Antiphospholipid syndrome, antiphospholipid antibody syndrome, Hughes syndrome or APS is a systemic autoimmune disease. APS is characterized by arterial, venous or small vessel thrombosis. In addition, this syndrome is also associated with miscarriages, fetal losses and premature births.
APS is associated with the presence of antiphospholipid antibodies (AAF). These molecules alter the function of phospholipids and create a procoagulant (which favors coagulation) and proinflammatory state, which increases the risk of thrombosis.
Provided below is an index with the 8 points we are going to expand on in this article.
- 1.
- 1.1.
- 2.
- 3.
- 4.
- 4.1.
- 5.
- 5.1.
- 5.2.
- 5.3.
- 5.4.
- 5.5.
- 6.
- 7.
- 8.
What is antiphospholipid syndrome?
It is an autoimmune disease characterized by the appearance of arterial or venous blood clots. In addition, APS is associated with recurrent miscarriages, fetal loss and preterm delivery.
APS is a rare disease (40-50 cases / 100,000 inhabitants). Despite this, the incidence of FAS is higher in younger women, often diagnosed between the ages of 30-40 years.
A distinction can be made between primary antiphospholipid syndrome or secondary antiphospholipid syndrome if it is associated with another disease, usually systemic lupus erythematosus (SLE). However, APS may be associated with other autoimmune diseases, infections, neoplasms, some drugs and other diseases.
Antiphospholipid antibodies (AAF)
Antiphospholipid antibodies (AAF) play an important role in the development of this syndrome. AAFs are antibodies that the immune system produces erroneously, as they will affect the function of phospholipids. This will create a state of hypercoagulation which increases the risk of thrombosis.
The main antiphospholipid antibodies are:
- Lupus anticoagulant (LA).
- Anticardiolipin antibodies.
- Anti-β2glycoprotein I antibodies (Anti-β2GPI).
The reason for the occurrence of these AAFs is not known. An external factor in a genetically predisposed person may be the cause of its appearance.
Symptomatology
There are occasions when no symptomatology is present despite having AAF. However, the presence of AAF predisposes to an increased risk of thrombosis in certain situations such as:
- Prolonged rest period.
- Pregnancy.
- Surgeries
- Arterial hypertension and diabetes mellitus.
- Obesity.
- Ingestion of oral contraceptives (estrogens).
- Smoking.
- Autoimmune disease such as systemic lupus erythematosus (SLE).
- Neoplasms.
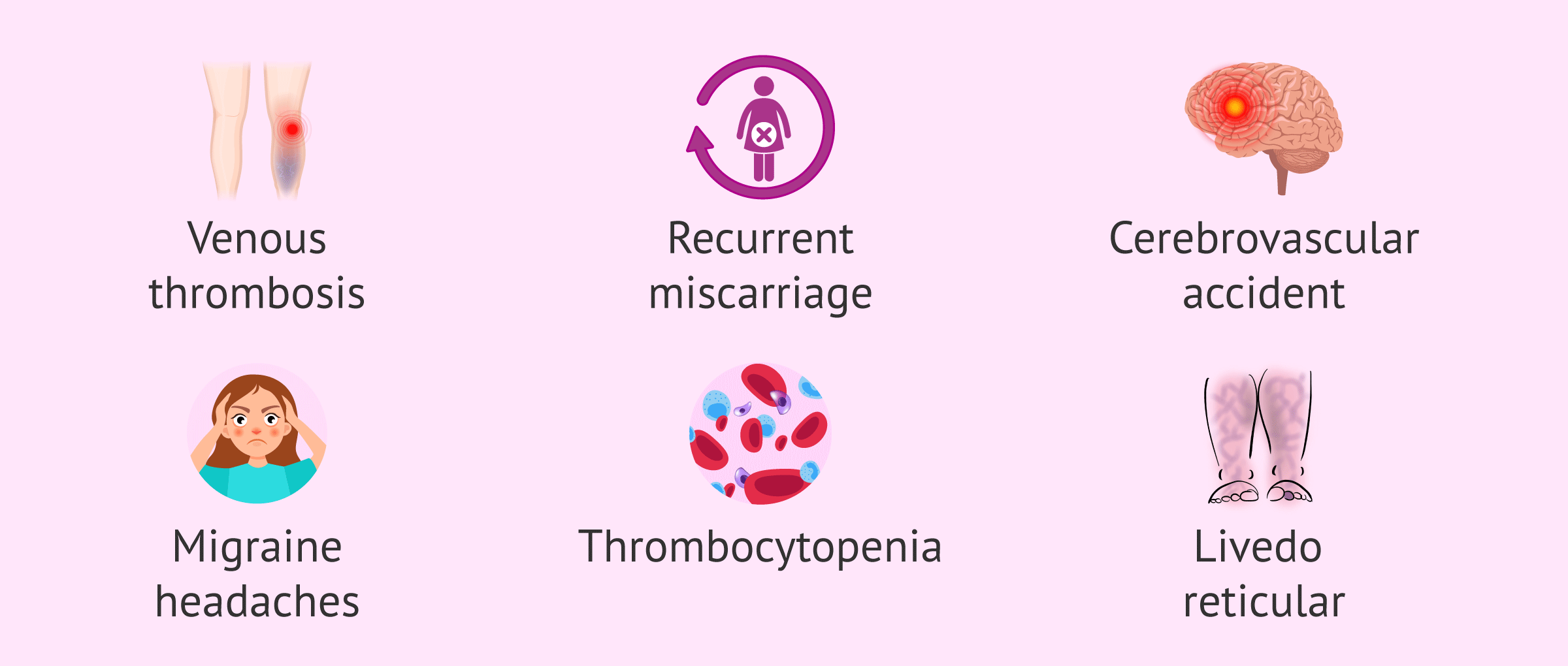
However, FAS can have clinical manifestations as varied as those mentioned below:
- Venous, arterial or small vessel and recurrent thrombosis.
