A molar pregnancy, also known as hydatidiform mole, is a disorder in early pregnancy based on the growth of a benign mass or tumor inside the uterus. This mass is made up of trophoblasts, the cells that normally develop into the placenta. Therefore, it is a type of gestational trophoblastic disease (GTD).
The causes of this pregnancy disorder are not known exactly, although there are some risk factors such as nutritional deficiencies or abnormalities in the uterus.
The initial symptoms of molar pregnancy are similar to those of a normal pregnancy. Painless vaginal bleeding usually occurs in the fourth or fifth week of pregnancy. In addition, the size of the uterus may increase earlier than expected.
A molar pregnancy can present serious complications, such as cancer. Therefore, it is of great importance to establish early treatment.
Provided below is an index with the 10 points we are going to expand on in this article.
- 1.
- 1.1.
- 1.2.
- 2.
- 3.
- 4.
- 5.
- 6.
- 7.
- 7.1.
- 7.2.
- 7.3.
- 7.4.
- 7.5.
- 7.6.
- 8.
- 9.
- 10.
Types of molar pregnancy
Hydatidiform mole is classified as either partial or complete, but it is important to note the differences between the two. Each type of molar pregnancy is described below.
Partial hydatidiform mole (PHM)
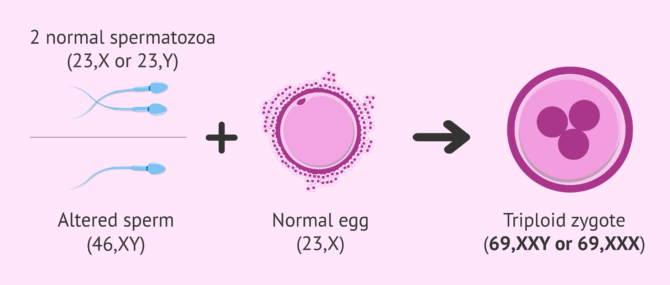
The etiology of this type of molar pregnancy can be caused in two ways:
- Fertilization of a single egg with two normal sperm (23,X or 23,Y).
- Fertilization of an egg with a single altered, diploid (46,XY) sperm.
In this case, the mass may be composed of placental debris and even a small embryo with severe defects.
The embryo's karyotype is triploid, that is, it is formed by the 23 chromosomes from the mother and two sets of chromosomes from the father. Consequently, the embryo has 69 chromosomes, when the normal number is 46.
However, the baby will not be able to develop normally, since the placental tissue grows out of control. Thus, partial molar pregnancy usually ends in miscarriage. However, this type of mole has virtually no malignant potential.
Complete hydatidiform mole (CHM)
The complete molar pregnancy (CHM) is produced by fertilization between a sperm and an egg without genetic information. The sperm initiates cell division and a placenta is formed, but there is no embryo. The placenta is growing and producing pregnancy hormone hCG, so pregnancy tests would be positive.
This type of mole is diploid, that is, it is formed by 46 chromosomes because the DNA of the sperm is duplicated. However, all chromosomes are paternal, since the egg lacks DNA.
What are the risk factors?
Currently, approximately 1 in every 1,000 pregnancies is diagnosed as a molar pregnancy. The exact causes of this type of pregnancy are not known, but there are several factors associated with hydatidiform mole, such as:
- Mother's age. Women older than 35 years and younger than 20 years are more likely to have a molar pregnancy.
- Previous molar pregnancy.
- History of spontaneous abortion.
- Diet poor in protein, folic acid or carotenes that are part of foods such as carrots, chard, pumpkin, lettuce, spinach, etc.
In addition, the risk of suffering a hydatidiform mole does not change due to a change of partner. There is also scientific evidence, although to a lesser extent, of an increased risk of this type of disorder among blood groups A and AB.
Symptoms molar pregnancy
During the first weeks of gestation there is no difference between a molar pregnancy and a normal pregnancy, since their symptoms are similar. The pregnancy test is positive and all signs confirm the presence of pregnancy.
Many times hydatidiform mole is asymptomatic and is discovered at the first ultrasound scan. Other times, the symptoms that appear are the following:
- Abnormal growth of the uterus.
- Severenausea and vomiting.
- Vaginal bleeding during the first trimester of pregnancy.
- Symptoms of hyperthyroidism, such as heat intolerance, watery stools, rapid heart rate, restlessness, nervousness, unexplained weight loss, etc.
- High blood pressure accompanied by swelling of feet, ankles and legs in the first trimester of pregnancy.
As already mentioned, the embryo does not complete its evolution. In most cases there is a miscarriage accompanied by dark-colored, watery bleeding.
What is the diagnosis like?
