation takes place.
These causes are usually more obvious and some can be diagnosed with an ultrasound scan.
For example, the most common alterations are the following:
- Uterus septum
- Submucous uterine myoma
- Asherman's syndrome
- Cervical insufficiency
In general, any alteration that distorts the morphology of the uterus or alters its functionality. In the latter case, the role of the endometrium, its innermost layer, and the one in which the embryo implants, must also be emphasized.
Most of these pathologies can be eliminated with surgery. You can read more about this topic at the following link: Female infertility due to a uterine factor.
Endocrine causes
Recurrent miscarriages may also be related to hormonal problems in the woman, although this is one of the least likely factors. Specifically, there are 3 different situations:
- Corpus luteum insufficiency
- refers to the inability of the ovary to produce progesterone, a hormone that is very important for the maintenance of pregnancy.
- Diabetes mellitus
- elevated blood glucose concentration.
- Thyroid disorders
- hypothyroidism and hyperthyroidism.
Obviously, not all women suffering from these disorders will suffer repeated miscarriages: only the most severe cases are associated.
Diagnosis
A multitude of tests are available to determine the cause of recurrent miscarriages. The following are the most important ones:
- Male and female karyotypes
- Imaging tests in women to view the anatomy of the uterus: hysterosalpingography, ultrasound or hysteroscopy
- Endometrial biopsy
- Hormonal analysis: prolactin level, progesterone and thyroid gland function
- Sperm DNA fragmentation study (TUNEL)
- FISH of spermatozoa
- Study of thrombophilias: lupus anticoagulant factor and anticardiolipin antibodies
- Immunological study
- Levels of vitamin D
In 50% of the cases in which repeat abortion is studied, the results of all tests are normal. This results in what is known as idiopathic or unexplained recurrent miscarriage.
In a situation of repeated miscarriages of unknown cause, the woman is recommended to follow strict control of the next pregnancy, including psychological support if necessary, in order to avoid a recurrence of gestational loss.
Considering undergoing a fertility treatment? By getting your individual Fertility Report your will see different clinics especially selected for you out of the pool of clinics that meet our strict quality criteria. Moreover, it will offer you a comparison between the fees and conditions each clinic offers in order for you to make a well informed choice.
Treatment of recurrent miscarriage
The strategy for achieving a viable pregnancy and the birth of a healthy child in women who suffer repeated miscarriages will depend on the specific cause of the miscarriage. Therefore, each couple or woman will need a personalized treatment.
Below, we will discuss some strategies that can be followed in order to have a baby:
- PGD
- when there is a genetic alteration that stops embryonic development.
- Gamete donation
- if pregnancy is not achieved after several attempts, if it is not possible to identify the genetic cause or if no healthy embryo is obtained after PGD.
- Heparin and/or aspirin
- for coagulation problems or thrombophilic causes. It is necessary to keep a strict control of the pregnancy and to personalize the dose of medication needed at each moment.
- Surrogacy
- in cases where the woman is unable to gestate because this would endanger her life.
Some of the causes of recurrent miscarriage, such as immunological causes, may require combined treatment by various specialists. In this case, all physicians treating the woman or the couple will have to agree on the strategy to be followed.
FAQs from users
What are the causes of repeated biochemical pregnancies?
A biochemical pregnancy is an early pregnancy loss that occurs shortly after implantation.
The exact cause of a biochemical pregnancy is unknown. But in most cases miscarriage is due to problems with the embryo, possibly caused by poor quality sperm or eggs.
Read more
What is antiphospholipid syndrome?
Antiphospholipid syndrome (APS) is an entity with specific clinical and analytical features independent of other autoimmune entities. The etiopathogenesis of the condition is unknown. This means that the mechanism by which antiphospholipid antibodies cause fetal losses is not known. However, it seems that a coagulation phenomenon (thrombosis) may be at the basis of the problem.
Ultimately, pregnant patients affected by SAP are at risk of recurrent miscarriages and recurrent late fetal losses. Therefore, it is imperative to rule out this syndrome in these patients by determining the possible presence of APL or ACA.
Once other causes of miscarriage have been ruled out, and a diagnosis of SAP has been made, treatment will be based fundamentally on drugs with an antiplatelet (acetylsalicylic acid) and/or anticoagulant (Heparin) effect.
Can repeated miscarriages have a male cause?
The truth is that, after a detailed study of the individual case, we are sometimes unable to make an aetiological diagnosis. That is, we do not determine the cause of the miscarriages. It is important to note that in couples with repeated miscarriages in which the cause of the miscarriages is not found, the probability of a subsequent full-term pregnancy is greater than 50%.
Among the most common causes of repeat miscarriages are genetic causes and the so-called primary antiphospholipid syndrome.
However, recent studies point to a possible male factor as the origin of repeat miscarriages. In recent years, semen quality has declined, largely due to stress, long working hours, environmental pollution, exposure to heat, alcohol and tobacco, poor eating habits and even the use of tight underwear.

Tests are available to identify chromosomal alterations in semen samples.
What tests are included in the repeat miscarriage study?
Normally, the study of repeated miscarriages consists of an analysis of the Antiphospholipid Syndrome, genetic testing, assessment of thrombophilias, hysteroscopy, and transvaginal ultrasound to study anatomy.
Read more
What are the signs and symptoms of recurrent miscarriage?
The main symptoms of recurrent miscarriage are the same as those a woman has when she has a miscarriage: heavy bleeding and severe pelvic or abdominal pain.

