Ectopic pregnancy occurs when embryonic implantation occurs outside the uterine cavity. Once the egg has been fertilized, as it descends through the fallopian tube, it does not reach the mother's uterus and implants in a different tissue, which ends up causing an abortion.
In 95% of cases, ectopic pregnancies are located in the tube and are known as pregnancies at the tubal level. There are also other less frequent places such as the ovary, the abdominal cavity, or the cervical canal.
This kind of pregnancy can cause serious complications in women if it is not treated correctly once it has been detected.
Provided below is an index with the 10 points we are going to expand on in this article.
- 1.
- 2.
- 3.
- 4.
- 5.
- 6.
- 7.
- 7.1.
- 7.2.
- 7.3.
- 7.4.
- 7.5.
- 7.6.
- 7.7.
- 8.
- 9.
- 10.
Definition of ectopic pregnancy
Fertilization of the embryo takes place in the fallopian tubes after ovulation. However, the appropriate place for implantation and subsequent embryonic development is the uterus, where the endometrium is prepared for the formation of the gestational sac.
Ectopic pregnancies are amongst the most frequent causes of maternal death during the first trimester of pregnancy. The mortality rate is 1.8 deaths per 1,000 ectopic pregnancies.
Ectopic pregnancy, also known as extrauterine pregnancy, arises as a consequence of some complication during the descent of the embryo through the tube. This is not able to reach the uterus and implants in an abnormal place that does not allow its development.
What types of extra-uterine pregnancies are there?
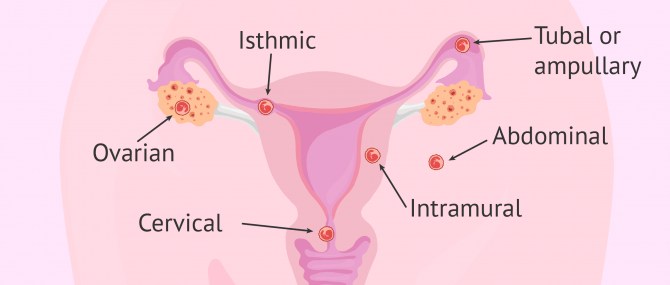
The different types of ectopic pregnancy are classified based on the place outside the womb where the embryo attaches. Most ectopic pregnancies occur in the tube, though.
The following is a list of the different types of ectopic pregnancy and their names:
- Tubal or ampullary ectopic pregnancy
- The embryo attaches in the Fallopian tube, causing inflammation and blockage.
- Isthmic ectopic pregnancy
- Implantation occurs in the isthmus of uterine tube, the closest segment to the uterus.
- Ovarian ectopic pregnancy
- Embryo implantation occurs in one of the ovaries, and it is sometimes confused for a cyst.
- Cervical ectopic pregnancy
- The embryo attaches to the cervix.
- Abdominal ectopic pregnancy
- The embryo grows outside the womb in the abdomen.
- Intramural or interstitial ectopic pregnancy
- It is a rarest of all types. The embryo attaches to the myometrium (smooth muscle within the uterus).
An heterotopic pregnancy is a "hybrid" type of ectopic pregnancy in which an extrauterine and intrauterine pregnancy occurs at the same time.
Why does an ectopic pregnancy occur?
La causa de este tipo de embarazo es el bloqueo o retraso del trayecto del óvulo fecundado a través de la trompa.
Existen una serie de factores que aumentan el riesgo de padecer un embarazo ectópico. Entre ellos están:
- Endometriosis
- Salpingitis: infection in the Fallopian tubes.
- Birth defects of the Fallopian tubes
- Advanced maternal age (>35)
- Previous ectopic pregnancies
- Smoking
- Intrauterine Device (IUD)
- Pelvic Inflammatory Disease (PID)
- Pelvic or abdominal surgery
- Fertility treatments
- Tubal ligation reversal
In some cases, finding out the cause is not possible. In fact, it may be due to hormonal imbalances.
It should be noted that the frequency of ectopic pregnancies has increased in the past 20 years due to, on the one hand, new diagnostic methods, and on the other hand, the presence of new risk factors, such as the use of Assisted Reproductive Technologies (ART).
The incidence rate of ectopic pregnancies is 1 per every 100 pregnancies, that is, 1%.
It should be noted that ectopic pregnancy could also occur after a tubal ligation if the woman decides to undergo in vitro fertilization (IVF) to attempt a pregnancy.
According to the Dr. Gorka Barrenetxea, a specialist in Gynecology and Obstetrics:
When a tubal ligation has been performed, what is done is to dry out a portion of the tubes, but another portion remains. Therefore, an ectopic pregnancy is possible.
If you would like to read more about the possible causes of extrauterine pregnancies, we recommend you visit the following article: What are the causes and consequences of ectopic pregnancy?
Symptoms
When a woman has an implantation in tissue other than the uterine endometrium, there may not be any discomfort in the initial stage or the symptoms may be similar to those of a normal pregnancy, such as fatigue, nausea or abdominal pain.
