Virtually all in vitro fertilization (IVF) processes include an ovarian stimulation treatment. The objective of this is to favor the development of more than one ovarian follicle since only one would develop naturally, in order to obtain a greater number of mature eggs and increase the probability of pregnancy.
Faced with this treatment, many women ask themselves the following question: How many eggs must be obtained in order to achieve pregnancy in an IVF process? Although there is no single answer, there are certain important aspects related to this question.
Provided below is an index with the 7 points we are going to expand on in this article.
- 1.
- 1.1.
- 2.
- 2.1.
- 2.2.
- 3.
- 4.
- 4.1.
- 4.2.
- 4.3.
- 4.4.
- 5.
- 6.
- 7.
Ovarian response during IVF cycles
The ovarian response to the stimulation carried out in the IVF-ICSI cycles will vary from one woman to another depending on the indicated medication regimen, the woman's fertility situation, etc. Thus, we can distinguish three types of women based on their response to ovarian stimulation:
- Low responders: these are women from whom it has only been possible to obtain a maximum of 3 ovules in the follicular puncture after stimulation. In this group, we find women with a low ovarian reserve due to age, but also those women with certain pathologies that prevent obtaining a greater number of eggs.
- Normoresponders: in these women, after ovarian stimulation it is possible to obtain between 4-15 ovules per cycle. However, there are those who differentiate a subgroup called suboptimal response for patients from whom between 4-9 oocytes are obtained.
- Hyper-responders: this group corresponds to women from whom more than 15 oocytes per cycle can be obtained. They are usually young women without fertility problems, such as donors.
- Low responders
- When the number of eggs retrieved is 3 or less. Some clinics set this limit on 5 eggs. It typically corresponds to women with poor ovarian reserve due to age, as well as those with certain conditions that prevent the development of a higher amount of eggs.
