In in vitro fertilization (IVF) treatments, whether conventional IVF or ICSI, the embryos are cultured in the laboratory for a few days in order to decide which one(s) will be transferred to the uterus and which ones will be frozen (vitrified). In order to make the decision, its quality must be assessed during all stages of embryonic development.
Depending on the day of development of the embryo, embryologists analyze different characteristics to determine their quality and if they are capable of implantation to give rise to a pregnancy. If, the embryos are of poor quality, they could stop their development, cause implantation failure or even cause an abortion in the first months of pregnancy.
In the in vitro fertilization laboratory, the embryos spend a maximum of 6 days in culture, going from being a 1-day-old zygote to a 5 or 6-day-old blastocyst with a multitude of cells.
Provided below is an index with the 7 points we are going to expand on in this article.
- 1.
- 2.
- 2.1.
- 2.2.
- 2.3.
- 2.4.
- 2.5.
- 3.
- 3.1.
- 3.2.
- 3.3.
- 4.
- 4.1.
- 4.2.
- 4.3.
- 4.4.
- 4.5.
- 4.6.
- 4.7.
- 4.8.
- 5.
- 6.
- 7.
How and why is embryo quality measured?
In IVF-ICSI processes, in which egg fertilization takes place in the laboratory, it is important to assess the quality of the resulting embryos.
It is common for more than one embryo to be obtained, so its classification helps to choose which of the embryos in culture are most likely to implant and result in pregnancy. Thus, the embryo classification will be taken into account for the transfer, since the highest quality embryos will be those that will be introduced into the uterus.
Evaluation of the quality of embryos requires taking into account different characteristics of their morphology, i.e. their shape or appearance, and the evolution over the days they remain in culture. In order to do this, there are two options:
- Remove the embryos from the incubator every day for a few minutes so that they can be evaluated under a microscope.
- Valuate the embryos by means of a time-lapse system, which allows images to be obtained every few minutes in order to evaluate their complete development without removing them from the incubator.
The first alternative is the traditional method, while the second is a recent addition to assisted reproduction laboratories. The use of time-lapse systems allows the embryologist to observe the entire embryonic development, not just the specific moments when the observation would be made under the microscope. It also avoids the temperature and gas changes that occur when embryos are removed from the incubator, reducing stress and improving embryo viability.
First days of embryonic development
Either by direct visualization under the microscope or with the time-lapse system, embryos are evaluated almost every day until they are transferred or frozen.
