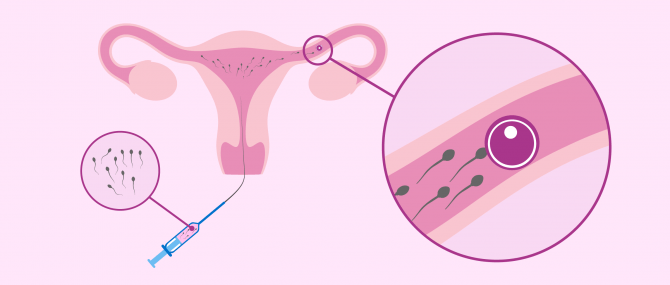
Intrauterine insemination (IUI) or artificial insemination is a fertility treatment that involves inserting a semen sample into the uterus of the woman by controlling her ovulation cycle with hormone medications. The ultimate goal is to increase the chances of pregnancy.
In short, it is a simple process that can be performed at the doctor's office. Anesthesia is not required, as it is enough with the insertion of an insemination cannula, which is not painful at all.
Provided below is an index with the 9 points we are going to expand on in this article.
- 1.
- 1.1.
- 1.2.
- 1.3.
- 1.4.
- 2.
- 3.
- 4.
- 5.
- 6.
- 6.1.
- 6.2.
- 6.3.
- 6.4.
- 6.5.
- 6.6.
- 6.7.
- 7.
- 8.
- 9.
IUI step by step
As one shall see in the video below, the intrauterine insemination process includes the stages of ovarian stimulation, semen collection, lab processing of the semen sample, and finally insemination per se.
Ovarian stimulation
This stage can last up to 10 to 12 days. It involves the administration of gonadotropins in small doses through an injection.
It is also important to control the number of follicles that are expected to be obtained in order to avoid a multiple pregnancy. Follicular maturation can be monitored by means of a transvaginal ultrasound and an estradiol test.
The goal of these medications is to stimulate the ovary in a controlled manner to trigger the maturation of multiple eggs, simulating the natural process. It is important to monitor ovarian development, readjusting the dosage of hormone medications, to prevent that multiple eggs develop.
This would increase the risk of multiple pregnancy, as fertilization occurs inside the woman's organism.
Monitoring the cycle
Follicle maturation can be monitored through a transvaginal ultrasound as well as with an analysis of estradiol levels.
Follicles are structures located in the ovary where eggs develop.
When the OB/GYN observes that the size of one or two follicles reaches 16-18 mm, ovulation is triggered naturally using the hSG shot.
This hormone, administered in a single shot on day 12-14 of the cycle, allows follicles to release the eggs they contain. Thus, when an egg leaves the ovary, starts a journey toward the Fallopian tubes, where they will be waiting for the arrival of spermatozoa.
Insemination or insertion of the semen sample is scheduled for one day before this approximately, since ovulation occurs 36 hours within the hCG shot.
Semen collection and preparation
The semen sample is collected on the same day when insemination is going to be performed. Samples are obtained through masturbation after a period of sexual abstinence of between 3 to 5 days.
After the sperm is collected, it is processed using a technique called sperm capacitation. The goal is to concentrate the maximum number of high-quality sperm possible in a single sample. By doing this, immotile sperm are removed, along with the dead and seminal plasma.
In intercourse, this sperm selection process occurs naturally while sperm are traveling along the female reproductive tract. When this is done at the lab, the selection process becomes easier and the chances of success are increased.
Then, the capacitated sample is inserted using an insemination cannula.
In case the technique used is Artificial Insemination by Donor (AID), the semen sample must have been frozen for a minimum period of 6 months. Thus, it will be thawed on the insemination day. Sperm capacitation can be done either prior to being frozen or post thaw.
Semen samples might be frozen for other reasons. In such cases, the process to follow is the same as in cases of AID.
Get more info by clicking the following link: What Is Capacitation of Sperm Cells? – Definition & In Vitro Techniques.
Insemination
To carry out the insemination step, the woman has to get into a position that is comfortable for her. Then, the OB/GYN inserts a cannula that has been pre-loaded with spermatozoa through the vagina until it reaches the uterus. Once there, they are placed gently inside the uterine cavity.
To be able to visualize the pathway of the cannula and control the place where sperm are placed, insemination is done aided by an ultrasound. This, at the same time, prevents the uterine walls from being scratched during the procedure, which could affect embryo implantation.
This process is not painful at all. In fact, it is similar to a gynecological examination or Pap smear.