- Normal responders
- Fortunately, most women can be included in this second group. It means that a good number of eggs is retrieved after undergoing stimulation. Broadly speaking, the average number of eggs is 6-7 or even 9-10 per cycle.
- High responders
- We include here cases where 20 or more eggs per cycle are obtained. The profile of these patients is typically associated with young girls, without fertility problems. A good example is egg donors. Even though it occurs rarely, there have been cases in which over 50 eggs have been retrieved.
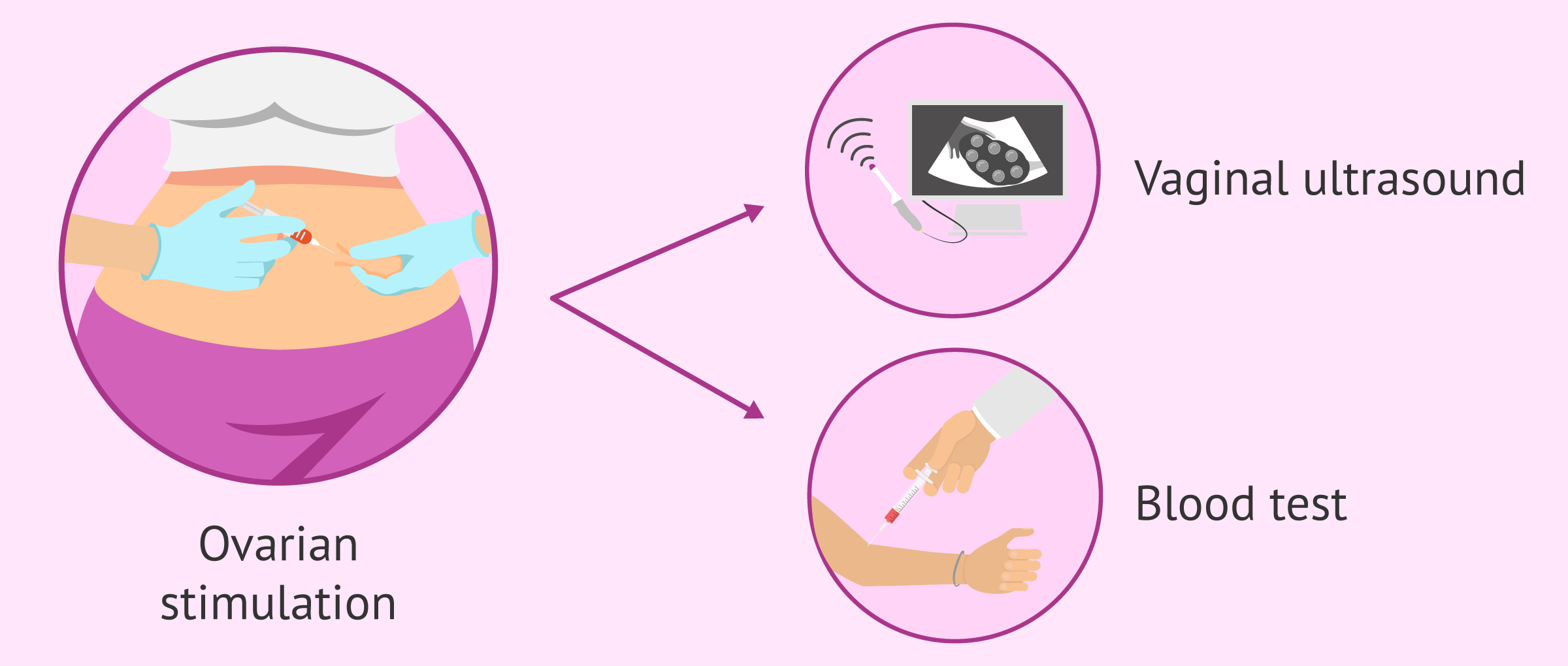
It is very important that, during the period of ovarian stimulation, the woman goes to the specialist's office for an ultrasound and analytical controls. In this way, the gynecologist will be able to assess the response of the ovary to the hormonal medication administered and adjust the dose if necessary.
Clinical significance
That a woman is in one group or another of ovarian response is not indicative of pathology. As an example, it is normal for a 45-year-old woman to be a low-responder. In fact, few eggs are obtained in the puncture because her ovarian reserve is low since she is close to menopause.
For its part, a healthy 20-year-old woman is expected to respond excessively to stimulation, so it will be essential to properly control the dose of medication. The most unusual thing, in this case, would be that this young woman manifested a low response.
If you need to undergo IVF to become a mother, we recommend that you generate your Fertility Report now. In 3 simple steps, it will show you a list of clinics that fit your preferences and meet our strict quality criteria. Moreover, you will receive a report via email with useful tips to visit a fertility clinic for the first time.
Estimation of the number of oocytes
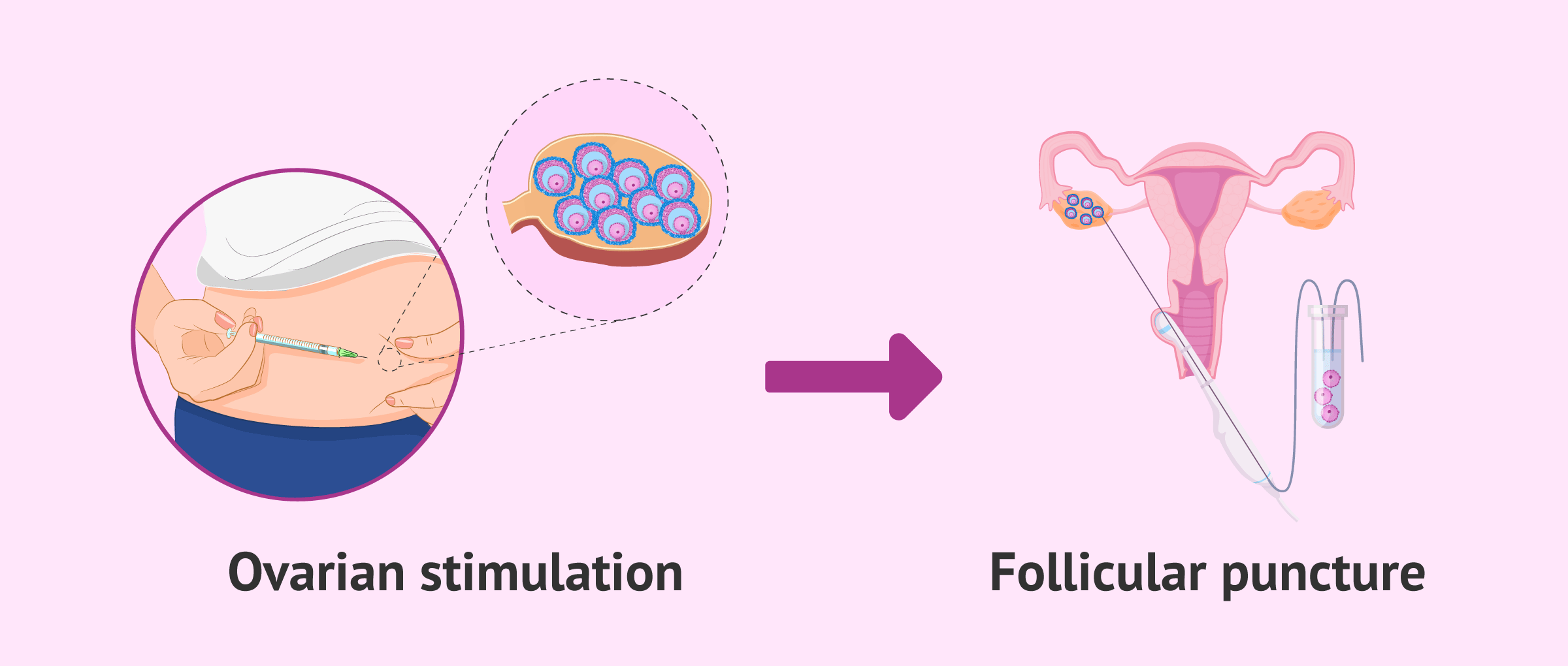
Follicular puncture is the surgical intervention in which the ovules are obtained after ovarian stimulation. The objective of this procedure is to extract the ovules when they are in a stage of maturation known as metaphase II. This is the stage considered mature since it is in which the fertilization of the oocyte by the sperm can occur.