Depending on the day, embryologists will have to look at different aspects of embryo morphology in order to classify them.
Next, let's talk about these developmental days and what the embryos are expected to look like.
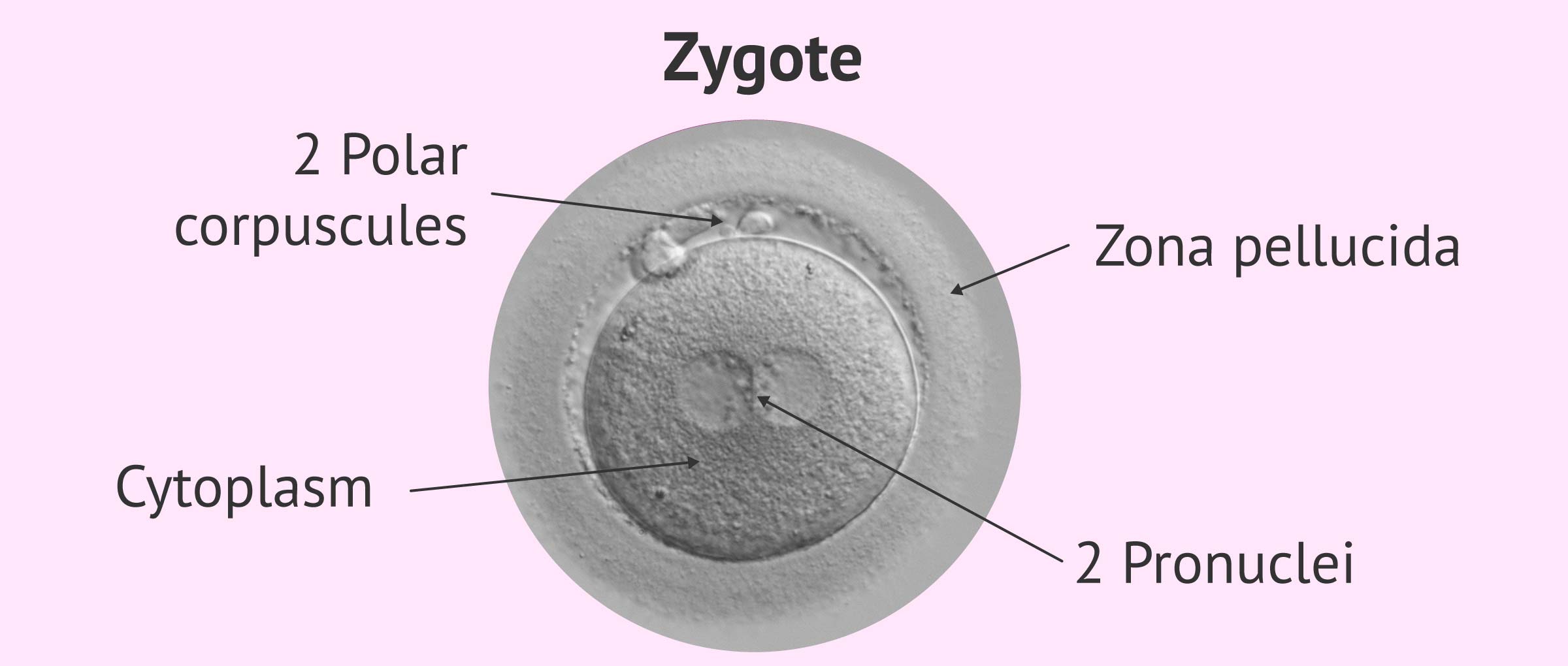
Embryo on day 1: zygote
The day after fertilization (day 0) it is necessary to confirm whether the eggs have fertilized with the appearance of the first embryonic stage: the zygote or zygote.
This is a single cell that has not yet begun to divide and in which the following should be observed:
- The presence of two pronuclei (PN), one from the egg and the other from the sperm.
- The presence of two polar corpuscles (CP), indicating that after fertilization the meiosis of the ovum has been completed.
- The appearance of the cytoplasm of the zygote, which should be uniform and clear.
To avoid misinterpretation, it should be observed between 16 and 18 hours after in vitro insemination or microinjection (postinsemination). If they are observed later, the pronuclei may have disappeared, an event necessary for the first division to take place, which will give rise to the two-cell embryo.
The existence of the 2 PNs confirms that there has been fertilization. If 1 or 3 pronuclei are observed, the embryo should be discarded, as it indicates that the genetic endowment of the embryo is not adequate. Their development in the next few days occurs in the same way as in viable embryos, so it is important to visualize them before PN fusion occurs and we are not able to distinguish viable from non-viable embryos.
Embryo on day 2: four cells
After the first two divisions (day 2 of development), the embryo must have 4 cells, called blastomeres. Both the number of blastomers and their appearance at this point in time will be decisive in the classification. Observing fewer than 4 cells or many more is indicative of delayed or accelerated development.
The observation of embryos at this stage of development should be done between 44 and 45 hours postinsemination paying attention mainly to the following aspects:
- Size and symmetry of the blastomeres: the 4 cells should be approximately equal in size.
- Number of cells: each cell must have only one nucleus. If they have two, they would be binucleated, and if they have more than two, they would be multinucleated. If they have more than one nucleus they are considered abnormal and are associated with cell division errors.
- Percentage of fragmentation: the fragments are small traces of cytoplasm from an abnormal division of the blastomeres. The quantity, distribution and volume of the fragments are important, as they can compromise the development of the embryo.
- Presence of vacuoles: vacuoles are like "sachets" filled with liquid. If they are large or numerous, they can have a negative influence on embryo quality.