Normally, the first signs of hydatidiform mole appear with the development of an abnormal uterus and the absence of a heartbeat, along with vaginal bleeding.
The specialist performs a pelvic examination to reveal whether the uterus is larger or smaller and if there is an enlargement of the ovaries.
Ultrasound will show an abnormal placenta, with or without development of a fetus. This imaging test does not detect a heartbeat or fetal movement. In addition, other conclusive tests that can be performed are:
- Blood test including a quantification of human chorionic hormone (hCG). This hormone is found in higher concentration in complete molas than in partial molas.
- Magnetic resonance imaging of the abdomen.
- Total blood cell count.
- Blood coagulation test.
- Renal and liver function tests.
Hydatidiform mole treatment
This type of pregnancy is not viable because it can develop into a cancerous mass. To prevent complications, abnormal placental tissue must be removed.
Treatment of molas usually involves some of the following tests:
- Dilatation and curettage to remove tissue from the uterus. Local or general anesthesia is administered for this test.
- Hysterectomy (removal of the uterus) may be an option for older women who do not wish to become pregnant again.
- Control of hCG hormone until its values return to normal. If the levels of this hormone increase or do not normalize, additional tests will be necessary to check if the tumor has spread.
- Chemotherapy in cases where the mole persists or has spread throughout the body.
Once treatment is completed, the couple must use reliable contraceptives for 6 to 12 months to prevent pregnancy.
What is the prognosis of molar pregnancy?
Most hydatidiform moles are benign and do not lead to cancer. In general, the treatments are successful.
Only 15% of cases of molas can become malignant. These moles grow and invade other areas of the woman's body and may cause bleeding or other complications.
As for complete hydatidiform molas, very few of them develop into choriocarcinoma, i.e. an aggressive cancer of the placenta. Normally, this complication is successfully treated with chemotherapy, although in some cases it can be life-threatening.
FAQs from users
Is molar pregnancy the same as anembryonic pregnancy?
It is not the same thing. An anembryonic gestation is a gestation in which the gestational sac, the placenta, is produced, but the embryo does not develop. This type of pregnancy is usually diagnosed at 6-7 weeks gestation. Sometimes anembryonic pregnancies are manifested by bleeding, but the vast majority do not show symptoms, and are diagnosed at the time of the first trimester ultrasound.
It is at this ultrasound moment that a gestational sac, a trophoblast, is found, but no embryo is identified. Treatment is usually pharmacological or surgical curettage.

On the other hand, molar disease is a tumor of the placenta. In this type of gestation the embryo is also not identified and there is uncontrolled growth of the placenta. The symptoms are usually bleeding, in some cases expulsion through the vagina of molar tissue (grape clusters), and by very important symptoms of nausea or vomiting, because the pregnancy hormone rises disproportionately.
Can a molar pregnancy give rise to a tumor?
Molar pregnancy is a rare complication of pregnancy in which trophoblastic tissue (which in a standard pregnancy forms the placenta) proliferates abnormally.
Molar pregnancy is a disease of benign behavior in most cases, but it can give rise to gestational trophoblastic neoplasia which has malignant features.
The most common form of molar pregnancy is hydatidiform mole, which can be complete or partial. In the complete form there is only abnormal placental tissue and in the partial form there is also fetal tissue. Partial hydatidiform mole has a benign behavior most of the time and only becomes malignant in 4% of cases, while complete hydatidiform mole is malignant in up to 20% of cases. After the treatment of molar pregnancy, a strict follow-up with frequent controls should be followed for a long period of time, because in some cases the disease can persist and give rise to gestational trophoblastic neoplasia, which can have different degrees of malignancy and give rise to tumors.
What complications can arise from hydatidiform mole?
The main complication is excessive bleeding that can occur during the removal of the hydatidiform mole.
Another very feared complication is the possibility that the hydatidiform mole may develop into choriocarcinoma, a type of tumor. This cancer can metastasize and invade other structures in the woman's body.
Can I have another molar pregnancy?
Yes, people who have already had a molar pregnancy have a 1-2% risk of having another one. This percentage represents a high risk compared to the risk of the general population.
Is it necessary to wait some time to get pregnant again after a hydatidiform mole?
Yes, specialists recommend waiting between 6 months and 1 year to try to conceive again. In addition, during this time, the specialist checks the woman to make sure that the mass does not reappear.
Is an invasive mola the same as a hydatidiform mola?
No. Invasive mole is a type of hydatidiform mole (partial or complete) that has spread into the myometrium, that is, into the muscular layer of the uterine body. It is therefore a complication of hydatidiform mole and gives rise to cancer.
