Teratozoospermia or teratospermia refers to the presence of poor sperm morphology in the semen.
This sperm disorder is a cause of male infertility, since abnormally shaped sperm are unable to reach and fertilize the egg or, if they are so, embryo development issues are likely to occur.
There are no symptoms associated with teratozoospermia that could be recognized by the man suffering from it. Thus, the only possible method available to detect this sperm disorder is by examining a sperm sample at the Andrology Lab through a semen analysis.
Provided below is an index with the 7 points we are going to expand on in this article.
- 1.
- 1.1.
- 1.2.
- 2.
- 3.
- 4.
- 4.1.
- 4.2.
- 4.3.
- 4.4.
- 4.5.
- 5.
- 6.
- 7.
What is a semen analysis?
A semen analysis, also called semenogram, seminogram, or sperm test, is a key diagnostic test to evaluate male fertility.
It is a comprehensive analysis of the semen where multiple parameters are evaluated. The following are the most important ones:
The results of a basic semen analysis can provide us with a vast amount of valuable information about the male's fertility.
Fertility treatments, like any other medical treatment, require that you trust the fertility specialists that will be by your side during your journey. Logically, each clinic has a different work methodology. Our Fertility Report will offer you a selection of recommended clinics, that is, fertility centers that have passed our rigorous selection process. Moreover, our system is capable of comparing the costs and conditions of each one so that you can make a well-informed decision.
Particularly, the number of sperm with abnormalities in their morphology will indicate if there is teratozoospermia or not.
Teratozoospermia according to WHO's criteria
When a semen sample is analysed and a large number of spermatozoa with amorphous forms are observed, the diagnosis is teratozoospermia.
Although the World Health Organisation (WHO) has published an update of the Laboratory Manual for Semen Testing and Processing in 2021 (the sixth edition), the criteria of the fifth edition (2010) are the most common..
Therefore, a man is considered to have good sperm morphology when he has at least 4% of spermatozoa with a normal shape. Therefore, in order for a man to be considered to have teratozoospermia, more than 96% of his spermatozoa must have alterations in the head, neck or tail.
Teratozoospermia according to Kruger's strict criteria
It is possible that certain andrology labs use different reference values from those published by the WHO to examine sperm morphology.
We are referring to Kruger's strict criteria, which consider that a man has teratozoospermia when more than 85% of his sperm have an abnormal morphology.
Conversely, a man is considered fertile when 15% or more of his sperm have a normal shape.
Kruger's strict criteria, as the name suggests, are stricter than the guidelines of the OMS. Thus, a man can be diagnosed with teratozoospermia according to Kruger, whilst his sample can be considered normal if the OMS criteria are used. This is the case of teratozoospermia with values between 4 y 14%.
Analysis of sperm morphology
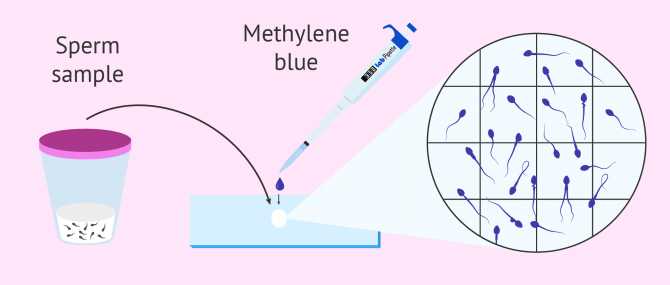
During a semen analysis, doing a dye test of a drop of semen is necessary to observe the morphology of sperm under the microscope.
Even though there exist as many types of stains as andrology laboratories, the Diff-Quick stain is one of the most commonly ones used. This technique uses a stain set that contains an aqueous solution of methylene blue that allows for sperm cell nuclei to appear stained in an either intensely dark blue or dark violet color, thereby allowing the structures to be visible.
The ideal sperm cell, according to the WHO, has an oval-shaped head with an acrosome inside, a middle-piece slightly enlarged, and a long tail that allows it to move.
In order to be able to determine whether a sperm has a normal or abnormal shape, andrologists must take the following criteria into account when examining each part of the sperm:
- Head
- A normal sperm has an oval head, with a regular contour. The acrosome should cover between 40 and 70% of the head's volume, and be placed in the distal edge. The presence of vacuoles should be below 20%.
- Middle-piece
- It should be linear and be connected to the head on the axial part (opposite to the acrosome). Its normal length is 1.5 times bigger than the head. Moreover, it should be thinner than the head, but thicker than the tail ideally.
- Tail
- It is the thinnest, longest part of sperm cells. The length should be 50 micra and be uncoiled.
In order to calculate the percent of abnormal sperm, the specialist usually counts 200 sperms under the microscope while determining their quality. Then, the percent of each one of the anomalies detected is determined, as well as the total percentage.
There exist more innovative methods to evaluate seminal parameters and sperm morphology more quickly, known as CASA systems (Computer Assisted Semen Analysis). Nonetheless, these methods are far from being common practice amongst fertility clinics nowadays.
Semen analysis results
As explained above, each lab should specify the criterion used to perform the semen analysis, that is, the Kruger's or the WHO's criteria.
Typically, semen analysis reports include a table with the total sperm count and the percent of each parameter. Sometimes, they include charts to make it more understandable by the patient.
