Teratozoospermia, sometimes called teratospermia, is defined as abnormal sperm morphology. It is a sperm disorder that causes males affected to produced abnormally shaped sperm.
The pregnancy rate in males affected by teratozoospermia depends on the grade of severity. It is considered a cause of male infertility, and its causes are varied or even unknown.
There exist various treatment options to have a baby with abnormal sperm morphology. The chances of success depend on the remaining sperm parameters, as teratozoospermia may be combined with other pathologies, like sperm count or sperm motility.
Provided below is an index with the 9 points we are going to expand on in this article.
- 1.
- 1.1.
- 2.
- 3.
- 4.
- 4.1.
- 5.
- 5.1.
- 5.2.
- 6.
- 6.1.
- 6.2.
- 6.3.
- 6.4.
- 6.5.
- 6.6.
- 6.7.
- 6.8.
- 7.
- 8.
- 9.
Definition
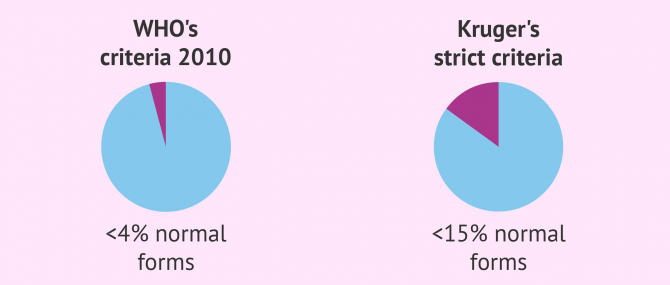
Teratozoospermia is the medical term used to refer to abnormal sperm morphology, caused by either defects in the head, midpiece, and/or tail. According to the criteria published in 2010 by the World Health Organization (WHO), a man has teratozoospermia when more than 96% of the sperms he produces are abnormally shaped.
Although the World Health Organization (WHO) has published an update of the Laboratory Manual for Semen Examination and Processing in 2021 (the sixth edition), the most common practice is to continue to follow the criteria of the fifth edition (2010).
If at least 4% of sperms have a normal shape, the male is considered fertile and able to make a woman naturally.
Teratozoospermia according to Kruger's criteria
Some laboratories use the Kruger's strict criteria to evaluate a semen sample as well as those of the WHO.
According to Kruger's strict criteria, teratozoospermia is present when more than 85% of spermatozoa have an abnormal shape. This criteria is far stricter than the ones published by the WHO.
In other words, the borderline to consider whether a man has teratozoospermia is set at a minumum of 15% of spermatozoa with normal forms instead of 4%, which is the percent currently established by the WHO.
Unless otherwise specified in your semen analysis report, it is according tp the critieria set by the WHO's 2010 and not that of Kruger.
What causes teratozoospermia
Teratozoospermia is associated with male infertility in all cases, as it means that sperm are unable to get to the egg due to their abnormal shape.
The causes of abnormal sperm morphology are varied and in most cases difficult to determine. The following are the most common ones:
- Genetic traits
- Cancer treatments (chemotherapy and radiotherapy)
- Bacterial infections in sperm and orchitis
- Testicular trauma
- Testicular disorders, like varicocele
- Fever
- Diabetes mellitus (DM) or meningitis
- Tobacco, alcohol and street drug use
- Unhealthy habits: unbalanced diet, exposure to toxic substances, too tight clothes, etc.
The good news is that teratozoospermia can be cured in some of these cases. For example, if caused by fever, infections, or stress, the man is likely to start producing normal sperm again once these conditions disappear. If the cause is associated with unhealthy habits, picking up healthier habits such as following a balanced diet, quitting smoking, etc. can improve sperm quality.
You can read more about this in the following article: What are the causes of teratozoospermia?
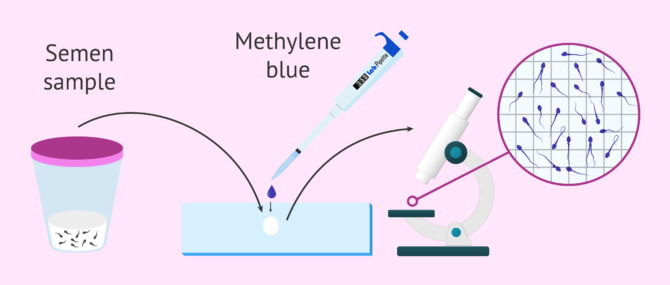
Diagnosis
When a man has teratozoospermia he will not feel any pain. Therefore, the way to diagnose this seminal alteration is by means of a seminogram. In this study a specialist will study the shape of the spermatozoa in the andrology laboratory.