Recommended readings
We have mentioned that a risk factor for hydatidiform molas is spontaneous abortions. If you want to learn more about them, you can visit the following article: Miscarriage: symptoms, causes and consequences.
Also, if you want to know what are the normal levels of beta-hCG hormone, you can click here: Beta-hCG hormone levels and weeks of pregnancy.
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
Baumgarten J, Happel C, Becker S, El-Balat A, Grünwald F. HCG-induced hyperthyroidism in a 51-year-old patient with hydatidiform mole. Nuklearmedizin. 2018 Dec;57(6):N57. doi: 10.3413/Nukmed-0990-18-08.
Ben Salah I, Najeh H, Dhouha B, Oueslati H. Partial Hydatiform Mole Associated With a Pregnancy at 22 Weeks of Amenorrhea. J Obstet Gynaecol Can. 2017 Jul;39(7):511. doi: 10.1016/j.jogc.2017.03.002.
Boufettal H, Samouh N. Invasive hydatidiform mole in the cervix. Pan Afr Med J. 2018 Jan 12;29:27. doi: 10.11604/pamj.2018.29.27.10675.
Mittal S, Menon S. Interstitial pregnancy mimicking an invasive hydatidiform mole. Am J Obstet Gynecol. 2019 May;220(5):501. doi: 10.1016/j.ajog.2018.10.024.
Nickkho-Amiry M, Horne G, Akhtar M, Mathur R, Brison DR.Hydatidiform molar pregnancy following assisted reproduction. J Assist Reprod Genet. 2019 Apr;36(4):667-671. doi: 10.1007/s10815-018-1389-9.
Ross JA, Unipan A, Clarke J, Magee C, Johns J. Ultrasound diagnosis of molar pregnancy. Ultrasound. 2018 Aug;26(3):153-159. doi: 10.1177/1742271X17748514.
Uemura N, Takai Y, Mikami Y, Ogasawara M, Saitoh M, Baba K, Tamaru J, Hara M, Seki H. Molecular cytogenetic analysis of a hydatidiform mole with coexistent fetus: a case report. J Med Case Rep. 2019 Aug 18;13(1):256. doi: 10.1186/s13256-019-2180-y.
Zhang L, Xie Y, Zhan L. The potential value of red blood cell distribution width in patients with invasive hydatidiform mole. J Clin Lab Anal. 2019 May;33(4):e22846. doi: 10.1002/jcla.22846.
Zhao T, Hou X, Su C, Wu Q. Tubal hydatidiform mole treated with salpingotomy: A case report. Clin Case Rep. 2019 Feb 19;7(4):653-655. doi: 10.1002/ccr3.2037.
Zornoza-García V, Luengo-Tabernero A, Álvarez-Domínguez A, Carriles-Sastre R, González-García C. Pregnancy in a patient aged more than fifty years. Complete hydatidiform mole. Elsevier 2010. Vol. 37 (6) 258-260. DOI: 10.1016/j.gine.2009.05.008.
FAQs from users: 'Is molar pregnancy the same as anembryonic pregnancy?', 'Can a molar pregnancy give rise to a tumor?', 'What complications can arise from hydatidiform mole?', 'Can I have another molar pregnancy?', 'Is it necessary to wait some time to get pregnant again after a hydatidiform mole?' and 'Is an invasive mola the same as a hydatidiform mola?'.
Authors and contributors
More information about Cristina Algarra Goosman









Hello, two months ago I got pregnant and the pregnancy resulted in molar pregnancy, I didn’t understand very well what it was but they had to operate to remove the tumor. I am quite disappointed and want to know if it is healthy to try for a pregnancy again, thank you.
Hello Olivia,
After intervention for molar pregnancy, it is recommended to perform a thorough control by the doctors to ensure that everything is fine and to intervene in case there is any kind of problem. For this reason, it is usually recommended that patients wait between 6 months and 1 year, enough time to observe any changes that could be made that could harm the health of the mother or the future baby.
I recommend that you talk to your doctor about the postoperative plan of action and conception plan appropriate for your case.
I hope I have helped you.
Best regards.
Hi, I am 10 weeks pregnant, I have been told that they think I have a molar pregnancy and they are going to have to remove it. We have been trying to get pregnant for a long time and now that we are successful they want to remove it. Is there anything I can do?
Hello Angeria,
A molar pregnancy is not viable, it is caused by a malformation at the time of zygote development. Most of the time this abnormal tissue has benign behavior and is not compatible with life, since the fetus would not develop properly and can be harmful to the mother because it is tissue with malignant characteristics.
I recommend that you talk to your doctor so that he/she can explain to you step by step the procedures that will be carried out and the conceptive alternatives that your particular case presents.
I hope I have helped you.
Best regards.