In vitro fertilization (IVF) refers to the union of the woman's egg and the man's sperm in the laboratory with the aim of generating embryos.
The procedure for conventional IVF and IVF with intracytoplasmic sperm injection (IVF-ICSI) is the same, except for one of the steps: the union of the egg and the sperm. For this reason, this article will detail each of the steps necessary to carry out IVF in general.
On the other hand, the IVF process does not change if it is carried out in a private clinic or in Social Security. The only difference will be the waiting times and the cost of the treatment.
Provided below is an index with the 6 points we are going to expand on in this article.
- 1.
- 1.1.
- 1.2.
- 1.3.
- 1.4.
- 1.5.
- 1.6.
- 1.7.
- 1.8.
- 1.9.
- 1.10.
- 2.
- 3.
- 3.1.
- 3.2.
- 3.3.
- 3.4.
- 3.5.
- 3.6.
- 4.
- 5.
- 6.
What does the IVF process consist of?
In vitro fertilization means fusing gametes (eggs and sperm) in the laboratory to create embryos that will later be transferred to the woman's uterus to achieve a pregnancy.
Prior to the union of the gametes, it is necessary to follow a series of steps. Next, each one of them is detailed.
Controlled ovarian stimulation
Ovarian stimulation consists of the administration of specific hormones to women with two main purposes:
- Ensure that all the ovules that initiate growth in this cycle reach the final stage of maturation. In the natural cycle of the woman, only one of the ovules reaches the final stage of maturation, which will be released at the ovulation stage. Therefore, the greater the quantity and quality of ovules, the greater the probability of obtaining embryos, and the pregnancy rate will increase.
- Control the ovarian cycle and know approximately when the ovules are mature and, therefore, when ovulation will occur. This increases the chance of success.
There are several medical protocols to stimulate the ovary, although they generally consist of the administration of gonadotropins and GnRH analogs. The doctor will establish the most appropriate treatment for each patient.
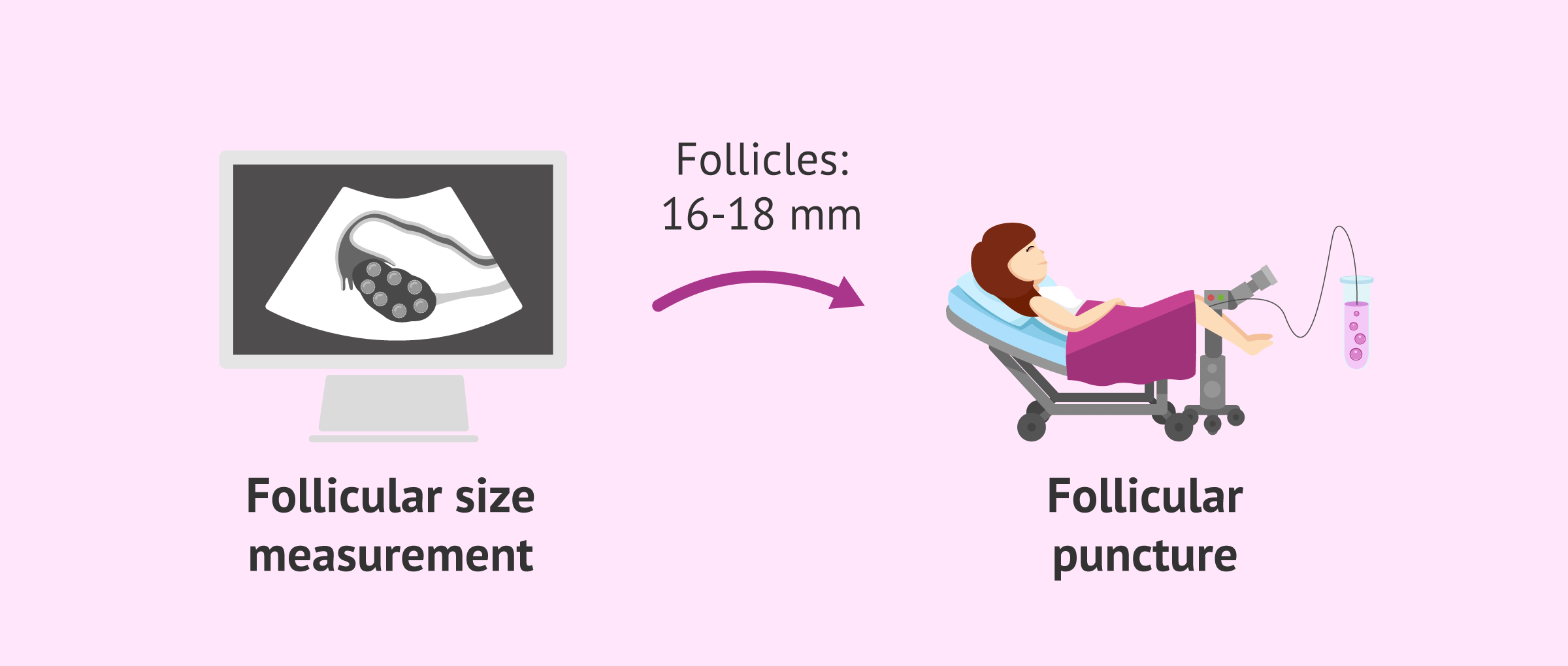
Normally, ovarian stimulation lasts 6-10 days, during which time it will be necessary for the patient to visit a regular doctor every 2 or 3 days. Thus, the specialist will control the evolution of the ovary and will be able to program the puncture at the right time, that is, when the ovarian follicles reach a size of 16-18 mm.