To do this, the specialist will stain a drop of semen and observe the morphology of the stained spermatozoa under the microscope. The most common way to stain spermatozoa is using methylene blue dye.
Generally, 200 spermatozoa are studied to get a representative sample and work out the percentage of abnormal spermatozoa.
A spermatozoon is normal when it has an oval-shaped head and an acrosome inside. The neck or midpiece is slightly thicker than the tail and, finally, the tail is elongated and uncoiled.
If you are interested and want to read more detailed information, you can visit this link: How can teratozoospermia be diagnosed?
What different types of teratospermia are there?
Defects in the morphology of sperm can be classified into different types depending on their location - head, midpiece, and/or tail. However, before diagnosing teratozoospermia, all abnormalities are taken into consideration.
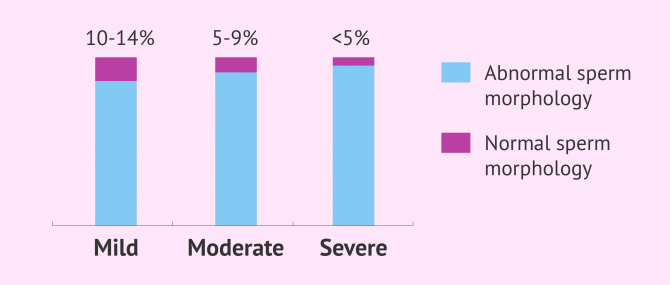
After examining sperm morphology with a semen analysis, it is possible for the specialist to determine the type of teratozoospermia and its grade of severity. For this purpose, the Kruger criteria are used and teratospermia is classified into three grades:
- Mild teratozoospermia
- Between 10% and 14% of sperm have a normal morphology.
- Moderate teratozoospermia
- The percentage of sperm with normal morphology ranges between 5% and 9%.
- Severe teratozoospermia
- Normal morphology is present in less than 5% of sperm.
As mentioned earlier, the criteria used to diagnose teratozoospermia are the ones published by the OMS. In other words, this classification has fallen into disuse. However, it is still possible to find them in the results of some sperm analyses.
For more information on this, we encourage you to read the following article: Teratozoospermia types - mild, moderate and severe.
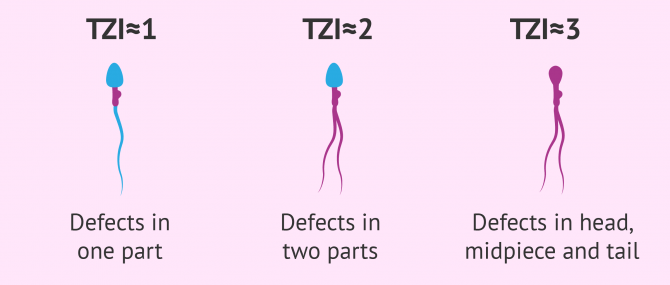
Teratozoospermia index
This measurement is used to identify the number of defects present in each sperm cell. It is possible for a sperm to have an anomaly in just one part, or in multiple areas.
To calculate the teratozoospermia index (TZI), we use the following formula: TZI = ( c + p + q ) / x, where each variable means:
- c = head defects
- p = midpiece defects
- q = tail defects
- x = total number of abnormal sperm
The TZI score should be interpreted as follows:
- TZI close to 1: One part affected
- TZI close to 2: Two parts affected
- TZI close to 3: Head, midpiece and tail affected
It should be noted that all three types can be found in a semen sample, that is, with sperm cells that have defects in one, two or all three parts. The TZI indicates which type is the most frequent one.
How to achieve pregnancy
A man with teratozoospermia can achieve a natural pregnancy as long as the remaining sperm parameters, particularly the sperm count and sperm motility, are normal.
Nevertheless, when a couple is trying to conceive but pregnancy it not happening, men can follow a series of medical tips in an attempt to improve the morphology of their sperm.