- Shape and thickness of the zona pellucida: it should be round and not too thick or too thin. Alterations in the zona pellucida are associated with low implantation rates, as it will be difficult for the embryo to detach from it in order to implant.
Some of the embryonic alterations influence the implantation capacity of the embryo to a greater or lesser extent so that one quality category or another will be assigned according to this.
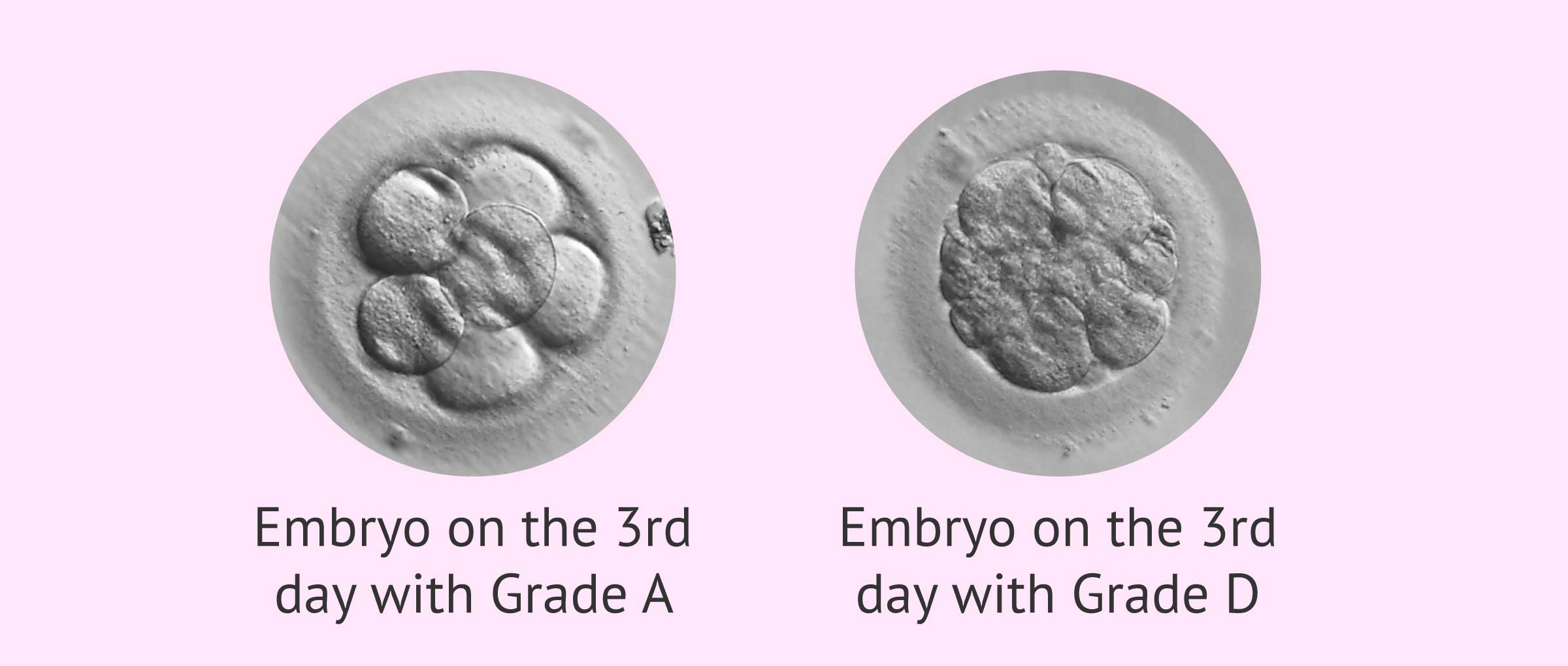
Embryo on day 3: eight cells
To analyze embryo quality on day 3, embryos are assessed between 68 and 69 hours postinsemination. At this moment, the same parameters that have been considered on day 2 of development are analyzed, as well as the rhythm of division.
The best quality embryos would be those with 7-8 cells proceeding from 4-cell embryos on day 2.
Embryos can be transferred at this time of development or kept in the incubator until day 5 or 6 for blastocyst stage transfer. Also, embryos that are not transferred can be vitrified at this time or on day 5 or 6.
