In recent years, blastocyst culture is becoming increasingly popular in almost every In Vitro Fertilization (IVF) procedure due to better implantation rates with blastocyst embryos (day 5-6 of development) than with embryo transfer at earlier stages.
One of the multiple advantages it offers is that is allows for a better selection of embryos. To this end, blastocysts are cultured based on their morphology and grade of expansion, that is, their stage of development: early, cavitating, expanded, hatching, etc.
Provided below is an index with the 10 points we are going to expand on in this article.
- 1.
- 2.
- 2.1.
- 2.2.
- 3.
- 3.1.
- 3.2.
- 3.3.
- 4.
- 5.
- 6.
- 7.
- 7.1.
- 7.2.
- 7.3.
- 7.4.
- 7.5.
- 7.6.
- 7.7.
- 7.8.
- 7.9.
- 8.
- 9.
- 10.
What is blastocyst culture?
Long embryo culture consists of keeping the embryos in the laboratory until day 5 or 6 of their development when they reach the blastocyst stage. Throughout these days, the embryos are inappropriate conditions that favor their development.
Blastocysts are made of two clearly identifiable parts:
- Trophoblast
- Composed of the cells of the blastocyst that are in direct contact with the uterine lining (endometrium). This structure will turn into the placenta eventually. The outer layer is protected by the zona pellucida (ZP).
- Inner cell mass
- Located within the trophoblast. It develops into the fetus.
When an embryo attaches naturally to the uterine lining, it is at the blastocyst stage. If embryo development occurs artificially at an IVF laboratory, it should be cultured in optimal conditions in order for it to reach the blastocyst stage and still be a high-quality embryo, with implantation potential.
Types of embryo culture
Extended embryo culture can be done in two different culture media, as one shall see in the sections below:
Embryo culture using sequential media
In order to allow embryos to make it to the blastocyst stage, they are cultured in two media of different chemical compositions to adapt to the nutritional requirements of embryos at each phase of their development.
Embryos are cultured in the first medium from the zygote (day 1) stage until day 3. The second media will be used from day 3 until the blastocyst stage (days 5-6 of development).
Embryo culture using global media
In this case, embryos are cultured in a single type of medium that contains all the necessary nutrients embryos need from day 1 of development until the transfer or vitrification day on day 5-6 when they reach the blastocyst stage.
Assisted procreation, as any other medical treatment, requires that you rely on the professionalism of the doctors and staff of the clinic you choose. Obviously, each clinic is different. Get now your Fertility Report, which will select several clinics for you out of the pool of clinics that meet our strict quality criteria. Moreover, it will offer you a comparison between the fees and conditions each clinic offers in order for you to make a well informed choice.
Blastocyst grading
Currently, one of the most widely used methods to predict the implantation potential of blastocysts is morphological assessment. Thanks to it, we can classify embryos according to their quality.
For embryo classification, the degree of expansion, the inner cell mass (ICM), and the trophectoderm are evaluated. In addition, it is necessary that the blastocele has developed so that the structures can be easily observed.
According to these three parameters, the traditional method used to classify embryos uses a figure (1-5) and two letters (A-D), based on the degree of expansion, the quality of the ICM, and the trophoblast, respectively. For example, following the criteria that we will explain below, and expanded blastocyst of good quality would be classified as 3AA.
Degree of expansion
The numerical score of blastocyst embryos is established using the following numerical score system:
- Grade 1 or early blastocyst
- The blastocoel starts to be visible.
- Grade 2 or cavitating blastocyst
- Both the trophoblast and the ICM are distinguishable.
- Grade 3 or expanded blastocyst
- The blastocyst has increased in size. The layer that covers it, the ZP, is thinner now.
- Grade 4 or hatching blastocyst
- The blastocyst is starting to hatch out of the ZP.
- Grade 5 or hatched blastocyst
- The blastocyst is already completely hatched.
Inner cell mass (ICM)
When it comes to evaluating the ICM, the embryologist takes into account its size, degree of compaction, and its appearance:
- A score
- Multiple compacted cells.
- B score
- Multiple non-compacted cells.
- C score
- Only a few cells.
- D score
- Cells with signs of degeneration.
Trophoblast
As regards the trophoblast, which should be formed of a single layer, the parameter examined is its appearance:
- A score
- Homogeneous, cohesive, and with multiple cells.
- B score
- Homogeneous and with a lower number of cells.
