Embryo culture is one of the most important phases of in vitro fertilization (IVF) treatments.
The embryos are cultured in the IVF (In Vitro Fertilization) laboratory and the laboratory conditions directly influence the quality of the eggs and embryos.
The time the embryos remain in culture may vary, but 5 days is usual. From this moment on, embryo transfer and/or vitrification of the embryos is performed.
Provided below is an index with the 7 points we are going to expand on in this article.
- 1.
- 2.
- 3.
- 3.1.
- 3.2.
- 3.3.
- 4.
- 4.1.
- 4.2.
- 4.3.
- 4.4.
- 4.5.
- 4.6.
- 4.7.
- 5.
- 6.
- 7.
When is embryo culture performed?
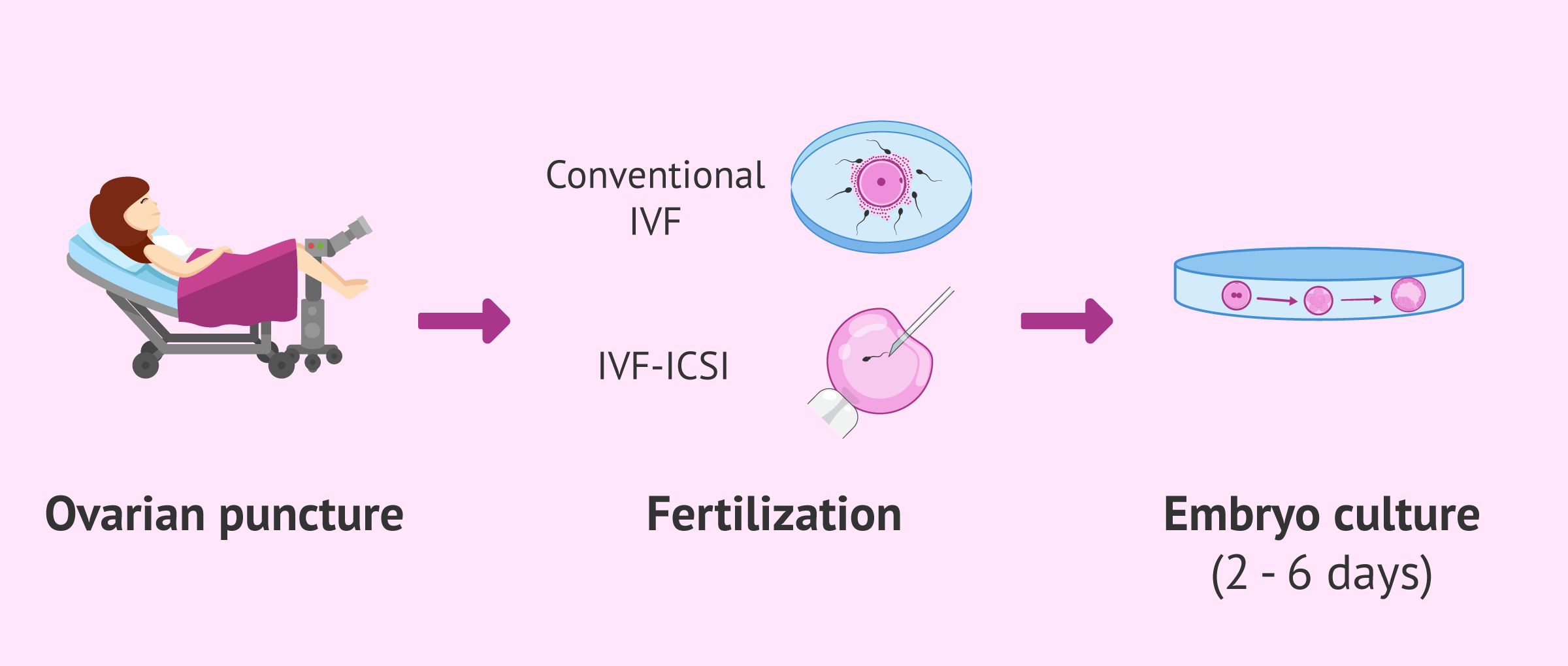
Culturing in the IVF laboratory begins after obtaining the eggs by follicular puncture. Initially, the eggs will be cultured without removing the surrounding granulosa cell layer (decumulation or denudation).
The day of the puncture is known as day 0 of embryonic development, since this is when fertilization (union of the egg and sperm) occurs.
Depending on the IVF technique applied to fertilize the eggs, the next step will be:
- Conventional IVF
- the undecumulated eggs are joined with the spermatozoa.
- ICSI
- the eggs are decumulated and intracytoplasmic microinjection of the sperm is performed.
The culture of embryos obtained after fertilization will be extended until the day the embryos:
- Be transferred to the maternal uterus, which is usually at day 3 or blastocyst stage (day 5-6).