Related post: Day 5 vs. Day 3 Embryo Transfer- Pros & Cons.
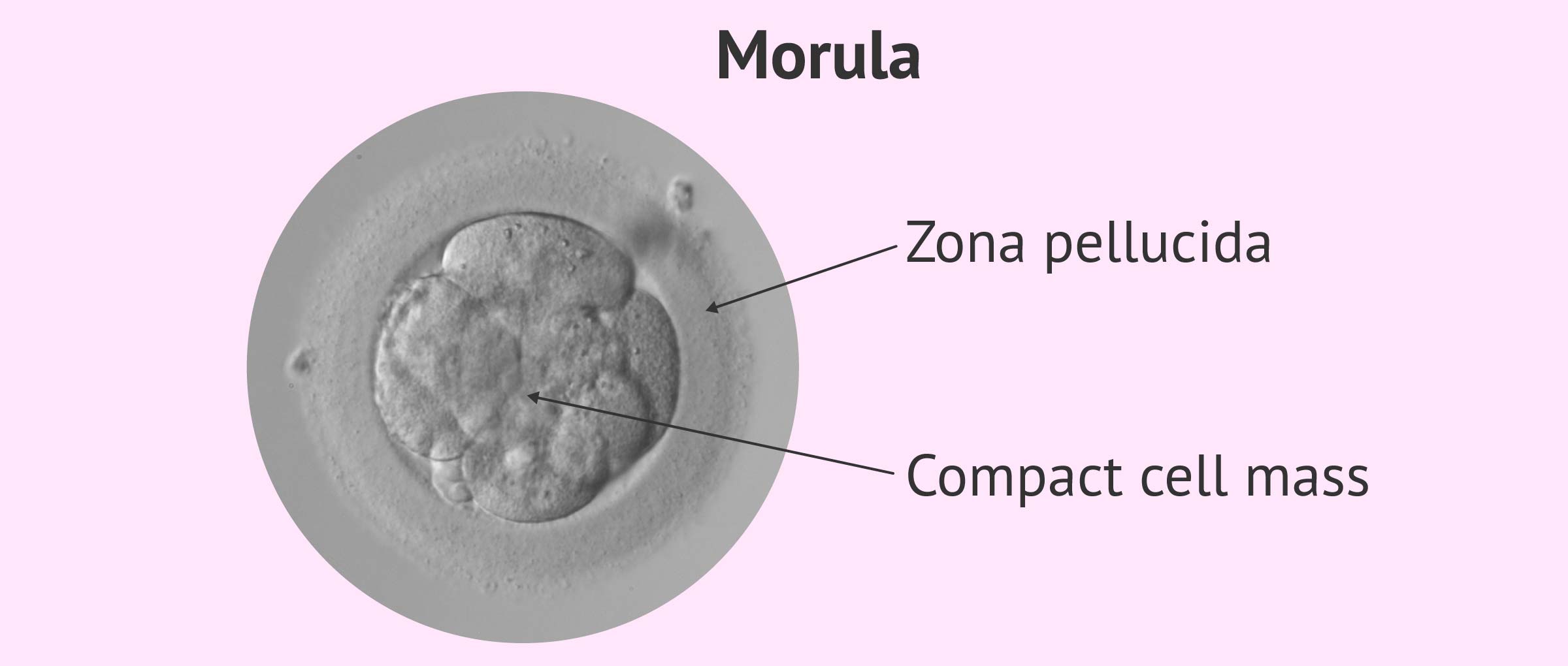
Embryo on Day 4: Morula
Compaction is the process by which embryonic cells form tight joints between themselves to form the morula. It is usually produced from the fourth day of development, although some embryos may show signs of the beginning of early compaction (on day 3).
The morula can be observed between 90 and 94 hours postinsemination. This moment provides little information about the state of the embryo since all its cells have been compacted and it is not possible to observe distinctive features in these embryos.
Nevertheless, the following aspects are valued:
- Number of cells: the embryo must have more than 8 cells.