On the other hand, if teratozoospermia has a genetic origin or is present from birth (congenital), finding a treatment option that works may be harder.
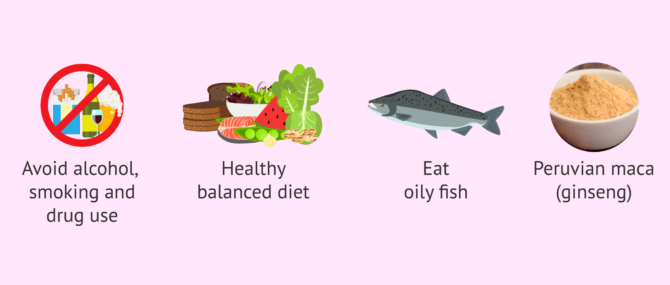
Natural treatments for teratospermia
First of all, men with teratozoospermia should change their lifestyle and quit unhealthy habits for their organism, such as cigarette smoking or alcoholic drinks.
Following a balanced diet is always key when it comes to improving one's fertility. Particularly, foods rich in antioxidants and essential amino acids like L-carnitine, which boosts sperm quality.
Oily fish is rich in omega-3 fatty acids as well, which is greatly beneficial for the reproductive health of males.
Also, all these vitamins and nutrients can be taken in the form of vitamin supplements like maca root powder or supplements containing vitamin E, which functions as a powerful antioxidant.
You can find more advice and recommendations in this article: TTreatment of teratozoospermia.
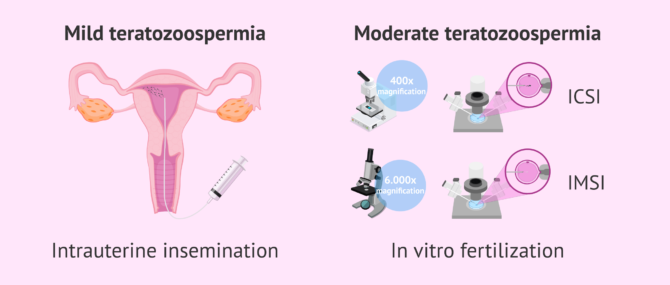
Assisted reproduction with teratozoospermia
Men with mild teratozoospermia who are unable to conceive a child should resort to assisted reproduction. In these cases, artificial insemination (AI), also known as intrauterine insemination (IUI) will be possible as long as the concentration and motility of the sperm are not altered.
IUI will be the first option to consider if the woman has no fertility problems and the only cause that prevents gestation is teratozoospermia.
On the other hand, in cases of moderate or severe teratozoospermia, or other alterations that cause sterility, it will be necessary to perform IVF-ICSI. This is an in vitro fertilization technique in which intracytoplasmic sperm injection is used to achieve fertilization of the eggs.
Finally, there exists a cutting-edge technique that is similar to ICSI. It is called IMSI (intracytoplasmic morphologically selected sperm injection), and involves the use of a high magnification light microscopy imaging method to see sperm morphology in detail.
If you need to undergo IVF to become a mother, we recommend that you generate your Fertility Report now. In 3 simple steps, it will show you a list of clinics that fit your preferences and meet our strict quality criteria. Moreover, you will receive a report via email with useful tips to visit a fertility clinic for the first time.
The microscope used in IMSI to select the best spermatozoon includes a lens for high magnification, which allows the specialist to see the potential defects that are present in each sperm cell in full detail.
More information on assisted reproduction with IMSI can be found in this article:Read: What Is Intracytoplasmic Morphologically Selected Sperm Injection (IMSI)?
FAQs from users
What is the cause of teratozoospermia?
Teratozoospermia is an abnormality affecting male semen in which most sperm are abnormally shaped.
Because of their poor morphology, sperm cannot fertilize the egg and cause sterility.
The causes of teratozoospermia are:
- Genetic alterations
- Chemotherapy and radiation therapy
- Seminal infections and orchitis
- Testicular trauma
- Varicocele
- Fever
- Diabetes Mellitus and meningitis
- Tobacco, alcohol, drugs
- Bad eating habits, toxic, tight clothing...
There are some causes that can be solved (fever, quitting tobacco, healthy habits...) so that the problem in some cases would be reversible.