- Be vitrified.
- Are discarded because they do not continue their development or because they have a genetic anomaly after preimplantation genetic diagnosis (PGD).
It should be noted that those surplus embryos that are vitrified can also have different destinations: their own use in the future, donate to research or give to other couples for reproductive purposes. For more information, you can visit this article: What is the destination of IVF leftover embryos?
Stages of embryonic development
Next, we will briefly see which stages embryologists evaluate in order to select the embryo that is most likely to implant and, therefore, result in pregnancy:
- Day 1
- is the day after the follicular puncture and when 16-18 hours after fertilization, it is assessed to see it is has occurred correctly. At this stage, the embryos are called zygotes. Their metabolic needs are very similar to those of oocytes.
- Day 2
- the embryos have already undergone their first divisions and have 2-4 cells, also known as blastomeres.
- Day 3
- at this time, the embryos have about 6-8 blastomeres. The embryo has already begun to express its own genes, so its energy needs are gradually changing.
- Day 4
- the embryo is in the morula stage and compacts.
- Days 5 and 6
- the embryo reaches the blastocyst stage. Embryos that reach this stage with good morphological characteristics have a high probability of implanting.
There are several reasons why embryos may arrest at any point in their embryonic development. Most commonly, embryonic development is blocked due to a genetic abnormality in the embryo.
How should the embryos be grown?
There are variations in embryo culture characteristics between different clinics or even between patients. However, they always agree that embryo culture conditions must be perfectly regulated, since any alteration may affect embryo development and compromise the chances of success of the fertility treatment.
Types of embryo cultures
Depending on the duration of the cultivation, a distinction is made between:
- Short culture: up to day 2 or 3 of embryonic development.
- Long culture: up to the blastocyst stage. The same type of medium can be used throughout the development (single medium) or several different ones (sequential media).
Whether one type of culture or another is performed depends on several factors, such as the number of eggs obtained, the quality of the embryos on day 3 or the need for preimplantation genetic diagnosis (PGD).
In some cases, co-culture is also performed, which consists of culturing the embryos with endometrial cells to improve the conditions of the medium and, thus, the development. However, it is an uncommon technique in the clinic and is used more in the field of research.
Required conditions
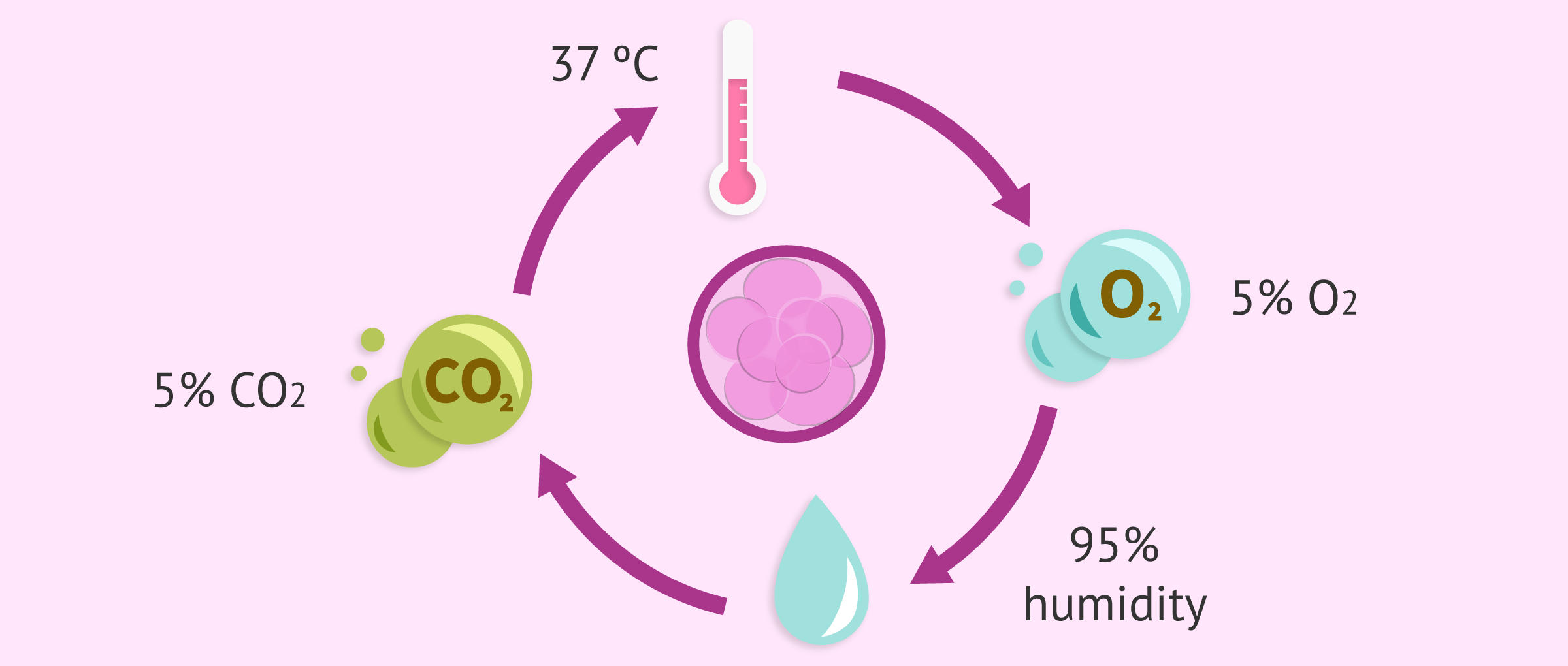
The eggs and embryos should be in as stable an environment as possible. For this purpose, they are kept inside incubators for most of the time, since this way the culture conditions are not altered. Aspects such as the following are controlled:
- Temperature
- Carbon dioxide and oxygen concentration
- Humidity
In addition, it is also necessary for assisted reproduction laboratories to have very controlled conditions. Some of the factors that are regulated are:
- Air purity (with very few particles in suspension)
- Light
- Temperature
- Gases present and in what percentage
Media of embryo culture
The embryos develop in plates with culture media that provide them with the nutrients necessary for them to evolve correctly. As we have already mentioned, their energy needs vary at different stages. Depending on their composition, we distinguish:
- Sequential media
- contain the specific nutrients needed by embryos at certain stages of their development. There is usually one medium for the first two days of embryonic development and another for use after the third day.
- Unique means
- contain all the nutrients needed by the embryo from day one of development to the blastocyst stage. The embryo will consume what it needs at each moment.
FAQs from users
In which patients is long cultivation recommended?