- Degree of compaction: if compaction takes place at an early stage, cell membrane junctions are observed but can be distinguished from each other, while if it is advanced it is no longer possible to distinguish one cell from another. The compaction must be complete, i.e. it must affect all the cells of the embryo. If it is partial it means that some cell has been excluded and it is a sign of a bad prognosis.
- Fragments and vacuoles: If one of these two structures is observed, the embryo or part of it may be degenerating.
The optimal embryo on day 3 is the one with the following characteristics: it has more than 8 cells, it is compacted or compacting and the compaction affects the whole volume of the embryo.
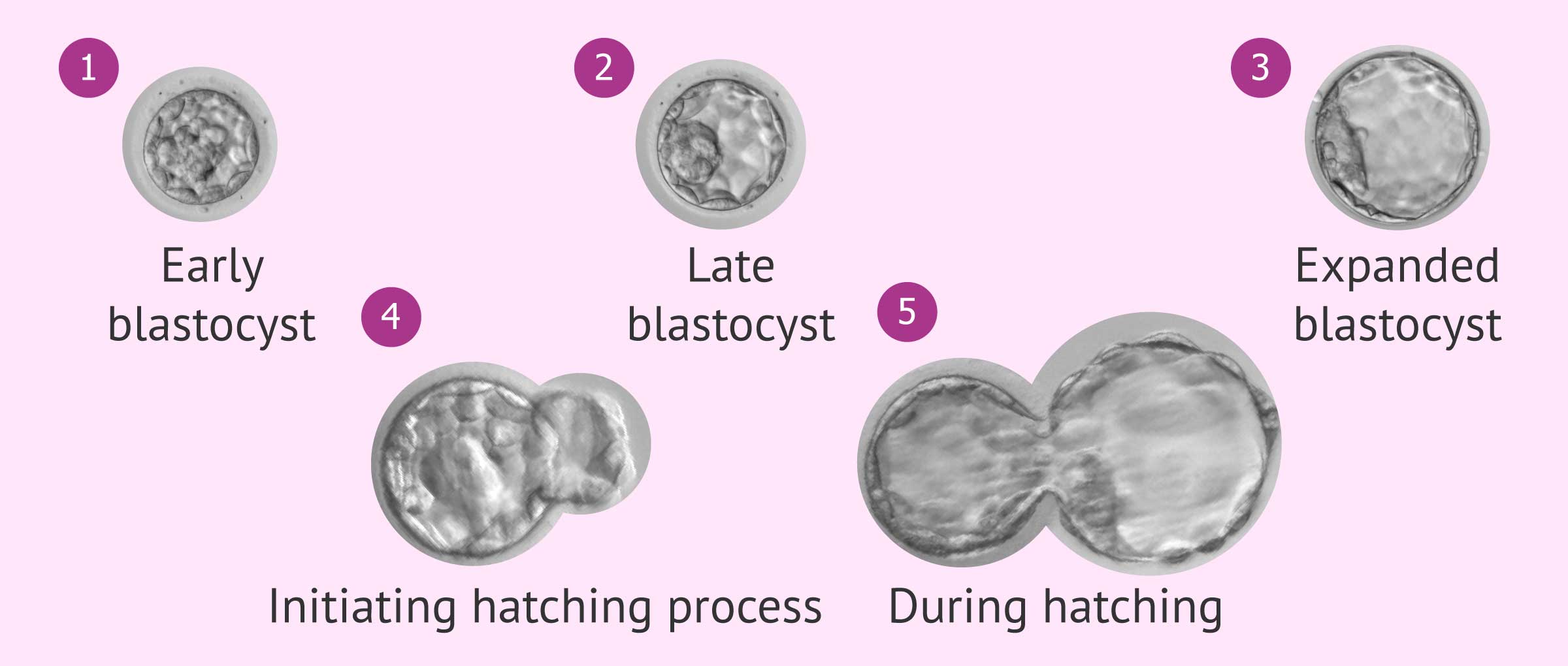
Embryo on day 5 or 6: blastocyst
Between 114 and 118 (day 5) or 136-140 hours postinsemination (day 6) we are faced with a blastocyst, the last stage of embryonic development that can take place in the laboratory.