In the words of Elena Martín Hidalgo, MD, controlled ovarian stimulation is just a process whereby the hormones that typically participate in the reproduction process are administered artificially. According to Dr. Martín Hidalgo, this process can last up to 14 days on average, depending on each case.
Check out this for more information: Ovarian Stimulation Protocols for IVF – Process & Medications Used.
Follicular puncture
Once the ovarian follicles reach the desired size, the next step is to obtain the ovules by follicular or ovarian puncture. It is a surgical intervention performed under anesthesia in which the gynecologist punctures the follicles of the ovary ("bags" that contain the ovules) and aspirates their content. Subsequently, the aspirated follicular fluid will be analyzed in the laboratory in search of the ovules.
This process lasts about 30 minutes and the patient does not feel pain. In addition, the woman can go home when the ovarian puncture is finished, so she does not require hospitalization.
If you want to know more about follicular puncture, you can visit this article: Ovum Pick-Up Procedure: How Are Eggs Harvested in IVF?
Collection and preparation of semen
Generally, the sperm sample is obtained by masturbation and requires an abstinence period of 3-5 days. A few minutes after ejaculation, the sample goes through a process is known as sperm capacitation which consists of removing poor quality sperm and seminal plasma. Thus, the sample is concentrated in spermatozoa with progressive mobility.
In cases in which masturbation does not allow sperm to be obtained, the sample can be obtained by testicular biopsy or epididymal aspiration. These types of samples require fertilization through the ICSI method, due to the low quantity and poor quality of the sperm.
Fertilization or fusion of the gametes
Fertilization refers to the moment in which the egg and sperm fuse to join the genetic endowment of both parents and give rise to the new being. The union can occur with more or less the intervention of the embryologist. However, in general, it works as follows:
- Conventional IVF
- The embryologist simply places the ovules and the sperm in the same culture plate, waiting for the latter to be able to penetrate the ovule.
- ICSI
- The embryologist is the one who deposits the sperm directly inside the egg.
In the following article you can read all the differences between these two types of in vitro fertilization: Differences between IVF and ICSI
Checking fertilization
Between 16 and 20 hours after fertilization, the embryologist checks whether the egg has been correctly fertilized or whether there has been an error that has prevented fusion. To do this, he analyzes the presence of the two polar corpuscles (PC) and the two pronuclei (PN), which will fuse to give rise to the zygote (one-cell embryo).