- Recurrent miscarriage or fetal loss, preterm birth, preeclampsia, eclampsia and fetal growth retardation.
- Stroke and transient ischemic attack.
- Cognitive impairment and other neurological manifestations such as migraine.
- Thrombocytopenia (low platelet count).
- Marble-like or marmoreal skin (livedo reticular).
It should be noted that the symptoms and severity of a blood clot will depend on the organ affected and the extent of the involvement.
Diagnosis
The diagnosis of FAS is usually made in patients who have had a history of thrombosis, recurrent miscarriages, fetal loss or premature delivery with no other apparent explanation. This constitutes, broadly speaking, the clinical criteria for its diagnosis.
However, laboratory criteria are also necessary for the diagnosis of definitive FAS. This criterion is determined by a blood test to check for any of the 3 AAF mentioned above. However, in case of a positive result for any FFA, the analysis must be repeated in a period of time longer than 12 weeks to confirm the result.
Treatment
First of all, situations that may increase the risk of thrombosis should be avoided and treated.
Currently, the treatment of APS is aimed at decreasing the risk of blood clot formation. In patients with positive AAF, but without clinical symptoms, spot treatment can be administered in situations that increase their risk of thrombosis. In patients at higher risk, treatment may be indefinite.
In the face of clinical manifestations of FAS, treatment will vary according to the individual case.
Treatment during pregnancy
In the case of a pregnant woman, maternal thrombosis and pregnancy loss must be controlled and avoided. However, the specialist will study the treatment individually.
Acetylsalicylic acid and heparin are drugs frequently used in pregnancy. The follow-up of the entire gestation period requires strict multidisciplinary control by obstetric specialists, hematologists and rheumatologists or internists with experience in this type of pathology.
On the other hand, ovarian stimulation performed in assisted reproduction techniques produces an increase in estrogen levels. Because of this, the risk of thrombosis may be increased with respect to the general population, especially in patients prone to develop thrombosis.
Assisted procreation, as any other medical treatment, requires that you rely on the professionalism of the doctors and staff of the clinic you choose. Obviously, each clinic is different. Get now your Fertility Report, which will select several clinics for you out of the pool of clinics that meet our strict quality criteria. Moreover, it will offer you a comparison between the fees and conditions each clinic offers in order for you to make a well informed choice.
In these cases, appropriate antithrombotic treatment should be administered and it is recommended to avoid ovarian hyperstimulation syndrome.
FAQs from users
Can I get pregnant with APS?
Antiphospholipid syndrome or APS is an autoimmune disorder characterized by thrombotic events and/or problems in pregnancy associated with the presence of antiphospholipid antibodies in the blood, such as anticardiolipin antibodies, anti-beta2-glycoprotein antibodies or lupus anticoagulant. It can occur in isolation or in the context of other autoimmune diseases such as lupus erythematosus sitematosus.
Complications in pregnancy include miscarriages (especially those after 10 weeks), preeclampsia or placental insufficiency. The mechanism by which PAS produces these adverse events could be a defect in placentation. Thus, in women with APS, the risk of thrombombolism during pregnancy or postpartum is 5-12% (in the general population it would be <0.10%).Treatment of APS during pregnancy reduces the likelihood of thrombosis and pregnancy complications. The medication that is prescribed will depend on the problems that the woman has presented, but normally consists of acetylsalicylic acid or ASA (low-dose aspirin) and heparin, although sometimes other drugs such as hydroxychloroquine may be used. If thrombosis has occurred, lifelong treatment with anticoagulants will probably be necessary, not only during pregnancy. If the PBS has only been expressed as complications of pregnancy it can probably be withdrawn 6 weeks after delivery.
What is antiphospholipid syndrome?