- C score
- With a reduced number of cells.
- D score
- Cells with signs of degeneration.
It should be noted that the Association for the Study of Reproductive Biology (ASEBIR) has established a new classification of embryos at day 5 of development and gives priority to the trophectoderm over the inner cell mass. Therefore, only one letter would be used. For example, a blastocyst with an ICM of category A and trophoectoderm of B quality, then the blastocyst would be of B quality.
Indications
Long culture is not performed in all patients, as it depends on several factors. Therefore, it is of vital importance to evaluate each patient individually and to take into account the number of embryos available. For example, long embryo culture can be used in the following situations:
- IVF cycles in which the number of high-quality embryos is high on day 3 of development.
- Cases of repeated implantation failure.
- Patients who undergo Preimplantation Genetic Diagnosis (PGD).
- Patients of advanced maternal age.
- Patients with repeated miscarriages
- Cases in which multiple pregnancy is contraindicated.
- To optimize a cycle of vitrification, since waiting up until the embryo reaches the blastocyst stage to cryopreserve the embryos allows us to store only those with the best quality.
It is therefore of vital importance to assess each patient individually and to take into account the number of embryos available.
Advantages and disadvantages
Extended culture increases the overall success rates of IVF cycles because:
- It increases the implantation rates, as it allows for an improved embryo selection process.
- It diminishes the risk of multiple births, as it allows for Single Embryo Transfers (SETs) without affecting the pregnancy success rates.
- It enhances the synchronization between the embryo and the endometrial lining.
Nonetheless, in spite of the advantages that blastocyst embryo transfers offer, it is not indicated for all kinds of patients due to the cons associated:
- Many embryos arrest before even making it to the blastocyst stage. Thus, you would be putting yourself at risk of having no embryos available on the transfer day.
- Not all IVF laboratories reach good outcomes with extended embryo culture.
- It is necessary to have a significant number of eggs/embryos available to make sure that a certain number of embryos will be available on the transfer day.
Nevertheless, it is essential to analyse all the factors together and to follow the recommendations set out by specialists.
What to expect
José Luis de Pablo, BSc, Ph.D., Senior Clinical Embryologist by the ESHRE, indicates that blastocyst culture is highly advisable when we have at least three embryos of good quality on day 3 of development.
Unfortunately, predicting if they will actually make it to blastocyst is impossible. When we opt for sequential embryo culture, we are doing a much stricter embryo selection process in order to choose only those with the highest implantation potential.
De Pablo also suggests that talking about success rates with blastocyst culture is complicated since it is directly associated with the age of the patient. Depending on the age group, we can talk about pregnancy rates with accuracy.
It is true, however, that embryos that make it to blastocyst have a greater implantation potential, that is to say, they are more likely to lead to a positive pregnancy test.
FAQs from users
Why are embryos lost throughout the culture time?
The embryologist Laura Molina from the Ginemed centers answers us:
Evidently they are embryos that do not have optimal characteristics to develop normally. It is not that they are lost due to the procedure or due to incubation or due to the conditions in the laboratory, but it is the embryo itself that, due to any type of metabolic failure or some type of chromosomal genetic alteration that it may have, automatically those embryos will not progress and will stop in their development. They are blockages that are associated with the quality of the embryo itself, which can come from problems that come from the sperm as well as from the ovules. Actually, it is also a form of selection. This long development also allows us to assess the quality of the embryos because if they do not evolve, they would not become pregnant either.
What does the term early blastocyst refer to?
The blastocyst stage is characterized because the cells are arranged in such a way that in one area of the embryo a cellular group accumulates, which is called the inner cell mass and will give rise to the embryo and the fetus that we will later see in the ultrasound scans. While the rest of the embryo is surrounded by a row of cells that will give rise to the membranes and the placenta, which we call the trophoectoderm. And in the central area there is an area without cells with a liquid inside, which is called the blastocele and which will give rise to the amniotic fluid.
The difference between an early blastocyst and an expanded blastocyst is that, in the first case, the separation of these three parts begins to be intuited, initially appearing the blastocele which differentiates two cell groups, one that will give rise to the inner cell mass and the other to the trophoectoderm. At this stage the blastocyst is not clearly expanded and therefore the zones are not clearly differentiated. This embryonic stage usually begins to be seen at the end of the fourth day or at the beginning of the fifth day.