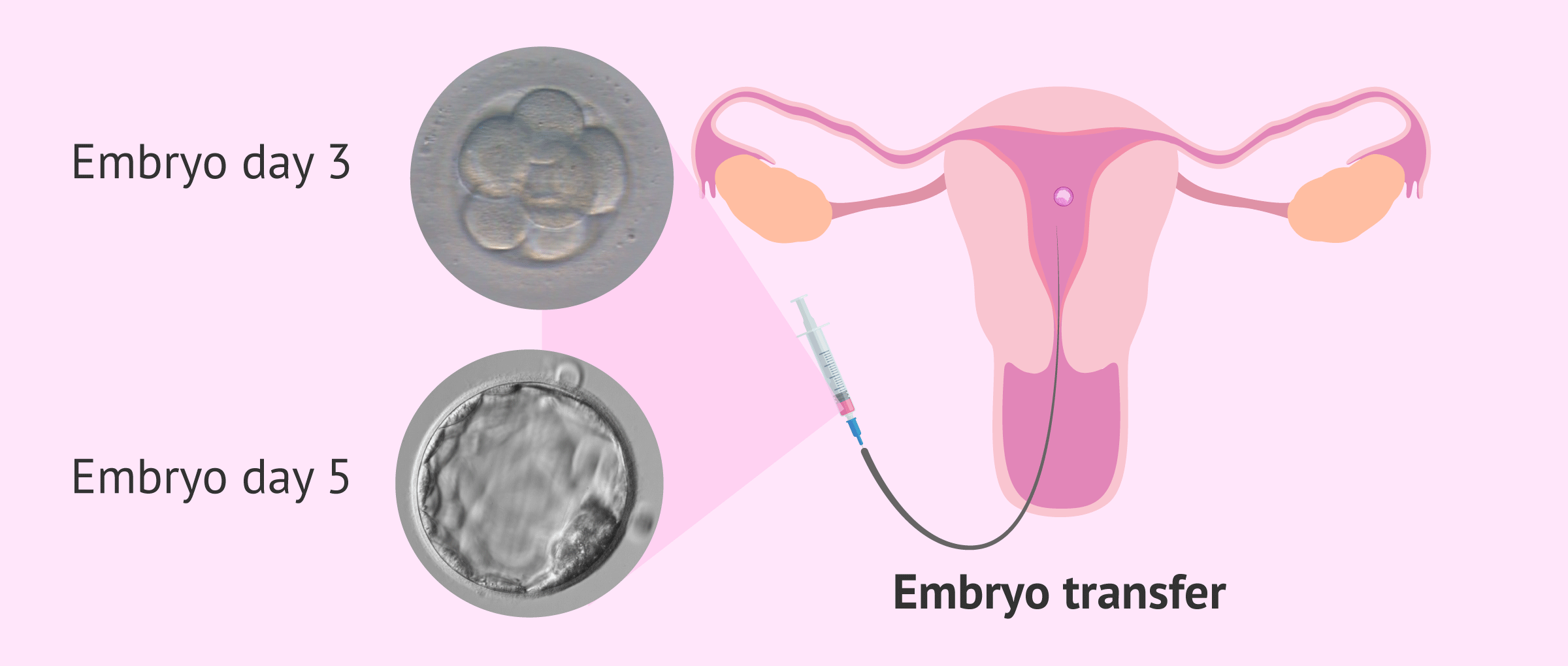
Embryo culture
The zygotes are left in culture to continue their evolution, passing through the embryo and blastocyst stage. These embryos will be left in a specific incubator that maintains the ideal temperature and gas conditions for embryonic growth until the moment of transfer to the mother's uterus. During the time they are in the incubator, their condition will be analyzed and their quality determined.
You can read more by clicking on the following link: Embryo quality for embryo transfer or freezing.
Preparation of the endometrium
The patient will receive hormonal medication other than that for ovarian stimulation to ensure that her endometrium is receptive, that is, it is capable of interacting with the embryo so that it implants and starts the pregnancy.
The endometrium must have a trilaminar appearance and a thickness of approximately 7 to 10 mm to favor embryo implantation.
In most cases, the medication for endometrial preparation consists of estrogen and progesterone. These drugs can be administered vaginally, orally, or as patches.
If IVF is done fresh, the natural release of estrogen is often harnessed and only progesterone is given to support the luteal phase.
Embryo transfer
Based on the quality of the embryos, the best embryo is selected, that is, the one with the greatest implantation potential. This embryo is transferred to the future mother's uterus through a specific cannula, waiting for it to implant in the uterine endometrium and thus produce pregnancy.
The transfer is painless and short-lived. It is a simple process that is carried out by the gynecologist in the office or in the operating room without the need for anesthesia.
We recommend you read this article for more information related to this phase of IVF: Embryo transfer: when and how is it done.
Freezing the embryos
Spanish legislation allows the transfer of a maximum of three embryos, although it is common to have one or in some cases two. However, the number of embryos obtained in an IVF cycle can be higher. For this reason, there are three possible destinations for those embryos of good quality that are not going to be transferred:
- Cryopreservation of embryos for future embryo transfers.