As the pregnancy progresses, other symptoms will appear that may be more serious and will put the woman on alert. These are as follows:
- Sharp, intense abdominal pain
- Abnormal vaginal bleeding
- Weakness and/or dizziness or fainting
- Lower back pain
- Shoulder pain
- Rectal pressure
- Pale skin and low blood pressure
These symptoms can become worse in case a ruptured ectopic pregnancy occurs, as it is a life-threatening situation that needs emergency surgery. As the embryo grows, the tube expands until it gets to tear or burst, given that the Fallopian tubes are narrow structures that can only stretch a little. It is a medical emergency that can cause heavy internal bleeding and may cause the woman to die if not treated on time.
In short, seeing a doctor as soon as possible if you suspect that you may be having an ectopic pregnancy is crucial. If treated on time, we can prevent further complications such as needing surgery to remove the Fallopian tube.
How is an ectopic pregnancy diagnosed?
There are two basic methods for detecting an ectopic pregnancy: determining the beta-hCG blood levels, and performing a transvaginal ultrasound.
A quantitative β-hCG blood test is used to determine whether a woman is pregnant based on the weeks of pregnancy. This type of pregnancy test is very common amongst women who have undergone a fertility treatment such as IUI or IVF.
If the result is positive, the pregnancy is confirmed by ultrasound within 2 weeks in order to determine the presence of an embryonic sac.
If no gestational sac was seen by ultrasound with a positive β-hCG blood test result, you may be having an ectopic pregnancy. In such case, the β-hCG blood test would be repeated to confirm the levels of biochemical markers such as progesterone, placental protein 14, CA 125, and creatine kinase (CK), among others.
In ectopic pregnancies, the beta-hCG hormone doesn't increase so rapidly as in normal pregnancies. As a consequence, the levels remain low.
Treatment
Many ectopic pregnancies, especially the tubal type, go away on their own by just causing an early miscarriage. Nevertheless, when abortion doesn't occur spontaneously, the woman will have no choice but to terminate the pregnancy through surgery or with abortion pills such as Methotrexate.
The treatment of choice will be determined after a series of diagnostic and based on the symptoms described by the patient. Your physician should inform you in detail about the pros and cons of each treatment option.
In cases of ruptured ectopic pregnancies and shock, more challenging treatments may be required, such as a blood transfusion or even a salpingectomy in case the tube is severely damaged.
FAQs from users
Is there a risk of ectopic pregnancy in an AI?
An ectopic pregnancy is nothing more than a gestation that nests inappropriately in the fallopian tubes, which implies a medical emergency that may require surgical treatment, in addition to having consequences on the reproductive health of women.
This is due to the fact that the fallopian tubes -of much smaller diameter and resistance than the uterus- are not prepared to host a pregnancy and, with the development of the embryo in this area, a rupture of this tissue, which has a lot of blood supply, can be generated. This would trigger a hemorrhage that could pose a great risk to the woman.
Artificial insemination is a simple and minimally invasive assisted reproduction treatment, which can be ideal when the causes of reproductive problems are due to the male factor. In this treatment, the sperm -previously prepared- is basically introduced into the uterus in order to promote pregnancy. In most cases, the woman is also usually given medication to help promote ovulation.
All assisted reproduction treatments carry a slightly increased risk of ectopic pregnancy, and artificial insemination is no exception. The causes for this type of pregnancy are not entirely clear, but the most widely accepted are the following: firstly, the fact of injecting the sperm directly into the uterus could affect the peristalsis of the tubes (movement of the tubes that moves the ovum from the ovary to the uterus), causing it to function inadequately and not be able to transport the fertilized ovum to the uterus. The other cause may be that there is a pathology in the tubes that partially occludes them, enough to allow the passage of the sperm, but subsequently does not allow the passage of the fertilized embryo.
Why do ectopic pregnancies occur?
Ectopic pregnancy occurs when the embryo implants outside the endometrial cavity. When this happens, in most cases, the implantation occurs in the fallopian tube, although it can also be seen in other locations such as the ovary, cervix and even the abdomen.
There are different factors that increase the risk of this occurring: history of pelvic inflammatory disease, previous ectopic pregnancy, previous cesarean section, endometriosis, IUD, contraceptives with only gestagens, postcoital pill and assisted reproduction techniques.
Is there an increased risk of ectopic pregnancy after tubal ligation?
All contraceptive methods have a risk of pregnancy occurring during use. Among the contraceptive methods available, tubal ligation is the most effective. The treatment consists of blocking the uterine tubes to prevent the union of egg and sperm.
Although it may be thought that the uterine or Fallopian tubes are merely a tunnel through which the sperm, egg and embryo pass, this is not true. The uterine tubes have several functions, its tissue helps the movement of the sperm and the egg so that they come together in its outermost third, secretes nutritional molecules that establish an optimal environment for the development of the embryo and then helps the embryo formed to move into the uterus where it will finally implant.
When a tubal ligation is performed, it is possible that it will reopen and spontaneously recanalize. This will hinder the movement of the embryo to the interior of the uterus, so the embryo can be trapped in the tube, implanting inside it and developing a pregnancy outside the uterus called an ectopic pregnancy.
At how many weeks can ectopic pregnancy be detected?