Read more
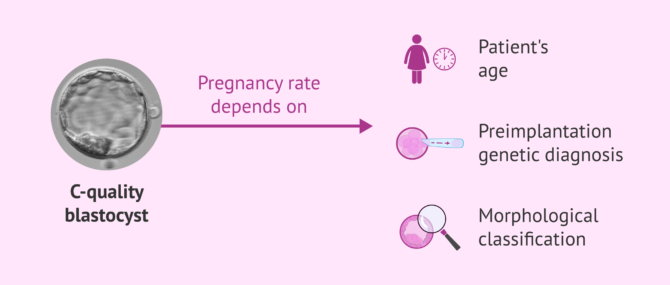
Do I have a high probability of pregnancy with a C-grade blastocyst?
We do not know the patient's age or whether the embryo has undergone perimplantation genetic diagnosis (PGD), but we will now explain the probability of pregnancy according to different variables:
- The age of the patient when the blastocysts were generated: normally ages below 35 years give us the highest pregnancy rates. This allows egg donation (age of donors under 35 years according to the law) to have accumulated pregnancy rates close to 90%.
- Perimplantation genetic testing of aneuploidy: allows a more efficient selection of embryos than classification by morphology. This test is able to tell us which embryos will not be implanted, therefore it can make us have the same pregnancy rate in a 40 year old woman as in a 35 year old one, since when we transfer an embryo it will be a healthy embryo.
- Morphological classification: embryos are classified by their morphology (by their shape), how they have divided, according to fragmentation (cell fragments that are produced in cell division) and the internal cell mass (future embryo and the trophoectoderm that will give rise to the placenta). Normally, embryos are classified with two letters, that determines the potential for implantation. It should be noted that each laboratory has its results according to the type of embryo.
 /div>
/div>Why do some embryos not reach the blastocyst stage?
Embryonic blockage is the term used to refer to the fact that the embryos have not been able to form a blastocyst. They are normally embryos that usually stop developing on day +3/4 at the cell/morula stage.
Approximately between 50-60% of the embryos have the capacity to reach the blastocyst, the embryos that do not achieve this suffer the so-called embryonic arrest. Poor oocyte and seminal quality can be a reason for blocking the embryos. For example, it has been seen that sperm DNA fragmentation has a negative effect on embryonic development, producing a slower evolution of the embryos and being negatively related to embryonic arrest.
Another factor to take into account is the age of the oocyte. We know that the presence of chromosomal abnormalities in the oocyte increases with the age of the woman, influencing the embryonic genetic load and therefore its development. In addition, there are studies that show that one of the main causes of embryonic arrest is the presence of chromosomal abnormalities in the cells of the embryo. Specifically, it has been seen that almost 70% of the embryos that do not form the blastocyst have chromosomal abnormalities.
Advances and new technologies have allowed embryos to be cultured up to day +6 of embryonic development. The long culture allows us to select the embryos that have the capacity to form the blastocyst on day +5/+6 and, therefore, allows us a better embryonic selection. It will not be until day +3 of the culture when the embryo activates the embryonic genome, this activation is essential for the embryos to reach the blastocyst stage.
In which patients is long cultivation recommended?
If it were possible, the ideal would be to always perform the blastocyst culture. Over 5- days of culture, we will assess all the embryonic events that must happen (cleavage, compaction, blastulation etc), these allow a better embryo selection, which translates into a higher rate of implantation and pregnancy. If we also apply time-lapse technology, we will obtain more information for an even better embryo selection.
What are the success rates with blastocyst embryo culture?
By blastocyst culture we refer to keeping the embryos in the incubator until day 5-6 of development, that is, until they reach blastocyst stage. By doing this, we perform a much more thorough embryo selection process. The fact they they are capable of making it to blastocyst means that they have a greater implantation potential, as it was able to stay longer in the lab. Pregnancy success rates depend on age, though.
What is the difference between blastocyst and blastocele?
A blastocyst is an embryo that has begun the process of cavitation, on days 5-6 of development. Thanks to this cavitation, the blastocele, the central fluid-filled cavity, which is characteristic of blastocysts, is formed.
Can poor quality embryos implant as well?
Absolutely yes. The chances for pregnancy with poor quality blastocysts are lot, but they exist. Pregnancy is possible as well.
What percentage of embryos that reach day 3 reach the blastocyst stage?