If it were possible, the ideal would be to always perform the blastocyst culture. Over 5- days of culture, we will assess all the embryonic events that must happen (cleavage, compaction, blastulation etc), these allow a better embryo selection, which translates into a higher rate of implantation and pregnancy. If we also apply time-lapse technology, we will obtain more information for an even better embryo selection.
How do I know the chances of my embryos becoming blastocysts?
From the clinical point of view, young women without pathology are more likely to have embryos that reach blastocyst and from the laboratory point of view, those embryos of good quality that correctly comply with cell division times and maintain a perfect morphology in their early development, are also more likely to reach blastocyst.
What does embryonic fragmentation mean?
The laboratory manager and embryologist at Ovoclinic Madrid tells us what embryo fragmentation is. As Aurea tells us:
Embryonic fragmentation is an event that we sometimes see during embryo development. When embryos begin to develop, the ideal is that a mother cell generates two daughter cells, that the distribution of all the material that is in that mother cell passes equally to each of them. Sometimes it happens that these divisions are not completely clean. Two cells are not generated from one, but these two cells are generated and there is part of the cytoplasm that can be detached in the form of fragments. Those fragments are evaluated. We can quantify the percentage of fragments within the total volume of the embryo and this helps us to characterize the quality of each embryo. We observe this especially during the first days of development when the embryo divides into cells, which usually occurs from the day of fertilization, when the signs of fertilization are erased, until more or less the third or fourth day when the compacting and union of these cells begins for the formation of the morula, which is the next stage of development.
Which is better, the short cultur or the long one?
It depends on each case, since each type of culture offers a series of advantages and disadvantages. On the one hand, it is easier to carry out the short culture and, if there are not many embryos available, it is more likely that some will reach the day of the transfer.
On the other hand, by means of the long culture we can better select which is the embryo with more probabilities of implanting, since only those that are of good quality reach this stage.
Therefore, each patient will be more interested in one culture or another depending on the characteristics of their case.
Do all laboratories have the same conditions?
No, because the parameters that are best for one clinic may not be the best for another. For example, some laboratories obtain better results using low oxygen concentrations in incubators, while others see no significant difference.
Are the eggs cultivated in the same way as the embryos?
There are some differences in the composition of the culture media used in some and in others, but in general the conditions are very similar.
Despite the fact that both are very delicate, the eggs are extremely sensitive to changes in temperature, so sudden changes must be avoided when handling them from the moment of follicular puncture.
Is it successful to transfer embryos at day 2 of development?
Dr. Marina González of the Ginemed centers answers us. As the doctor tells us:
Although on day 2 of development we can achieve pregnancy by transferring these embryos, it is true that the embryos as they evolve will have a greater probability of success, the optimum being to transfer embryos at the blastocyst stage. Transferring more evolved embryos has several advantages. On the one hand, it is the most physiological, since in a natural pregnancy the embryo reaches the uterus when it is in the blastocyst stage. In addition, the fact of waiting more days until the transfer will allow us to make a natural selection of the embryos that will be lost throughout the cycle. All this means that the probabilities of success by transfer increase when the embryo's evolution is greater.