To schedule the follicular puncture at the right time and to be able to predict, approximately, the number of ovules that will be obtained, these two aspects are analyzed: the follicular size and the concentration of estradiol.
Each follicle develops an oocyte inside, but it is possible that, at the time of puncture, no oocyte is obtained from some follicles or that some oocytes are immature and, therefore, not suitable for fertilization.
Therefore, the number of mature oocytes recovered after ovarian puncture may be lower than the number previously estimated.
Follicle size
As the maturation stage of the ovarian follicles progresses, they increase in size. For this reason, the gynecologist controls the size of the follicles using transvaginal ultrasound. When a follicle measures around 16-18 mm, it is established that it has developed enough so that there is a mature oocyte inside it. In this way, the puncture will be scheduled 34-36 hours after finding follicles of this size.
Therefore, measuring the size of the follicles will be a way to estimate the number of mature eggs that will be extracted during the follicular puncture.
Blood estradiol concentration
Each mature ovarian follicle can correspond approximately to 200-300 pg/ml of estradiol in the blood. Therefore, taking this information into account, we can estimate the number of mature follicles based on the concentration of estradiol determined by a blood test.
As an example, an estradiol concentration of 3000 pg/ml would make us think that the gynecologist could puncture around 15 follicles, that is, extract around 15 ovules.
Quantity or quality of the ovules?
The purpose of an in vitro fertilization process is to achieve a healthy baby. For this, it is necessary to obtain viable embryos, capable of implanting in the maternal uterus and giving rise to an evolutionary gestation. This is why we can say that quantity is not as important as oocyte quality (and, of course, also of the sperm).