Can leucospermia cause teratospermia and male sterility?
Leucospermia, also called leucocytopermia, is the appearance of leukocytes in semen at a concentration greater than 1 million per milliliter. The cause of this seminal disease is an infection in the male reproductive tract that must be treated with antibiotics since it can affect spermatogenesis and cause alterations such as oligospermia or teratozoospermia.
Should I use donor sperm if I have teratozoospermia?
In principle, we should not resort directly to a treatment with donor sperm without first trying in vitro fertilization techniques with your own sperm.
However, if it is a severe teratozoospermia or if gestation is not achieved using the patient's own sperm, the alternative would be to opt for donor sperm.
Read more
What characteristics does a normal sperm have?
According to the World Health Organization (WHO), the characteristics that should present the ideal sperm, that is, with an excellent morphology are the following:
- Oval head and regular contour
- Single straight tail
- Fixed nucleus
- Transparent color
In principle, all sperm that meet these requirements have the capacity to fertilize the egg and lead to a viable pregnancy.
What are the consequences of having abnormal sperm in your semen?
The main consequence of teratozoospermia is the male infertility it causes, since amorphous sperm are not able to fertilize the egg or even present alterations in their DNA.
Read more
Can abnormal sperm morphology cause miscarriage?
In principle, poor sperm morphology doesn't lead to miscarriage once the egg has been fertilized and the embryo has attached to the womb. Another case would be that the sperm also contain genetic mutations as well as the abnormal morphology, which could lead to miscarriage.
How can I improve amorphous sperm in semen?
In the first place and as long as the cause of teratozoospermia is not a specific pathology, the male should follow some guidelines to modify his lifestyle, which may be interfering negatively in his reproductive state. Some men who give up habits such as tobacco or alcohol and follow a healthy diet see an improvement in their seminal quality after about 3 months.
Are teratozoospermia and necrozoospermia the same?
The answer is no. Teratozoospermia and necrozoospermia are seminal alterations, but each refers to a spermatic parameter.
On the one hand, teratozoospermia is an alteration in sperm morphology. In contrast, necrozoospermia refers to problems in the vitality of sperm, that is, when there are a lot of dead sperm in the ejaculate.
Recommended reading
There are other sperm disorders that can cause male infertility or at least complicate the TTC journey. Click here to learn more: Sperm Disorders that Cause Male Infertility.
A semen analysis is a method used by all andrology laboratories to evaluate sperm quality. To learn how it works and how to interpret the results, please click here: What Is a Semen Analysis Report? – Purpose, Preparation & Cost.
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
Auger J, Jouannet P, Eustache F. Another look at human sperm morphology. Hum Reprod. 2016;31(1):10-23 (View)
De Braekeleer M, Nguyen MH, Morel F, Perrin A. Genetic aspects of monomorphic teratozoospermia: a review. J Assist Reprod Genet. 2015;32(4):615-23 (View)
El Khattabi L, Dupont C, Sermondade N, Hugues JN, Poncelet C, Porcher R, Cedrin-Durnerin I, Lévy R, Sifer C. Is intracytoplasmic morphologically selected sperm injection effective in patients with infertility related to teratozoospermia or repeated implantation failure? Fertil Steril. 2013;100(1):62-8 (View)
French DB, Sabanegh ES Jr, Goldfarb J, Desai N. Does severe teratozoospermia affect blastocyst formation, live birth rate, and other clinical outcome parameters in ICSI cycles? Fertil Steril. 2010;93(4):1097-103 (View)
Lee RK, Hou JW, Ho HY, et al. Sperm morphology analysis using strict criteria as a prognostic factor in intrauterine insemination. Int J Androl. 2002; 25: 277-80. (View)
Marchini M, Ruspa M, Baglioni A, Piffaretti-Yanez A, Campana A, Balerna M. Poor reproductive prognosis in severe teratozoospermia with a predominant sperm anomaly. Andrologia. 1989;21(5):468-75.
Shabtaie SA, Gerkowicz SA, Kohn TP, Ramasamy R. Role of Abnormal Sperm Morphology in Predicting Pregnancy Outcomes. Curr Urol Rep. 2016;17(9):67.