Urinary tract infections and vaginal infections are also indicative of miscarriage risk.
What types of recurrent miscarriages are there?
Recurrent miscarriages or repeat miscarriages may be:
- Primary
- the woman or couple has failed to carry any pregnancy to term, i.e. all pregnancies have ended in miscarriage.
- Secondary
- when the woman or couple has achieved a pregnancy and had a baby prior to recurrent miscarriages.
Can repeat abortions be prevented?
The best way to prevent recurrent miscarriages from occurring is to know what causes them. If you do not know why repeat miscarriages occur when a woman becomes pregnant, it will be difficult to prevent them from happening again.
Recommended readings
As we have said, it is necessary to do many tests on the couple after having several repeated miscarriages in order to know the cause and what treatment to apply. In the following article, you will find information about these tests in women: What are the tests of a female fertility study?
Similarly, there are also tests to evaluate male fertility. In the case of repeated miscarriage, the malefactor is studied to a lesser extent, but here you can find some of these tests: What do the tests of a male fertility study consist of?
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
Dan Li, Lianwen Zheng, Donghai Zhao, Ying Xu, Yeling Wang. The Role of Immune Cells in Recurrent Spontaneous Abortion. Reprod Sci. 2021 Dec;28(12):3303-3315. doi: 10.1007/s43032-021-00599-y (View)
Deepika Delsa Dean, Sarita Agarwal, Poonam Tripathi. Connecting links between genetic factors defining ovarian reserve and recurrent miscarriages. J Assist Reprod Genet. 2018 Dec;35(12):2121-2128. doi: 10.1007/s10815-018-1305-3 (View)
Diana Alecsandru, Amber M Klimczak, Juan A Garcia Velasco, Paul Pirtea, Jason M Franasiak. Immunologic causes and thrombophilia in recurrent pregnancy loss. Fertil Steril. 2021 Mar;115(3):561-566. doi: 10.1016/j.fertnstert.2021.01.017 (View)
Marie Carbonnel, Paul Pirtea, Dominique de Ziegler, Jean Marc Ayoubi. Uterine factors in recurrent pregnancy losses. Fertil Steril. 2021 Mar;115(3):538-545. doi: 10.1016/j.fertnstert.2020.12.003 (View)
Marta Kacprzak, Marta Chrzanowska, Beata Skoczylas, Hanna Moczulska, Maciej Borowiec, Piotr Sieroszewski. Genetic causes of recurrent miscarriages. Ginekol Pol. 2016;87(10):722-726. doi: 10.5603/GP.2016.0075 (View)
Paul Pirtea, Ettore Cicinelli, Rosalba De Nola, Dominique de Ziegler, Jean Marc Ayoubi. Endometrial causes of recurrent pregnancy losses: endometriosis, adenomyosis, and chronic endometritis. Fertil Steril. 2021 Mar;115(3):546-560. doi: 10.1016/j.fertnstert.2020.12.010 (View)
Tianqing Deng, Xiaoyang Liao, Shaomi Zhu. Recent Advances in Treatment of Recurrent Spontaneous Abortion. Obstet Gynecol Surv. 2022 Jun;77(6):355-366. doi: 10.1097/OGX.0000000000001033 (View)
FAQs from users: 'What are the causes of repeated biochemical pregnancies?', 'What is antiphospholipid syndrome?', 'Can repeated miscarriages have a male cause?', 'What tests are included in the repeat miscarriage study?', 'What are the signs and symptoms of recurrent miscarriage?', 'What types of recurrent miscarriages are there?' and 'Can repeat abortions be prevented?'.
Authors and contributors


More information about Cristina Algarra Goosman










The doctors have told me that I have a genetic anomaly that does not allow the embryos to develop. What options do I have to become a mother?
Hi KarlaZ,
If you have a genetic complication that does not allow you to conceive with your eggs, there are mainly two ways to try to solve the problem.
On the one hand, you can resort to egg donation, which would be indicated in the case where there is no impediment to achieving pregnancy except genetics.
On the other hand, there is the possibility of resorting to surrogacy with donated eggs, which would solve both the genetic problem and any other problem that would make pregnancy impossible.
I hope I have helped you,
Best regards
Hello, I have already had 3 miscarriages in a row. I don’t know what we are doing wrong, we manage to get pregnant but we lose it before 12 weeks. Is there anything I should do differently?
Hi Millie,
After several recurrent miscarriages, it is advisable to approach a fertility expert to evaluate, if possible what is the reason for the recurrent miscarriages. If identified, it will be possible to put a treatment that will try to avoid another miscarriage.
If it does not work, other techniques such as PGD or gamete donation may be used.
I hope I have helped you,
Best regards
Teen moms should think about if they want to keep their baby or put it up to adoption, once they find out they are pregnant. Once I found out I was pregnant I fell in love with my baby. I got an ultrasound and that same day i fell in love with her. Listening to her heart was exciting. I knew that i wanted to keep my baby. But if for any reason teen moms know that they won’t be able to care for their child’s needs and/or they know that they will not love their baby, then they should put the baby up to adoption and let a beautiful family love your baby. Babies need a lot of love and they have to be cared for. So if you’re considering about putting your baby up to adoption think about the pros and cons before making your final decision.