The formation of the blastocyst is essential for the implantation of the embryo in the uterus to take place, so its formation in culture is considered to have a good prognosis.
These embryos present two key structures in their morphology:
- The inner cell mass (ICM)
- will originate the embryonic layers that will give rise to the baby's organs
- The trophectoderm or external cell mass
- will originate the placenta.
Both structures are distinguished by the appearance of the blastocoel: the central cavity filled with fluid.
Parameters similar to those proposed by Gardner in 1998 are taken into account to assess the quality of blastocysts:
- The degree of expansion: from lowest to highest degree, from 1 to 5.
- The state of ICM: size, shape and compaction of the internal cell mass. Valuation is done by assigning 4 letters (A, B, C, D).
- The state of the trofoectoderm: structure and number of cells. Valuation is done by assigning 4 letters (A, B, C, D).
The thickness of the zona pellucida is also taken into account. It must become thinner to allow the blastocyst to expand and exit for implantation into the endometrium. A fine zona pellucida is related to good embryonic quality and a high probability of implantation.
Categories of embryo quality
Currently, embryos are classified by categories according to their morphogenetic quality.
Both day 3 embryos and blastocysts can be classified, but in a different way, since the embryonic structure is also different in both stages.
Quality of early embryos
The following quality grades are assigned to the embryos on day 2 and day 3 according to the different parameters mentioned in the previous section:
- Category A or 1: embryos of excellent quality, with maximum implantation capacity.
- Category B or 2: embryos of good quality, with high implantation capacity.
- Category C or 3: embryos of intermediate quality with medium implantation capacity.
- Category D or 4: poor quality embryos with low implantation capacity.
Quality of blastocysts
In order to assess blastocysts, as we have already seen, the usual embryonic classification has a number and 2 letters: the number (from 1 to 5) indicates the degree of expansion of the blastocyst; the first letter (A, B, C or D) indicates the quality of the internal cell mass; and the second (A, B, C or D), that of the trofoectoderm. Thus, the blastocysts with the best morphology and the highest implantation capacity would be the 3AA.
The numerical categories assigned according to the expansion are the following:
- Grade 1 or early blastocyst: the blastocele begins to become visible.
- Grade 2 or cavitated blastocyst : the different parts of the blastocyst are perfectly visualized.
- Grade 3 or Expanded Blastocyst : The blastocyst has increased in size and the zona pellucida is thin.
- Grade 4 or blastocyst hatching: the blastocyst begins to leave the zona pellucida.
- Grade 5 or blastocyst hatching: the blastocyst begins to leave the zona pellucida.
As for the internal cell mass, the 4 categories would be as follows:
- Category A: numerous cells forming a compact structure.
- Category B: numerous non-compacted cells.
- Category C: few cells.
- Category D: cells with signs of degeneration.
On the other hand, the trofoectoderm must have only one layer. According to the state of its cells, it is classified as follows:
- Category A: homogeneous, cohesive and with many cells.
- Category B: homogeneous and with fewer cells.
- Category C: few cells.
- Category D: cells with signs of degeneration.
The embryologist Jose Luis De Pablo tells us what is taken into account when assessing blastocysts:
In the blastocyst, two fundamental parts are valued: the internal cell mass, which will give rise to the embryo, and the trofoectoderm, the layer of cells that will give rise to the placenta.
Depending on the number of cells, the compaction of the internal cell mass, and the disposition of these cells, the final category of the blastocyst will be given.
New cataloguing of blastocysts
The Association for the Study of Reproductive Biology (ASEBIR) has proposed a new embryonic classification that gives greater weight to the morphology of the trophectoderm with respect to that of the internal cell mass.
In it, the quality is assigned with a single letter (A, B, C, or D) that encompasses the state of both the internal cell mass (ICM) and the trophectoderm. Thus, if the ICM is of quality A and the trophectoderm is of quality B, the overall assessment of the blastocyst would be B.
In both the conventional and the new cataloging, if embryos are taken to long culture for blastocyst stage transfer, it will be necessary to take into account the early stage classification (days 2 and 4) as well as that presented on day 5/6 for its overall assessment.