- Embryo donation to other people with fertility problems.
- Embryo donation for research.
The Dr. Miguel Dolz details the possible destinations of these leftover embryos:
Use by the couple themselves to be able to have a second child or to try again if they have not gotten pregnant without having to go through the whole process, donate them for research purposes always subject to legality, donate them with reproductive purposes if the legal requirements are met and, finally, destroy them when the woman's fertile period of life has ended.
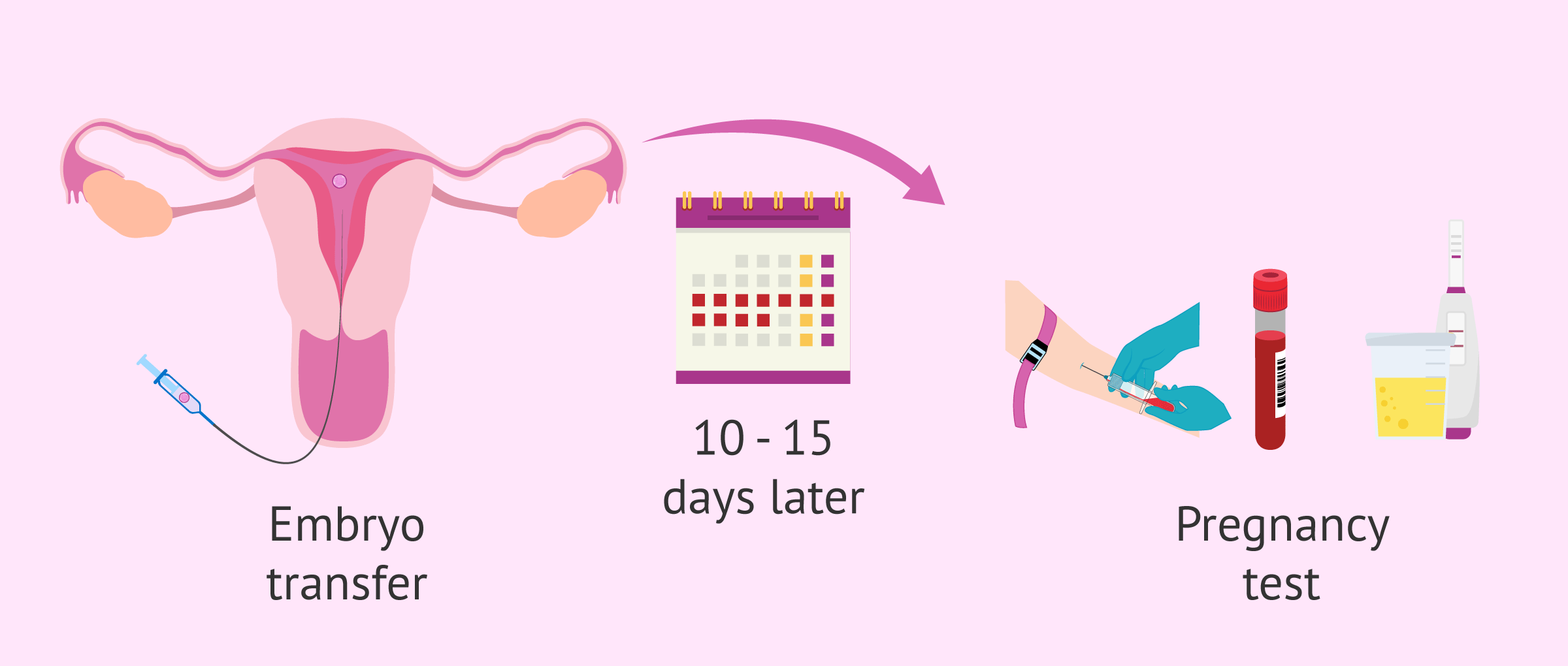
Pregnancy test
Once the embryo transfer has been carried out, the woman must wait between 10 and 15 days to do a pregnancy test and check if the IVF treatment has been successful.
The pregnancy test can be done in both urine and blood. Both techniques are based on the detection of the hormone beta-hCG, known for this as "the hormone of pregnancy". For this reason, the period between the transfer and the pregnancy test is known as "the two-week wait."
How much does IVF cost?
The price of in vitro fertilization varies by country. In the United States, IVF packages using own eggs start from $8,500.