It is true that the greater the number of ovules, the greater the probability of creating viable embryos and, therefore, of achieving reproductive success. However, if the eggs obtained are of poor quality, it will be more difficult to achieve conception even if many have been extracted in the puncture.
On the other hand, if we have fewer ovules but they are of high quality, it is likely that at least one embryo capable of implanting in the uterus and giving rise to pregnancy will be obtained.
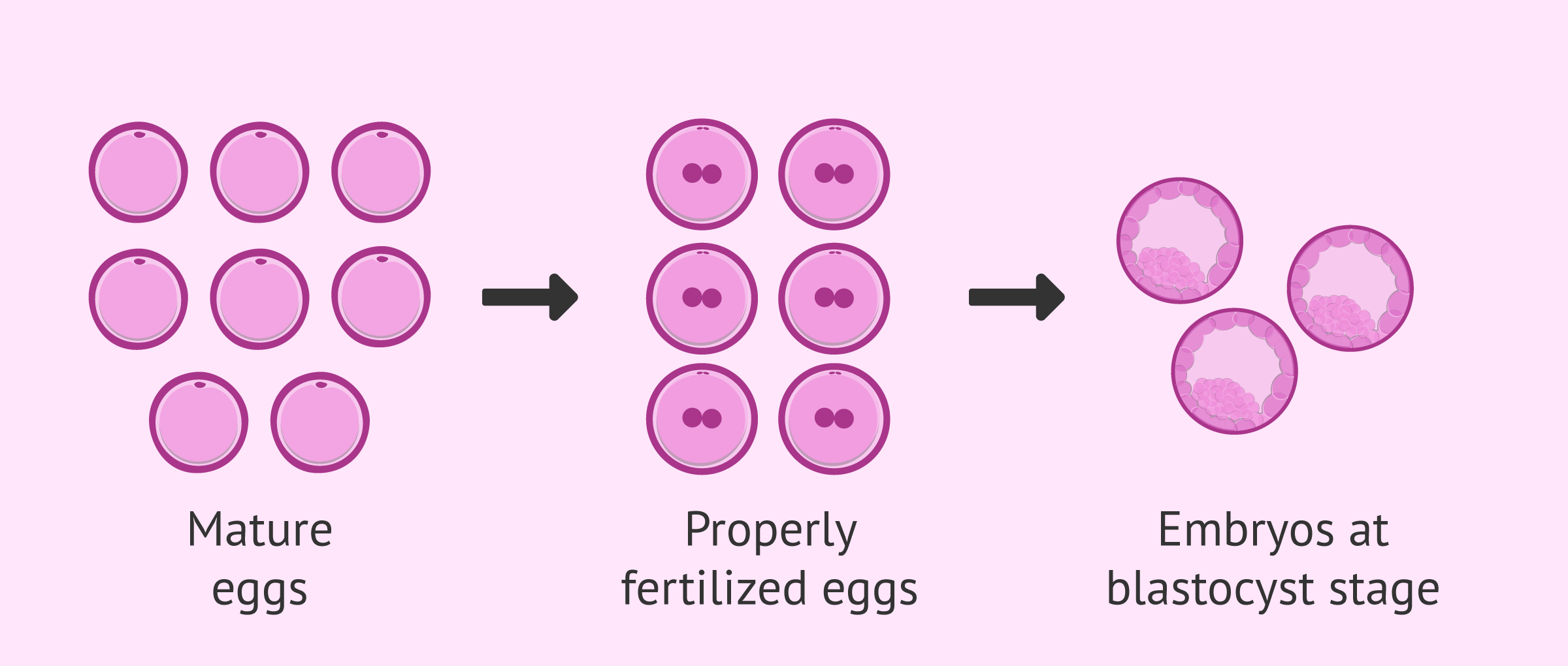
On the other hand, we must take into account that the number of ovules does not always correspond to the number of embryos. Of the mature ovules obtained, not all will be able to fertilize correctly and, of those that are fertilized, some will be blocked during embryonic development.