It is also important to bear in mind that embryo assessment is often very subjective, so there may be variations between laboratories.
FAQs from users
What does the term early blastocyst refer to?
The blastocyst stage is characterized because the cells are arranged in such a way that in one area of the embryo a cellular group accumulates, which is called the inner cell mass and will give rise to the embryo and the fetus that we will later see in the ultrasound scans. While the rest of the embryo is surrounded by a row of cells that will give rise to the membranes and the placenta, which we call the trophoectoderm. And in the central area there is an area without cells with a liquid inside, which is called the blastocele and which will give rise to the amniotic fluid.
The difference between an early blastocyst and an expanded blastocyst is that, in the first case, the separation of these three parts begins to be intuited, initially appearing the blastocele which differentiates two cell groups, one that will give rise to the inner cell mass and the other to the trophoectoderm. At this stage the blastocyst is not clearly expanded and therefore the zones are not clearly differentiated. This embryonic stage usually begins to be seen at the end of the fourth day or at the beginning of the fifth day.
Read more
How much likely is pregnancy with 2 embryos of A quality?
It is a high probability as long as the other factors involved are correct (endometrium, transfer...). We can conclude that the pregnancy rate for these embryos can exceed 70% when the conditions are correct.
Which quality does an embryo II with 8 cells have on day 3?
It would correspond to an embryo of 8 cells of category II or B, so it is of good quality, although not excellent. The implantation rates of these embryos are high, so there would be a high probability of pregnancy.
Is it possible to do a D-grade embryo transfer?
These types of embryos have a low probability of implanting, as their quality is poor. They have signs of degeneration, serious morphological alterations such as high fragmentation or vacuolization, or an abnormal division rhythm. It is advisable to avoid transferring this type of embryos but if there is no other of better quality they can be transferred. Even if the possibilities are low, they could lead to pregnancy.
What quality does an embryo have to have in order to be frozen?
Not all embryos are capable of surviving the processes of freezing and thawing. The best quality embryos have higher survival rates, so it is preferable to freeze those of quality A and B, although it is also possible to freeze those of type C. However, if the couple does not have better quality embryos, even type D embryos can be frozen, but this is not done in all centers because of their low survival chances. In most cases what is done with poor quality embryos is to leave them until day 5-6 in culture (under "observation") to see how they evolve.
Is the quality of an 8-cell or 6-cell embryo higher?
The optimal embryos on day 2 are those with 4 cells, while on day 3 are those with 8 cells. Having more or fewer cells, as we have seen throughout the article, assumes that the embryo is not of excellent quality.
In the case of having 6 cells, the embryo would be classified in category C, whether it is day 2 or day 3. In the case of having 8 cells, it will be necessary to assess how many there were on day 2. Thus, if it comes from an embryo with 4 cells on day 2, it will be of quality A, while if it had 6 cells it will be of category C. If it comes from an embryo with 4 cells on day 2, it will be of quality A, while if it had 6 cells it will be of category C.
Will AA quality embryos always lead to pregnancy?
This type of classification corresponds to a blastocyst of excellent quality, with an internal cell mass and a good looking trofoectoderm. It has a high implantation capacity and, therefore, a high probability of giving rise to a pregnancy. However, there is no guarantee that a woman will become pregnant. The fact that the embryo quality is good has a great influence on the implantation, but other factors such as the state of the endometrium at the time of the transfer, the age of the mother or the cause of infertility are also affected.
What causes poor embryo quality?
There are several factors, both intrinsic and extrinsic, that can influence embryo quality:
- Advanced maternal age
- Endometriosis
- Severe male factor
- Polycystic ovary syndrome
- Obesity
- Stimulation protocols
- Cultivation conditions
That being said, it is difficult to know the specific cause that could affect a particular case in women with good prognosis and good reproductive health.
Recommended reading
If you want to learn more about the criteria followed by embryologists to establish embryo quality, do not miss the following post: Embryo quality and grading - Does it affect IVF success?