World Health Organization (WHO) (2010). WHO laboratory Manual for the examination of human semen and sperm-cervical mucus interaction. Cambridge Academic Press.
FAQs from users: 'Why does teratozoospermia cause fertility problems?', 'What is the cause of teratozoospermia?', 'Can leucospermia cause teratospermia and male sterility?', 'Should I use donor sperm if I have teratozoospermia?', 'What characteristics does a normal sperm have?', 'What are the consequences of having abnormal sperm in your semen?', 'Can abnormal sperm morphology cause miscarriage?', 'What does 0 morphology mean?', 'How can I improve amorphous sperm in semen?', 'What does teratozoospermia actually mean?' and 'Are teratozoospermia and necrozoospermia the same?'.
Authors and contributors

More information about Michelle Lorraine Embleton



Hi Doctor,
The following is my sperm analysis. Pls suggest:
Volume: 2.5ml
Viscosity: Thin
Liquefaction Time: Normal
Fructose Test: Positive
Agglutination: Nil
Sperm Concentration: 40 million/ml
MOTILITY. Total: 80%
• RPM: 00%
• SPM: 45%
• NPM: 35%
• Non-Motile: 20%
MORPHOLOGY:
Normal Forms: 03%
Vitality: 81%
Round Cells: 1-2/HPF
Please suggest if I have any problem.
Regards
Hello Dev,
In terms of concentration, vitality and mobility, your semen sample is within de normal range. The only parameter that presents alterations is the morphology, which should be above 4%. This could imply some difficulties trying to achieve natural pregnancy, but it is not an alteration so severe to rule it out.
If you have been trying to conceive for less than 12 months you can keep doing it until you reach a year looking for it. Once you reach a year of searching, it is advisable to consult a specialist in fertility. The doctor will run some tests to both of you to determine if the cause of the infertility is the altered morphology or if there is some other factor involved. With all this information, he will be able to propose which treatment is the most suitable for your case.
I hope I have been able to help.
Regards.
My husband result:
Day of abstinence: 3
Volume 2.1 ml
Liquefaction: 15
Viscocity: normal
Colour : light yellow
Concentration : 84 x10^6
Total count: 197.4
Motility(%): 71.2
Progression : 2-2
Normal morphology : 3
Pus cell: occasional
Cellular debris: moderate
Clumping to cell debris: none
Tail to tail clumping: minimal
Head to head clumping: None
Analysis result: Teratozoospermia
What do you think of my husband result?
Shall I proceed with IUI ?
Hello Kean86,
All parameters are ok except for morphology. In order to be able to assess the severity of the situation, I need to know the method by which the morphology has been analysed. There are different methods that have different reference points. Mainly, there are two methods. The one established by the WHO says that the reference point is 4% of normal forms while Kruger morphology establishes it at 14% of normal forms.
In both cases the diagnosis is teratozoospermia, but depending on the method the diagnosis will be more or less severe. Since the rest of the parameters are normal, if the morphology has been assessed by the WHO method, the semen sample is good enough to be used in an IUI. If it has been assessed by the Kruger method, it could be preferable to choose IVF.
As a final note, the female fertility should be taken also into account in order to choose the most suitable technique for you.
I hope I have been able to help.
Regards.
My wife and I have been trying to conceive for 5 years but we haven’t used any substance to prevent this for the past almost 12 years.
Sperm Concentration (mil/ml) 200.00
Percentage Normal Morphology 16%
Percent Teratozoospermia 84%
Teratozoospermis- Description 54% mixed head defects
Percent Motile 90%
Pro-normal 40%
Pro-slow 50%
Non-pro 10%
Shaking (in place) 0%
Color grey
Odor normal
Volume (ml) 1.8
pH 8.0
Viscosity Normal
Liquification Normal
Dear Isaac,
All the parameters that the sperm analysis shows are within the normal range. Taking into account how long you have been trying to conceive I recommend that you visit a fertility specialist. The doctor will run some tests, on your partner and yourself, in order to determine the cause of your fertility problems.
Best wishes.
Hello,
My husband semen analysis result is remarks: teratozoospermia
Appearance:4.5%
Ph:7.5ml
Liquefaction:normal
Viscosity:normal
Total motility:70%
Progressive:59%
Non-progressive:11%
Immotile:30%
Concentration:83M
Total sperm count:373.5M
Morphology:4%
Leucocytes:0-1 HPf
What does this mean?