For this reason, it is important to obtain a good number of quality eggs, in order to have a greater number of viable embryos. In this way, these embryos can be vitrified and transferred in later cycles, either because the first attempt was not successful or because they want to have more offspring.
In any case, and by way of conclusion, we must emphasize that it is not only a matter of quantity but also of the quality of the ovules.
FAQs from users
What is the ideal number of eggs for an IVF cycle?
While the success with IVF literally only requires one normal embryo, patient outcomes improve with a reasonable number of eggs retrieved, typically 10-15 mature eggs. Actually, studies have shown that egg quality may be reduced if retrieval results in an excessively high number of eggs. Of the eggs retrieved, approximately 60-80% are mature and of these, about 70-80% will fertilize. Once an embryo divides, it has a 50-60% chance of developing into a day 5 blastocyst which is most optimal for implantation or freezing.
How many follicles are needed for IVF?
After undergoing ovarian stimulation, at least 3 mature follicles should be ready to be punctured. Follicles are considered mature when they are 16-20 mm in average diameter.
Is the quality or quantity of eggs more important in an IVF cycle?
Both aspects are important. However, it is essential that the egg is of good quality, because if the quality is low, it will not matter how many eggs we obtain, since it is likely that none of them will allow pregnancy after fertilization.
My gynecologist tells me that they anticipate getting 4 mature eggs in the retrieval, is that ok?
Under normal conditions, 4 eggs is a low number. However, depending on your situation and age, it is possible that it is a good prognostic number. In any case, the important thing is that these 4 eggs are of good quality. If at least one of them is of very good quality and allows obtaining an embryo capable of implantation, pregnancy will be achieved. In this case, 4 eggs will be sufficient to achieve the objective: gestation.
Recommended readings
If you liked this story, you may want to go through this: Collecting a Large Number of Eggs & Pregnancy Chances.
Also, if you are a poor responder, you may enjoy reading the following post: Poor Responders in IVF Cycles – Management & Best Protocols .
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
Dickey RP, Taylor SN, Lu PY, Sartor BM, Rye PH, Pyrzak R (2002). Effect of diagnosis, age, sperm quality, and number of preovulatory follicles on the outcome of multiple cycles of clomiphene citrate-intrauterine insemination. Fertil Steril;78:1088 – 1095.
Ghesquiere SL, Castelain EG, Spiessens C, Meuleman CL, D’Hooghe TM. Relationship between follicle number and (multiple) live birth rate after controlled ovarian hyperstimulation and intrauterine insemination. Am J Obstet Gynecol 2007;197:589.e1– 5
Hamoda H, Sunkara S, Khalaf Y, Braude P, El-Toukhy T. Outcome of fresh IVF/ICSI cycles in relation to the number of oocytes collected: a review of 4,701 treatment cycles. Hum Reprod 2010;25:147.
Kably Ambe A, Estevez Gonzalez S, Carballo Mondragon E, Dura´n Monterrosas L. Comparative analysis of pregnancy rate/captured oocytes in an in vitro fertilization program. Ginecol Obstet Mex 2008; 76:256 – 260. Spanish.
Kyoung YM,Hoon K, Joong YL, Jung RL, et al. Nomogram to predict the number of oocytes retrieved in controlled ovarian stimulation. Clin Exp Reprod Med 2016;43:112-118.
Letterie G, Marshall L, Angle M. The relationship of clinical response, oocyte number, and success in oocyte donor cycles. J Assist Reprod Genet 2005;22:115 – 117.
López-Rioja MJ, Campos-Cañas JA, Recio-López Y, Quiroz-Garza G, Sánchez-González M, HinojosaRodríguez K, Laresgoiti Servitje E. Número óptimo de ovocitos: modelo de predicción para fertilización in vitro. Ginecol Obstet Mex. 2017 nov;85(11):735-747.
Meniru GI, Craft IL. Utilization of retrieved oocytes as an index of the efficiency of superovulation strategies for in-vitro fertilization treatment. Hum Reprod 1997;12:2129– 2132.