As for the United Kingdom, some patients qualify to get NHS-funded IVF as long as they meet certain criteria established by the NICE (National Institute for Health and Care Excellence). In any case, the cost of an IVF cycle at a private clinic can be £5,000 or more.
Finally, Canadian patients can expect sums of around CAD $7,000 on average if covered by insurance; if you are not, you can expect higher sums. If you are an Ontario resident and have a valid OHIP card, you do not have to pay for fertility treatments.
If you need to undergo IVF to become a mother, we recommend that you generate your Fertility Report now. In 3 simple steps, it will show you a list of clinics that fit your preferences and meet our strict quality criteria. Moreover, you will receive a report via email with useful tips to visit a fertility clinic for the first time.
It is important to keep in mind that pregnancy is not always achieved the first time. For this reason, you should check the cost of undergoing more attempts at the clinic and if they offer any kind of discount.
FAQs from users
Can an IVF cycle be canceled, once started, and not reach the transfer?
Yes, both expected and unexpected. Sometimes, it is known that the woman's ovarian reserve is low, that the seminal quality is poor, or there are other conditions that may determine that an IVF cycle does not go all the way to the end.
However, other times it is not to be expected and at some point in the IVF cycle, it must be canceled.
Are birth control pills always given before fertility treatment?
Not necessarily. An ovarian stimulation cycle can start between the 1st and 4th day of the period without using contraceptives. However, they have many uses in our specialty.
Contraceptives can be given because a follicular cyst (also called a persistent follicle) is observed before performing ovarian stimulation. In this case, they are used for at least 14-15 days to reduce the follicle and leave the ovaries in a basal state, ready to start ovarian stimulation. They are also very useful in patients with endometriosis since, in some cases, they can reduce the symptoms and size of some endometriomas.
One of the main advantages of contraceptives is that they reduce the risk of asynchrony occurring during ovarian stimulation. An asynchrony is nothing more than the accelerated growth of a few follicles and, consequently, a worse result when performing the ovarian puncture. This would cause the collection of many fewer oocytes than would correspond to the patient and a suboptimal result.
Another advantage is that they help plan the start of ovarian stimulation and therefore the distribution of the workload of assisted reproduction centers. However, overusing contraceptives for more than 2 weeks prior to ovarian stimulation may result in a slower response and poorer results.
What are the recommendations after IVF?
Some time ago it was said that after in vitro fertilization, rest should be carried out, for at least two days, since embryo transfers were usually carried out on day 3 of embryonic development, so embryo implantation took place in approximately two days. Thus, it was thought that physical efforts could be counterproductive for the implantation process of some embryos that would naturally be traveling through the fallopian tubes, while in an IVF they would remain free in the uterine cavity.
With the arrival of transfers on day 5, this concept has been gradually abandoned. However, there are still centers that recommend rest to their patients after the transfer, for at least one day.
Currently there are scientific studies that show that no type of rest is necessary after performing IVF. In fact, many international patients fly to their home countries on the same day as the transfer, without lowering their chances of pregnancy.
In this way, a woman can return to her normal life after completing her In Vitro Fertilization, of course, using common sense and avoiding efforts that are not usual for her. For example, the days after IVF should not be used to start activities for which the woman is not already trained and/or to beat sports records.
What is the process of IVF using frozen embryos?
IVF with frozen embryos involves just the endometrial preparation and embryo transfer steps. Ovarian stimulation, follicular puncture, and embryo culture are not required, since the embryos were already created and cryopreserved in previous cycles.
How long does IVF treatment take from start to finish?
In Vitro Fertilization takes approximately a complete female cycle, that is, about 30 days. Since the beginning of the menstrual cycle, marked by the start of menstruation, the intended mother starts stimulating the ovaries. Between 6 and 10 days after that, the follicular puncture for egg retrieval is scheduled. This procedure is used to retrieve the eggs, which will be fertilized in the lab in order to obtain viable embryos. The resulting embryos remain in culture for 3 to 5 days, depending on each case, till they are transferred back to the mother's uterus. At this point, 15 days will have passed since the beginning.
Approximately two weeks after the embryo transfer, the woman can take a pregnancy test to verify whether it has been successful or not.
Is the IVF medication always the same?
No, although the objective of the medication administered is the same, there are different protocols and ways of stimulating the ovary and preparing the endometrium.
Depending on the situation of each woman, the most appropriate medication and dosage for her characteristics are determined. For this reason, it is essential to carry out a good fertility study on the woman prior to the IVF process. It is also important to monitor the response to the indicated medication and to change the type of drug or the dose accordingly.