Please help us… thanks!
Dear Anna,
The diagnosis of teratozoospermia means that the morphology of the spermatozoa is altered and, for example, the head or the tail has an abnormal shape. Those spermatozoa with altered morphology can not swim properly, which hinders its arrival to the Fallopian tube, where fertilization takes place. In case that an abnormal spermatozoon reached the oocyte, it would not be able to fertilize it properly. Finally, a high percentage of abnormal spermatozoa carries chromosomic alterations that, in case of fertilization, might lead into an altered embryo that will not implant in the uterus or that will end in an early miscarriage. For those reasons, it can be difficult for you to conceive naturally.
Those abnormal spermatozoa can be eliminated from the semen sample in the lab when it is prepared for an assisted reproduction technique. For that reason, it is advisable to contact a fertility specialist so that he can asses you. The doctor will evaluate all your fertility tests and decide which is the best option in your case. The rest of the seminal parameters are normal, which will allow you to use any technique.
I hope I have been helpful.
Hello Dr.,
My husband semen analysis details:
Liquefaction:. Normal
Appearance:. White gray
Viscosity:. Normal
Volume:. 3.0 ml
Ph:. 8.0
White blood cells:. Abnormal
Concerntration: 25.4 mil/ml
Motility:. 50%
Progressive motility:. 35%
Non-Progressive motility:. 15%
Immotile:. 50%
Viability:. 55%
Normal Morphology:. 45%
Total sperm count:. 76.20 mil/ejac
Please guide us. Is it normal?
Dear Ruty,
All parameters are within the normal range except for the white blood cells count. Since the presence of white blood cells might be a sign of infection, the doctor might recommend antibiotic treatment. In any case, it is not a fertility problem and you should not have problems trying to conceive.
Best regards
Hello Dr.,
My husband semen analysis details:
Volume:. 6.0 ml
Concentrațion : 12 x 10^6/ml
Normal forms : 2%
Liquefaction : Complete
Viscosity : Normal
Total number : 72 ( 10^6)
Progressive :52%
Non – progressive 7%
Non -motile 41%
What does that mean ?
Please help us … thank you !
Dear Maria S,
First of all, I want to point out that the volume is quite elevated. This itself is not a fertility problem but it causes that concentration might seem altered when it is not. Usually, the reference value for concentration is at least 15 x 10^6 / ml. In the case of your husband’s analysis it is under this value. But if you take a look at the total number, the result is excellent since the reference value is at least 39 millions. This means that your husband does not have a sperm quantity problem but, because of the elevated volume, the sample is really diluted, giving the false appearance of a low concentration sample. To sum up, concentration is not a major concern.
The other parameter that appears altered is morphology. The percentage of normal forms is quite low. This means that you might have some trouble getting pregnant. If you have been trying to conceive for more that 12 months you should visit a fertility specialist in order to decide the best treatment. If you have been less that this period of time, and you are younger than 36, you can keep trying for a little bit longer.
I hope I have been able to help,
Best wishes
Hello Dr.
My semen analysis are given below:
Fresh:
Volume : 4.0 ml
Concentration : 19 million/ml
Progressive Motility : 35%
Grade : 2+
Total Count : 76 million
Washed:
Volume : 1.0 ml
Concentration : 20.4 million/ml
Progressive Motility : 76%
Grade : 3+
Total Count : 20.4 million
TMF : 15.5 million
Kruger’s criteria : 1%
Is it normal ? If not what should I do for become a father. Please guide me.
Regards
Hi Reza,
Volume, concentration and motility seem to be within the normal range. The only parameter that seems altered is morphology. Kruger’s criteria is used to evaluate normal morphology and, even though it does not say if the percentage refers to the normal proportion or to the abnormal one, I assume that it is referring to the normal percentage. Therefore, normal morphology is lower than it should be and it might reverberate into fertility problems.
If you have been trying to conceive for more than 12 months you should go to a fertility specialist, in order to run more tests and establish which would be the most suitable treatment for you. If you have not tried for 12 months yet, and your partner is younger than 36 years old, you can continue until you reach one year search.
I hope I have been able to help,
Regards