With the beta-hCG hormone blood test, ectopic pregnancy can be suspected as early as 5 weeks gestation if there is no normal increase in this hormone, which should be doubled approximately every 48 hours.
Is the presence of pseudosaccharide always related to ectopic pregnancy?
A pseudosac refers to an image obtained by ultrasound, which is relatively round and can be located within the uterine cavity or external to it in the case of an ectopic pregnancy.
This image will not always be observed in cases of extrauterine pregnancy, since no image may be observed, only the presence of free fluid or even the complete gestational sac with germinal vesicle, and when the ectopic gestation is greater than 6 weeks, an embryo with fetal heart rate may be visualized.
Can an ectopic pregnancy go to term?
The answer is yes, although worldwide there have been very few successful cases of babies being born from ovarian and abdominal ectopic pregnancies. However, an ectopic pregnancy can be very dangerous for the mother and doctors recommend abortion as soon as possible.
How long does an ectopic pregnancy last?
An ectopic pregnancy does not go beyond the first trimester. Normally, patients begin to bleed and have severe discomfort in the 6th or 7th week of gestation, which causes them to miscarry or leads them to go to the hospital for a diagnosis. As soon as the extrauterine pregnancy is confirmed, it must be eliminated with chemotherapeutic drugs or surgery.
Recommended readings
A quantitative beta-hCG blood test helps detect ectopic pregnancies, as we have seen above. The following guide to normal beta-hCG levels during pregnancy may help you understand what's considered normal and what's not: What Are Normal hCG Hormone Levels during Pregnancy?
Does an ectopic pregnancy affect future fertility? This is a frequently asked question from women who have gone through an ectopic pregnancy or miscarriage. Check out this for information: Pregnancy After a Miscarriage or Abortion – When to Conceive Again.
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
Alalade AO, Smith FJE, Kendall CE, Odejinmi F. Evidence-based management of non-tubal ectopic pregnancies. J Obstet Gynaecol. 2017 Nov;37(8):982-991. (View)
Brady PC. New Evidence to Guide Ectopic Pregnancy Diagnosis and Management. Obstet Gynecol Surv. 2017 Oct;72(10):618-625. (View)
Hendriks E, Rosenberg R, Prine L. Ectopic Pregnancy: Diagnosis and Management. Am Fam Physician. 2020 May 15;101(10):599-606. (View)
Kellie Mullany, Madeline Minneci, Ryan Monjazeb, Olivia C Coiado. Overview of ectopic pregnancy diagnosis, management, and innovation. Womens Health (Lond). 2023 Jan-Dec;19:17455057231160349 (View)
Milena Leziak, Klaudia Żak, Karolina Frankowska, Aleksandra Ziółkiewicz, Weronika Perczyńska, Monika Abramiuk, Rafał Tarkowski, Krzysztof Kułak. Future Perspectives of Ectopic Pregnancy Treatment-Review of Possible Pharmacological Methods. Int J Environ Res Public Health. 2022 Oct 31;19(21):14230 (View)
Parker VL, Srinivas M. Non-tubal ectopic pregnancy. Arch Gynecol Obstet. 2016 Jul;294(1):19-27. (View)
Rana P, Kazmi I, Singh R, Afzal M, Al-Abbasi FA, Aseeri A, Singh R, Khan R, Anwar F. Ectopic pregnancy: a review. Arch Gynecol Obstet. 2013 Oct;288(4):747-57. (View)
Taran FA, Kagan KO, Hübner M, Hoopmann M, Wallwiener D, Brucker S. The Diagnosis and Treatment of Ectopic Pregnancy. Dtsch Arztebl Int. 2015 Oct 9;112(41):693-703; quiz 704-5. (View)
Xiao C, Shi Q, Cheng Q, Xu J. Non-surgical management of tubal ectopic pregnancy: A systematic review and meta-analysis. Medicine (Baltimore). 2021 Dec 17;100(50):e27851. (View)
FAQs from users: 'Is there a risk of ectopic pregnancy in an AI?', 'Why do ectopic pregnancies occur?', 'Is there an increased risk of ectopic pregnancy after tubal ligation?', 'How do you know if you have an ectopic pregnancy?', 'At how many weeks can ectopic pregnancy be detected?', 'Is the presence of pseudosaccharide always related to ectopic pregnancy?', 'Can an ectopic pregnancy be saved?', 'Can an ectopic pregnancy go to term?', 'How does bleeding from ectopic pregnancy look like?' and 'How long does an ectopic pregnancy last?'.
Authors and contributors
More information about Cristina Algarra Goosman










Hello, I’m 8 weeks pregnant but nothing could be seen in two ultrasound tests…. Doctor said it was outside the uterus so i’m having an ectopic pregnancy… I don’t want to lose this pregnancy… What are the chances for the baby to survive? Pls, help.
Hello MaryLe,
An ectopic pregnancy is a non-viable pregnancy and there’s no option for you but to terminate the pregnancy. Otherwise, it can lead to serious complications for your health. Depending on the cause, it can be removed with medications such as Methotrexate or keyhole surgery.
I hope this helps,
Best wishes