Recommended Readings
Want to delve deeper into IVF, its differences with artificial insemination, indications, success rates, and more? Then do not miss this guide: What Is In Vitro Fertilization (IVF)? – Process, Cost & Success Rates.
Also, during the feared two-week wait, women experience a series of symptoms and side effects that are often very confusing. Learn more about them here: Symptoms After Embryo Transfer – Most Common Positive Signs.
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
ACE, Association of Clinical Embryologists (2003). Accreditation Standards and Guides for IVF Laboratories.
Alper M, Brinsden PR, Fischer R, Wikland M (2002). Is your IVF program good? Hum Reprod; 17: 8-10 (View)
Bourgain C, Devroey P. The endometrium in stimulated cycles for IVF. Hum Reprod Update 2003;9:515 – 522 (View)
Brian, K. (2010). The Complete Guide to IVF: An Insider’s Guide to Fertility Clinics and Treatments. Published by Hachette Digital, Londres (View)
The Practice Committee of the American Society for Reproductive Medicine and the Practice Committee of the Society for Assisted Reproductive Technology. Criteria for number of embryos to transfer: a committee opinion. Fertil Steril 2013; 99(1):44-6 (View)
Gianaroli L, Plachot M, van Kooij R, Al-Hasani S, Dawson K, DeVos A, Magli MC, Mandelbaum J, Selva J, van Inzen W (2000). ESHRE guidelines for good practice in IVF laboratories. Committee of the Special Interest Group on Embryology of the European Society of Human Reproduction and Embryology. Hum Repro; 15: 2241-6 (View)
Lenton, E. (1993) Natural cycle versus stimulated cycle IVF. /. Assist. Reprod. Genet., 10,406-08.
Mantikou E, Youssef MA, van Wely M, van der Veen F, Al-Inany HG, Repping S, et al. Embryo culture media and IVF/ICSI success rates: a systematic review. Hum Reprod Update 2013;19:210–20 (View)
Mayer J, Jones EL, Dowling-Lacey D, Nehchiri F, Muasher SJ, Gibbons WE, Oehninger SC. Total quality improvement in the IVF laboratory: choosing indicators of quality. Reprod BioMed Online 2003;7:695- 9 (View)
Nijs, M. and Geerst, L. (1993) Prevention of multiple pregnancies in an IVF program. Fertil. Steril., 59, 1245-1250 (View)
FAQs from users: 'Can an IVF cycle be canceled, once started, and not reach the transfer?', 'Are birth control pills always given before fertility treatment?', 'What are the recommendations after IVF?', 'What is the process of IVF using frozen embryos?', 'How long does IVF treatment take from start to finish?' and 'Is the IVF medication always the same?'.
Authors and contributors
More information about Cristina Algarra Goosman














Hello, I got a hysterectomy a couple of years ago, after my last pregnancy. I maintained my ovaries and I was wondering if I could use my eggs and my husband´s sperm and use my friend’s uterus. I think it´s the only way I can have a baby since I can´t carry it myself.
Hello Noi,
Using a third party is known as Surrogacy. There are many clinics that offer this procedure but you should check with your state’s laws to see if it is legal. The procedure would be simple, once the egg and sperm were obtained the lab technicians would fertilize the egg in the lab and create the embryo. Once the embryo was developed and ready it would be transferred into your friend’s uterus.
You can extract a number of eggs and create several embryos that could remain cryopreserved in case you needed them in the future.
I recommend you read the following article: What is surrogacy and how does it work?
I hope I could help you,
All the best
Hello, I am a couple of days before my first transfer, I can´t help but wonder if this cycle is going to work, does anyone know what probability it is for me to get pregnant for the first time? Thanks, this is nerve-racking
Hello Alyssa,
The probability of getting pregnant with IVF depends on several factors, like the technique of fertilization, the sperm quality, the number of transferred embryos, the cause of infertility…
Another important factor would be the woman´s age, if the woman is under 35 there is a probability of pregnancy of 34% per cycle, this percentage decreases to 25.2% when the age of the mother is between 35 – 39.
I recommend you try and focus on this cycle and hope for the best and deal with other solutions when there is a definite problem and you know for sure that this cycle hasn´t worked.
I hope I could help,
Best of luck