Molina Hita Ma. del M, Lobo Martinez S, Gonzalez Varea, Montejo Gadea JM, Garijo Lopez E, Cuadrado Mangas C. Correlation between the number of oocytes and the pregnancy rate in IVF-ICSI cycles. Revista Iberoamericana de Fertilidad y Reproduccion Humana 2008; 25:153 – 159. Spanish
Polyzos NP, Sunkara SK. Sub-optimal responders following controlled ovarian stimulation: an overlooked group? Hum Reprod. 2015 Sep;30(9):2005-8.
Steward RG, Lan L, Shah AA, Yeh JS, et al. Oocyte number as a predictor for ovarian hyperstimulation syndrome and live birth: an analysis of 256,381 in vitro fertilization cycles. Fertil Steril 2014;101:967-973.
Sunkara SK, Rittenberg V, Raine-Fenning N, Bhattacharya S, et al. Association between the number of eggs and live birth in IVF treatment: an analysis of 400 135 treatment cycles. Hum Reprod 2011;26:1768-1774.
Vaiarelli A, Cimadomo D, Ubaldi N, Rienzi L, Ubaldi FM. What is new in the management of poor ovarian response in IVF? Curr Opin Obstet Gynecol. 2018 Jun;30(3):155-162.
Van der Gaast MH, Eijkemans MJ, van der Net JB, de Boer EJ, et al. Optimum number of oocytes for a successful first IVF treatment cycle. Reprod Biomed Online 2006;13:476-480.
FAQs from users: 'What is the ideal number of eggs for an IVF cycle?', 'How many follicles are needed for IVF?', 'Is the quality or quantity of eggs more important in an IVF cycle?', 'How many do you need for IVF?', 'Do all fertilized eggs result in pregnancy?' and 'My gynecologist tells me that they anticipate getting 4 mature eggs in the retrieval, is that ok?'.
Authors and contributors
More information about Cristina Algarra Goosman

More information about Michelle Lorraine Embleton






Is it possible for a donor to produce 10 A quality embryos? What is considered a low quality outcome for an exclusive fresh egg donor?
Hi Claire
Well, yes it is possible for a donor to produce 10 A quality embryos and it would be an excellent result. To achieve 10 embryos is a very good number and grade A is the best quality embryo.
You can read about the quality of embryos and what this means in this article: Embryo Quality & Grading – Does It Affect IVF Success?
A low quality outcome for an exclusive fresh egg donor would be a lower number of embryos, of which the embryos are of grade C or D, which have a lower chance of implantation, and a small number of embryos.
In any case, the specialist will select the best quality embryos for embryo transfer and usually only one or two embryos are transferred, so a large number is not required. You can read more about this in the following article:Embryo transfer: How many embryos should be transferred in IVF?
I hope this answers your questions.
All the best
I thought I had a problem with my laboratory, they extracted 15 eggs and only 4 embryos were left, I thought that they had been treated badly or with some negligence… I understand that it is considered within the normal range then.
Hi Savannah,
Indeed, not all the eggs obtained manage to survive, once extracted they must mature, survive fertilization and develop properly until the blastocyst stage where they are transferred to the uterus or frozen for future cycles.
I hope I have helped you,
Best regards
Hello, I had a puncture this week for IVF, they had planned to remove 10 eggs but only 6 have come out, is it a failure?
Hi Mindyy,
The estimate made by the gynecologist before the puncture may vary depending on several factors. More than the number of eggs obtained is the quality of the eggs.
Of those 6 eggs, it must be taken into account that they must mature, fertilize and develop into an embryo. It is common that not all the eggs that are extracted survive all the processes through which they have to go through.
The quality of the eggs will have a great influence on their capacity to reach the embryonic stage. I would not consider obtaining 6 follicles as something negative, we will have to wait to see how they develop and adjust according to the results.
I hope I have helped you,
Best regards.