Aside from the percent of normal and abnormal sperm, the number of anomalies present on each part of the sperm cell (head, neck/middle-piece, and tail) is included as well.
Out of the number of malformations detected on each part of the sperm, the specialist can determine another parameter: the teratozoospermia index (TZI).
The following is the formula used to calculate it: TZI = ( c + p + q ) / x, where each variable of the equation equals:
- c = anomalies in the head
- p = anomalies in the middle-piece
- q = anomalies in the tail
- x = total abnormal sperm count
The TZI ranges from 1 to 3, where 1 refers to anomalies present in one part of the sperms, and 3 refers to anomalies in all parts of the sperm cell (head, neck, and tail). Simply put, the higher the TZI, the the more severe the case of teratozoospermia.
FAQs from users
Can I have children with 3% normal-shaped sperm?
Yes, pregnancy can be achieved with a percentage of 3% normal spermatozoa, although it is likely that assisted reproduction techniques will have to be used.
Natural pregnancy with teratozoospermia (abnormal spermatozoa) can be complicated. In the most severe cases of altered sperm morphology, it is practically impossible for fertilisation and subsequent embryo development to take place.

Men with infertility due to severe teratozoospermia will have to resort to assisted reproductive techniques in order to become fathers. Although if the alteration in morphology is slight, it is not a very reliable predictive factor for achieving pregnancy, it is another parameter that must be taken into account in the clinical context of each couple and will depend on the rest of the semen parameters, the woman's age, her ovarian reserve and general state of health, among others.
What is the definition of teratozoospermia according to Kruger's strict criteria?
To diagnose a sperm sample as teratozoospermic, today labs use the WHO's criteria, which indicate that a man has teratozoospermia if more than 96% of sperm are abnormally shaped.
However, some labs continue using Kruger's strict criteria to evaluate sperm morphology. According to Kruger's, a man is teratozoospermic if more than 85% of the sperm are abnormal.
Can you be diagnosed with teratozoospermia and azoospermia at the same time?
No, it is not possible. Azoospermia is a sperm disorder whereby no sperm are found in the semen. Thus, given that no sperm is found under the microscope we cannot guess if morphology is normal or not. In fact, in cases of secretory or non-obstructive azoospermia, there is no single sperm in the ejaculate.
Learn more: Azoospermia – Can a Man Actually Have Zero Sperm Count?
How much does it cost to get a sperm analysis?
The general rate for a lab semen analysis in the United States of America ranges between $100 and $300, although it varies from US state to state.
In the United Kingdom, a basic semen analysis costs £130 approximately. Finally, in Canada, it costs 250 CAD on average.
What does it mean if your teratozoospermia index is 1.6?
The teratozoospermia index (TZI) refers to the total number of areas that affect each abnormal sperm, that is, the head, neck, and tail. Thus, is the TZI ranges between 1 and 2, if means that sperms can have either one or two parts affected. It can also indicate that they present abnormalities in 3 different parts, although this case is uncommon.
Suggested for you
There exist multiple types of sperm abnormalities that affect both the structure and morphology of sperm cells. To lear more, click here: Types of Sperm Abnormalities.
A semen analysis is the most important diagnostic test for males to evaluate their semen and subsequently their fertility. To get more info about this, we recommend that you visit this article: What Is a Semen Analysis Report?
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
Aziz, N., Sharma, R. K., Mahfouz, R., Jha, R., & Agarwal, A. Association of sperm morphology and the sperm deformity index (SDI) with poly (ADP-ribose) polymerase (PARP) cleavage inhibition. Fertility and Sterility, 2011;95(8), 2481-2484 (View)
Gatimel N, Moreau J, Parinaud J, Léandri RD. Sperm morphology: assessment, pathophysiology, clinical relevance, and state of the art in 2017. Andrology. 2017;5(5):845-862 (View)
González R, Quintana J, Campos I, Magán R, Ballesteros A. Estudio de la pareja estéril. En Remohí J, Bellver J, Domingo J, Bosch E, Pellicer A. Manual práctico de esterilidad y reproducción humana. Editorial McGraw-Hill-Interamericana 2008:1- 8.
World Health Organization (WHO) (2021). WHO laboratory Manual for the examination of human semen and processing of human semen (View)
FAQs from users: 'Can I have children with 3% normal-shaped sperm?', 'What is the definition of teratozoospermia according to Kruger's strict criteria?', 'Can you be diagnosed with teratozoospermia and azoospermia at the same time?', 'How much does it cost to get a sperm analysis?' and 'What does it mean if your teratozoospermia index is 1.6?'.






Hi there! Not understanding my partner’s… head defects 48%, neck 37% and tail 15%. Does this indicate good or not? Been trying for a year now.
Dear Sarah,
One of the parameters that are analysed in a spermiogram is morphology. Depending on the percentage of normal spermatozoa the diagnosis will be normal semen analysis or teratozoospermia. Usually, on the medical report it is also analysed which kind of abnormalities can be found among the abnormal spermatozoa: head defects, middle piece defects, neck defects or tail defects.
In your case you have to check if those percentages that you explain refer to the totality of the spermatozoa in the sample or just to those that have an abnormality. By this I mean that 48%, 37% and 15% sum up 100%, and it would be the same result if this 100% refers to the whole sample or just to the fraction of abnormal spermatozoa.
I hope I have been able to help.
Best regards