Antiphospholipid syndrome (APS) is an entity with specific clinical and analytical features independent of other autoimmune entities. The etiopathogenesis of the condition is unknown. This means that the mechanism by which antiphospholipid antibodies cause fetal losses is not known. However, it seems that a coagulation phenomenon (thrombosis) may be at the basis of the problem.
Ultimately, pregnant patients affected by SAP are at risk of recurrent miscarriages and recurrent late fetal losses. Therefore, it is imperative to rule out this syndrome in these patients by determining the possible presence of APL or ACA.
Once other causes of miscarriage have been ruled out, and a diagnosis of SAP has been made, treatment will be based fundamentally on drugs with an antiplatelet (acetylsalicylic acid) and/or anticoagulant (Heparin) effect.
Why is anticoagulation important in antiphospholipid syndrome (APS)?
Treatment with anticoagulants is of great importance in APS, since these patients have a hypercoagulable situation that increases the risk of thrombosis and obstetric problems.
What does it mean that FAS is an autoimmune disease?
In an autoimmune disease the body's immune system produces antibodies that will attack the body itself. In the case of FAS, these antibodies alter the function of phospholipids creating a situation of hypercoagulation.
What is catastrophic antiphospholipid syndrome?
This is the most severe form of APS. This type of APS is characterized by multiple thromboses of sudden onset, leading to multiple organ involvement (either simultaneously or within a short period of time). Multi-organ failure can make catastrophic APS fatal.
Suggested for you
If you would like to learn more about immunological infertility, you can visit the following link: Immunological infertility: types, causes and treatments.
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
Cáliz Cáliz R, Díaz Del Campo Fontecha P, Galindo Izquierdo M, López Longo FJ, Martínez Zamora MÁ, Santamaría Ortiz A, Amengual Pliego O, Cuadrado Lozano MJ, Delgado Beltrán MP, Carmona Ortells L, Cervantes Pérez EC, Díaz-Cordovés Rego G, Garrote Corral S, Fuego Varela C, Martín López M, Nishishinya B, Novella Navarro M, Pereda Testa C, Sánchez Pérez H, Silva-Fernández L, Martínez Taboada VM. Recommendations of the Spanish Rheumatology Society for Primary Antiphospholipid Syndrome. Part I: Diagnosis, Evaluation and Treatment. Reumatol Clin. 2020 Mar-Apr;16(2 Pt 1):71-86. English, Spanish.
Cáliz Cáliz R, Díaz Del Campo Fontecha P, Galindo Izquierdo M, López Longo FJ, Martínez Zamora MÁ, Santamaria Ortiz A, Amengual Pliego O, Cuadrado Lozano MJ, Delgado Beltrán MP, Ortells LC, Pérez ECC, Rego GD, Corral SG, Varela CF, López MM, Nishishinya B, Navarro MN, Testa CP, Pérez HS, Silva-Fernández L, Taboada VMM. Recommendations of the Spanish Rheumatology Society for Primary Antiphospholipid Syndrome. Part II: Obstetric Antiphospholipid Syndrome and Special Situations. Reumatol Clin. 2020 Mar-Apr;16(2 Pt 2):133-148. English, Spanish.
Carmi O, Berla M, Shoenfeld Y, Levy Y. Diagnosis and management of catastrophic antiphospholipid syndrome. Expert Rev Hematol. 2017 Apr;10(4):365-374 (View)
Cervera R. Antiphospholipid syndrome. Thromb Res. 2017 Mar;151 Suppl 1:S43-S47 (View)
Cervera R. Estrategias terapéuticas en el síndrome antifosfolipídico [Therapeutic strategies in antiphospholipid syndrome]. Reumatol Clin. 2010 Jan-Feb;6(1):37-42. Spanish (View)
Garcia D, Erkan D. Diagnosis and Management of the Antiphospholipid Syndrome. N Engl J Med. 2018 May 24;378(21):2010-2021 (View)
Petri M. Antiphospholipid syndrome. Transl Res. 2020 Nov;225:70-81 (View)
Ruiz-Irastorza G, Crowther M, Branch W, Khamashta MA. Antiphospholipid syndrome. Lancet. 2010 Oct 30;376(9751):1498-509 (View)
Sammaritano LR. Antiphospholipid syndrome. Best Pract Res Clin Rheumatol. 2020 Feb;34(1):101463 (View)
Schreiber K, Hunt BJ. Managing antiphospholipid syndrome in pregnancy. Thromb Res. 2019 Sep;181 Suppl 1:S41-S46 (View)
FAQs from users: 'Can I get pregnant with APS?', 'What is antiphospholipid syndrome?', 'Why is anticoagulation important in antiphospholipid syndrome (APS)?', 'What does it mean that FAS is an autoimmune disease?' and 'What is catastrophic antiphospholipid syndrome?'.