Semen is able to remain alive once it gets inside the female reproductive tract from 3 to 5 days, while an egg has a lifespan of just 24 hours.
For this reason, insemination must be carried out after triggering ovulation using the hCG hormone, since this way we ensure the egg-sperm binding occurs inside the female reproductive tract.
Other insemination techniques
Although they are becoming less frequent over time, there exist other types of artificial insemination aside from IUI:
- Intratubal Insemination (ITI)
- The semen sample is placed directly in the Fallopian tube. ITI is uncommon because it requires greater assistance from the specialist, which does not correlate with an increase in the success rates.
- Intracervical Insemination (ICI)
- Sperm are placed in the cervix, so their journey toward the Fallopian tube will be longer.
- Intravaginal Insemination (IVI)
- The sperm is placed in the vaginal fundus, as in normal intercourse. This type of insemination is used when the man is unable to ejaculate inside the vagina due to issues such as sexual impotence or retrograde ejaculation.
- Intrafollicular Insemination (IFI)
- Sperm are put directly inside the follicle, that is, around the egg cell. IFI is has almost fallen into disuse, since it is a technically challenging procedure and might cause damage to the patient more easily. Moreover, the success rates are the same as IUI.
What to do after AI
After insemination, rest is recommended for about 15-30 minutes. Then, she can continue with her normal lifestyle, although avoiding excessive efforts and stressful situations.
On the other hand, women are usually prescribed additional progesterone doses, administered in the form of vaginal pessaries. This is due to improve endometrial quality (inner layer of the uterus), favoring embryo implantation.
Within 12-15 days after being inseminated, the woman can undergo a blood analysis to detect the presence of hCG levels. With this, patients can guess if embryo implantation has occurred or not, and therefore if they are pregnant.
It is crucial for patients to be patient and wait for a reasonable period of time before taking a pregnancy test. Doing it too early can lead to mistaken results (false positives and false negatives).
A blood test will be done to look for high levels of a hormone called beta-HCG one or two weeks later. Such test will determine whether implantation has occurred or not and, thus, if the insemination has been successful and pregnancy has been achieved.
In case there is a negative pregnancy test, artificial insemination can be performed again this time changing the stimulation pattern or monitoring the time of ovulation as accurate as possible.
Cost
The cost of intrauterine insemination varies from clinic to clinic. However, in general, it is one of the cheapest fertility treatments in comparison with more complex techniques such as IVF or IVF/ICSI.
In the United States, for example, the cost of AIH can be as low as $300, although this does not include the cost of medications. Some clinics offer special plans and discounts for second and subsequent attempts.
Did you know that we can help you to choose a fertility clinic for your IUI cycle? All you have to do is get your Fertility Report now. It is an easy-to-use tool that is capable of filtering the best clinics and tailor an individual report exclusively for you with useful tips that will help you make a well informed decision.
In the UK, patients might be eligible for NHS-funded IUI in some cases. However, the average cost is £500-1,000 per cycle. In other European countries, such as Spain, it ranges between €600 to €1,000.
IUI step-by-step process video
Ana Fernández, gynaecologist at Fertility Madrid, talks to us in this video about each of the stages involved in the artificial insemination process.
As the doctor tells us:
When we are doing an intrauterine insemination (IUI) we want to do a mildly stimulation to simulate the natural process of oocyte development.
FAQs from users
Is it necessary to wait for the arrival of the period to make an AI?
Artificial insemination or AI is one of the best known treatments in Assisted Reproduction.
It is a simple and minimally invasive technique, which consists of introducing a semen sample into the mother's uterus. For this, it is important that ovulation is taking place at that moment, for which ovarian stimulation is often used. In addition, the sperm deposited are previously capacitated in the laboratory, i.e. those with the highest fertilisation potential are selected.
As in any fertility treatment, in Artificial Insemination (AI), the monitoring begins in the first three days of the menstrual period and ends with the pregnancy test in blood four weeks later.
The first day of the menstrual cycle is the day of heavy vaginal bleeding, where the hormone levels of oestrogen and progesterone should be low. This triggers the start of the hormonal cycle and the response of the pituitary gland in the brain to begin production of the follicle-stimulating hormone (FSH) necessary for follicle recruitment and subsequent ovulation.
Even with irregular hormonal cycles, the first day of the period marks the start of the menstrual cycle.
What implantation symptoms will I experience after IUI?
If you undergo IUI (intrauterine insemination) and it is successful, the embryo will adheres to your endometrium as if pregnancy has occurred naturally, that is, by means of intercourse. So, taking this into account, the symptoms and signs you are likely to notice are exactly the same as in any other woman.