As we know, embryonic development lasts between 5-6 days. During these days the embryo evolves from the fertilised oocyte, 1 cell, to approximately 150-200 cells. On day 5-6 of development it reaches the blastocyst stage where we can observe two well differentiated structures, the inner cell mass, the cell group within the embryonic cavity that will give rise to the foetus and the trophectoderm, which is the cell layer that surrounds the inner cell mass and which will join the endometrium to form the placenta.
Approximately 40-60% of developing embryos on day 3, where the number of cells is between 6 and 12, reach the blastocyst stage. Although it is true that most of the embryos generated develop until day 3 of culture, where the oocyte plays a fundamental role, from day 3 onwards the embryonic genome is activated and it is the embryo itself that directs its development.
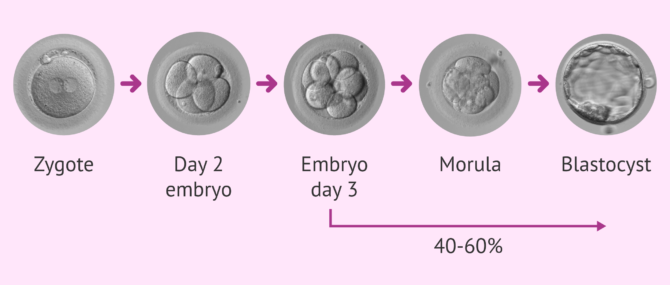
Many of the embryos do not continue their development from day 3 to day 5. Therefore, development up to day 5 of development is in itself a process of embryo selection. Many times we have precious embryos at day 3 that we would transfer and when we leave them in culture we see that they are arrested in their development and would never have achieved pregnancy if we had transferred them.
Embryos that reach the blastocyst stage have a higher probability of implantation. It is also important to bear in mind that nowadays both the culture media and incubation systems and a good blastocyst culture programme in the laboratory allow us to carry out this type of in vitro selection.
Recommended readings
If you are interested in learning more about embryo culture, a process that takes place at the IVF lab, we recommend that you have a look at this: Embryo Culture Media for Human IVF.
Also, you can find more details about the difference between day 3 and day 5 embryo transfer, visit the following post: Day 5 vs. Day 3 Embryo Transfer – What Are the Pros & Cons?
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
Balaban B, Urman B. Comparison of two sequential media for culturing cleavage-stage embryos and blastocysts: embryo characteristics and clinical outcome. Reprod Biomed Online 2005;10:485–91 (View)
Biggers JD, Summers MC. Choosing a culture medium: making informed choices. Fertil Steril 2008;90:473–83 (View)
Ciray HN, Aksoy T, Goktas C, Ozturk B, Bahceci M. Time-lapse evaluation of human embryo development in single versus sequential culture media— a sibling oocyte study. J Assist Reprod Genet 2012;29:891–900 (View)
Lane M, Gardner DK. Embryo culture medium: which is the best? Best Pract Res Clin Obstet Gynaecol 2007;21:83–100 (View)
Mantikou E, Youssef MA, van Wely M, van der Veen F, Al-Inany HG, Repping S, et al. Embryo culture media and IVF/ICSI success rates: a systematic review. Hum Reprod Update 2013;19:210–20 (View)
Mauri AL, Petersen CG, Baruffi RL, Franco JG Jr. A prospective, randomized comparison of two commercial media for ICSI and embryo culture. J Assist Reprod Genet 2001;18:378–81 (View)
Summers MC, Bird S, Mirzai FM, Thornhill A, Biggers JD. Human preimplantation embryo development in vitro: a morphological assessment of sibling zygotes cultured in a single medium or in sequential media. Hum Fertil (Camb) 2013;16:278–85 (View)
FAQs from users: 'Why are embryos lost throughout the culture time?', 'What does the term early blastocyst refer to?', 'Do I have a high probability of pregnancy with a C-grade blastocyst?', 'Why do some embryos not reach the blastocyst stage?', 'In which patients is long cultivation recommended?', 'What are the success rates with blastocyst embryo culture?', 'Could a blastocyst transfer with PGD help prevent implantation failure?', 'When does the embryo implant after blastocyst transfer?', 'What is the difference between blastocyst and blastocele?', 'Can poor quality embryos implant as well?' and 'What percentage of embryos that reach day 3 reach the blastocyst stage?'.
Authors and contributors


More information about Cristina Algarra Goosman