Recommended readings
The culture allows us to evaluate the evolution of the embryos, which is a key aspect in achieving pregnancy through IVF treatment. For example, did you know that the evaluation of zygotes (day 1 of development) is essential to rule out some embryos with abnormal chromosome load? You can find more information on this topic at the following link: Classification of embryos according to their quality.
In recent years, there has been a very important improvement in the field of embryo assessment thanks to the application of time-lapse technology in culture. It allows us to visualize embryo development continuously and without altering culture conditions, providing much new information. If you want to read more about this technique, we recommend you read this article: What is time-lapse?
Despite this progress, not all embryos are able to reach the blastocyst stage. Therefore, deciding whether to perform the transfer at day 3 or at the blastocyst stage remains a controversial issue. You can learn more about the advantages and disadvantages of each of these options in the following link: Day 3 or day 5 embryo transfer?
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
C Herbemont, J Labrosse, B Bennani-Smires, I Cedrin-Durnerin, M Peigne, N Sermondade, S Sarandi, A Vivot, E Vicaut, Z Talib, M Grynberg, C Sifer. Impact of oxygen tension according to embryo stage of development: a prospective randomized study. Sci Rep. 2021 Nov 16;11(1):22313 (see)
Lena Bick, Anja Schulz Nielsen, Ulla Breth Knudsen. Embryo Culture Media Influence on Live Birth Rate and Birthweight after IVF/ICSI: A Systematic Review Comparing Vitrolife G5 Media to Other Common Culture Media. JBRA Assist Reprod. 2021 Jul 21;25(3):480-492. doi: 10.5935/1518-0557.20200099 (see)
Linette van Duijn, Jeffrey Hoek, Melek Rousian, Esther B Baart, Sten P Willemsen, Joop S E Laven, Régine P M Steegers-Theunissen, Sam Schoenmakers. Prenatal growth trajectories and birth outcomes after frozen-thawed extended culture embryo transfer and fresh embryo transfer: the Rotterdam Periconception Cohort. Reprod Biomed Online. 2021 Aug;43(2):279-287. doi: 10.1016/j.rbmo.2021.04.013 (see)
Luis H Sordia-Hernandez, Felipe A Morales Martinez, Eduardo Gutierrez Orozco, Andrea Flores-Rodriguez, Paloma C Leyva-Camacho, Neri Alejandro Alvarez-Villalobos, Jorge Alberto Zuñiga-Hernandez. The Effect of Post warming Culture Period Between Thawing and Transfer of Cryopreserved Embryos on Reproductive Outcomes After In Vitro Fertilization (IVF): A Systematic Review and Meta-analysis (see)
Shanshan Wang , Lei Chen , Yingchun Zhu , Weihua Jiang. Characterization of microRNAs in spent culture medium associated with human embryo quality and development. Ann Transl Med. 2021 Nov;9(22):1648. doi: 10.21037/atm-21-5029 (see)
FAQs from users: 'In which patients is long cultivation recommended?', 'How do I know the chances of my embryos becoming blastocysts?', 'What does embryonic fragmentation mean?', 'Which is better, the short cultur or the long one?', 'Do all laboratories have the same conditions?', 'Are the eggs cultivated in the same way as the embryos?' and 'Is it successful to transfer embryos at day 2 of development?'.
Authors and contributors


More information about Cristina Algarra Goosman









Hello, I had an embryo transfer on day 3, when it was implanted it stopped growing and the IVF failed, if it had been implanted on day 5 could it have survived?
Hello Xanon,
I am sorry to hear that your cycle failed. An embryo on day 3 of development has between 6 and 8 cells and there can be a selection based on the development they have shown.
When there is a transfer there are changes in the conditions and sadly some embryos can´t survive those changes. This could be the reason the embryo didn´t survive or there could have been a genetic or development malformation the technicians hadn´t caught before implantation.
I recommend you speak with your clinic technicians so they can explain and assess you on what steps to follow.
I hope everything turns out good,
Good luck!
Hello, how long do embryos have to mature before they can be transferred to the uterus?
Hi Kassie,
Generally, embryos are matured in the lab until day 3 or 5, there are both advantages and disadvantages to transferring. Since the embryo descends into the uterus naturally around day 4 after fertilization so the endometrium is receptive and there is a possibility of continuing the pregnancy.
I recommend that you read the following article which explains the main characteristics and situations in which embryo transfer on day 3 or 5 is recommended: When to do an embryo transfer?
I hope I have helped,
Best regards