How long does the IUI process last?
Counting from the moment of insemination, the duration of the procedure is just 15 minutes plus a rest time of 15-30 minutes. On the contrary, if we consider the entire procedure, including the ovarian stimulation phase, it can be extended up to two months:
- One month to monitor the cycle using contraceptives
- Two weeks of ovarian stimulation until the day of ovulation
- One day for the insemination procedure itself
- About two weeks (i.e. two-week wait) before taking a pregnancy test
In any case, since we depend on each woman's response to medications as well as her particularities, these time frames may vary slightly.
Should the ovarian cycle be regulated before IUI?
Although it is common that the menstrual cycle is monitored closely before getting started with the IUI cycle, this step is not always taken.
Commonly, gynecologists prescribe a treatment based on hormonal birth control a month before the day of insemination, since it helps to regulate the menstrual cycle and makes the process easier. However, if the woman has very regular menstrual cycles, this process might be unnecessary.
Can you do artificial insemination without ovarian stimulation, that is, without taking hormone medications?
Yes. The process is known as natural cycle intrauterine insemination. It involves monitoring when ovulation is going to take place naturally through ultrasound scan in order for the insemination to be done on the same day or the previous day.
The chances of success are almost the same as those achieved with sexual intercourse, perhaps a little bit higher due to sperm capacitation.
What is the difference between single and double intrauterine insemination?
Both types of insemination are carried out with the same frequency. The main difference is the moment when the hCG shot is injected to trigger ovulation. Also, in double IUI, the woman has to visit the clinic two days in a row to repeat the process.
What are the risks of intrauterine insemination?
As indicated above, the process is simple and, therefore, the risks and complications associated are almost non-existent. The only risks that might occur are those associated with ovarian stimulation.
For this reason, it is crucial that the cycle is closely monitored by a specialist that can measure the response of each woman individually. Depending on it, the medication protocol can be readjusted.
On the other hand, ovarian development is monitored to prevent a multiple pregnancy. This type of pregnancy is more risky for both the woman and the babies.
Suggested for you
As explained above, a intrauterine insemination process is a key step in all intrauterine insemination (IUI) procedures. It typically lasts 10-12 days. Get more info here: Artificial Insemination (AI) Using Ovulation Induction.
Also, preparing the semen sample before using it is crucial in order to optimize the chances of success. The following article can provide you with further insight on this key step of the process: What Is Capacitation of Sperm Cells? – Definition & In Vitro Techniques.
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
Allegra A, Marino A, Coffaro F, Scaglione P, Sammartano F, Rizza G, Volpes A (2007). GnRH antagonist-induced inhibition of the premature LH surge increases pregnancy rates in IUI-stimulated cycles. A prospective randomized trial. Hum Reprod; 22: 101 – 108 (View)
Boomsma CM, Heineman MJ, Cohlen BJ, Farquhar C (2007). Semen preparation techniques for intrauterine insemination (Review). Cochrane Database Syst Rev; Art No.: CD004507 (View)
Goldberg JM, Mascha E, Falcone T, Attaran M (1999). Comparison of intrauterine and intracervical insemination with frozen donor sperm: a meta-analysis. Fertil Steril; 72(5):792-5 (View)
Gomez-Polomares JL, Juliia B, Acevedo-Martin B, Martinez-Burgos M, Hernandez ER, Ricciarelli E (2005). Timing ovulation for intrauterine insemination with a GnRH antagonist. Hum Reprod;20:368 – 372 (View)
Ragni G, Somigliana E, Vegetti W. (2004) Timing of intrauterine insemination: where are we? Fertil Steril;82:25 – 26 (View)
The ESHRE Capri Workshop Group (2009). Intrauterine insemination. Human Reproduction Update; 15 (3): 265–277.64
FAQs from users: 'Is it necessary to wait for the arrival of the period to make an AI?', 'What does the ovarian stimulation phase of IUI look like?', 'What controls are carried out throughout an IUI cycle?', 'When should the partner collect the semen sample for IUI?', 'At what point does IUI take place?', 'Can the woman continue her daily routine after IUI?', 'What implantation symptoms will I experience after IUI?', 'How long does one have to wait for pregnancy test afer IUI?', 'How long does the IUI process last?', 'Should the ovarian cycle be regulated before IUI?', 'Can you do artificial insemination without ovarian stimulation, that is, without taking hormone medications?', 'What is the difference between single and double intrauterine insemination?' and 'What are the risks of intrauterine insemination?'.
Authors and contributors