On the other hand, blastocysts are the embryos with the highest implantation capacity due to their high degree of development. If you want to know more about them, you can continue reading here: What is long embryo culture and blastocyst grading?
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
Abeyta M, Behr B. Morphological assessment of embryo viability. Semin Reprod Med. 2014 Mar;32(2):114-26.
Amorocho B, Gómez E, López D, Santana A, Martinez JC, Landeras J. Cultivo prolongado del embrión hasta blastocisto: cultivo secuencial. In J Remohí, A Cobo, JL Romero, MJ de los Santos, A Pellicer (eds) Manual Práctico de Esterilidad y Reproducción Humana. Laboratorio de reproducción asistida. 2008. Editorial McGraw-Hill / Interamericana de España, S.A.U. 3ª edición, pp.225 - 230.
Glujovsky D, Farquhar C, Quinteiro Retamar AM, Alvarez Sedo CR, Blake D. Cleavage stage versus blastocyst stage embryo transfer in assisted reproductive technology. Cochrane Database Syst Rev. 2016 Jun 30;(6):CD002118.
Lundin K, Ahlström A. Quality control and standardization of embryo morphology scoring and viability markers. Reprod Biomed Online. 2015 Oct;31(4):459-71.
Mercader A, Buendía P, Gámiz P, Albert C. Valoración morfológica del blastocisto. In J Remohí, A Cobo, JL Romero, MJ de los Santos, A Pellicer (eds) Manual Práctico de Esterilidad y Reproducción Humana. Laboratorio de reproducción asistida. 2008. Editorial McGraw-Hill / Interamericana de España, S.A.U. 3ª edición, pp. 231 - 236.
Meseguer M, Herrero J, Tejera A, Hilligsøe KM, Ramsing NB, Remohí J. The use of morphokinetics as a predictor of embryo implantation. Hum Reprod. 2011 Oct;26(10):2658-71.
FAQs from users: 'What does the term early blastocyst refer to?', 'How much likely is pregnancy with 2 embryos of A quality?', 'Which quality does an embryo II with 8 cells have on day 3?', 'Is it possible to do a D-grade embryo transfer?', 'What quality does an embryo have to have in order to be frozen?', 'Is the quality of an 8-cell or 6-cell embryo higher?', 'Will AA quality embryos always lead to pregnancy?' and 'What causes poor embryo quality?'.
Authors and contributors

More information about Cristina Algarra Goosman

More information about Michelle Lorraine Embleton







Hi, I am in the middle of an IVF process and after the puncture and everything 4 C quality embryos have survived. Since the embryos are of such poor quality, is it worth doing the transfer?
Hello Alicenelson,
Even if the embryos have been graded with C quality there is a chance that they will implant in the uterus. The technicians have observed the development and can judge the viability of the embryo. Based on their experience and recommendation they will tell you whether or not to continue with the cycle.
I hope I have helped you,
Best regards
Hello, I have undergone ovarian stimulation and I do not have embryos yet but I am very interested to know, only A or B quality embryos would be good, right?
Hi Kasie,
The classification of embryos by quality is done after observation at different stages, i.e. when they are zygote, the embryo (4, 8 cells), morula, and blastocyst.
Being day 2 or 3 of development when they are assigned a classificatory label based on their quality and implantation capacity. At this point is where the letters A, B, C, and D appear, the first one being of optimum quality and the last one of poor quality.
Subsequently, in the blastocyst stage, another observation is made that evaluates the degree of expansion, the internal cell mass, and the cell mass of the trophectoderm.
Therefore, if the embryos in the initial stage have a C or D quality it does not mean that there is a possibility that in the rest of the embryonic development it can improve and establish a viable embryo for an evolutionary pregnancy.
I hope I have helped you,
Best regards
Hi… I had my ET on 29/06/2016 at 8.30 am. 13 Days after when I checked my BETA HCG the result was only 34.6 and the doctor said that it is a negative result. Embryologist’s opinion about the embryos used for ET is that they were in ‘A’ grade. Unfortunately, the result was negative. Why did this happen? I need an advise from you for the successful implantation on my next embryo.