Teratozoospermia is a sperm disorder that refers to poor sperm morphology in the semen. It causes male infertility, since it prevents natural pregnancy.
Sperm malformations can be present in the head, neck/midpiece, and/or tail. Deformities occur as a result of alterations during spermatogenesis (sperm production process).
Provided below is an index with the 7 points we are going to expand on in this article.
- 1.
- 2.
- 2.1.
- 2.2.
- 2.3.
- 3.
- 4.
- 4.1.
- 4.2.
- 4.3.
- 4.4.
- 4.5.
- 5.
- 6.
- 7.
Abnormal sperm morphology
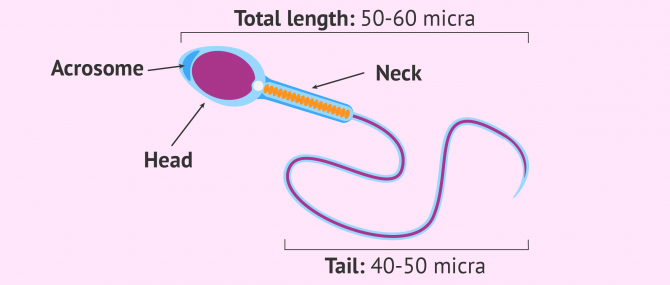
The World Health Organization (WHO) defines the ideal sperm morphology as follows:
- Oval head, and well-defined acrosome region in the apical part (upper part). If there are vacuoles, they cannot be greater than 20% of the head's area.
- The neck is connected to the head on its axial part (opposite to the acrosome region). The length of the midpiece should be 1.5 times larger than the head.
- The tail should be 45-50 micra long, and thinner than the remainder of the sperm cell.
- The total length of the sperm cell should range between 50 and 60 micra.
Sperm that exceeds or does not fit into these parameters are considered amorphous or abnormal.
You may also enjoy some further information reading this: What’s the Function of a Sperm Cell? – Definition & Structure.
Types of sperm morphological defects
Now that we have learned about the appearance of a normal sperm cell, that is, a sperm with normal morphology, we are going to explain the different types of morphological defects that may occur:
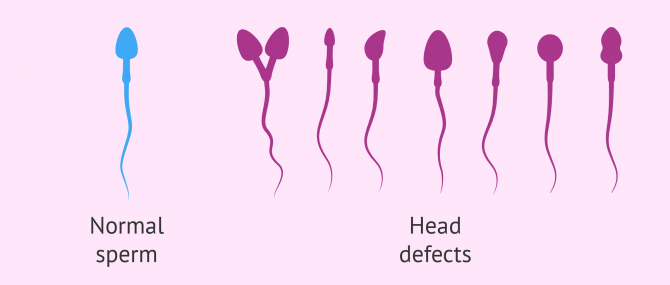
Head defects
The main amorphous types of sperm in relation to the head are: too large or too small head, elongated head, pyriform sperm, vacuolated head (over 20% of the total volume is occupied by vacuoles), too small vacuole area (the acrosomal area is smaller than 40% of the head), and double-headed sperm.
Sometimes, sperm have defects in the development of the acrosomal region, which affects morphology by causing a head that is too small and round-shaped. This condition is called globozoospermia.
Another kind of sperm morphological defect caused by adhesion issues between the acrosome and the nucleus is the one causing the head and the tail to be too separated. As a result, the head is absorbed and only "tails" remain in the semen, causing the sperm to be pin-headed.
Midpiece defects
Examples of morphological defects in the neck or midpiece include: bent neck (the neck and tail form an angle that is above 90° in comparison to the longitudinal axis of the head), asymmetrical insertion of the neck in the head, too thick or too thin neck, or irregular neck.
Also, the absence of mitochondria within the midpiece is considered another type of abnormality. Mitochondria are responsible for providing the necessary energy for sperm to move back and forth.
Tail defects
The tail of sperm can have several defects, in which case motion is the main parameter affected. Amongst the different types of deformities that we can find, having a too short tail, sperm with a duplicate tail, multiple tails, coiled tail, and a tail of irregular thickness are the most common ones.
The good news is that most of these abnormalities do not prevent sperms from reaching and fertilizing the egg cell, thereby resulting in a viable embryo. Nonetheless, tail defects cause a sperm disorder known as asthenoteratozoospermia, where morphology and motility are affected.
Number of alterations
When teratozoospermia or teratospermia is detected in a sperm sample, the personnel of the Andrology lab writes down the percentages of each one of the anomalies found per region, thanks to a staining procedure that allows the sperms to be seen microscopically.
When the semen analysis is concluded, they can calculate what is known as Teratozoospermia Index (TZI), a key diagnostic value to evaluate male fertility.
TZI is an indicator of how severe each case of teratospermia is, since it gives us information on the number of morphological defects in each sperm cell. For example, if sperm has defects in both the head and tail, the TZI will be higher than in those with defects only in one region like the head.
The TZI is calculated using the following formula: TZI = ( c + p + q ) / x, where each item is equivalent to:
- c = head defects
- p = midpiece defects
- q = tail defects
- x = total amount of abnormal sperm
The TZI can range between 1 and 3. When the result is close to 1, it means that the majority of sperms have anomalies in just one part of their structure. However, values above 1 indicate that more than one parts are defective. If the result is 3, sperms have defects in the head, neck, and tail, which aggravates the situation of infertility.
Considering undergoing a fertility treatment? By getting your individual Fertility Report your will see different clinics especially selected for you out of the pool of clinics that meet our strict quality criteria. Moreover, it will offer you a comparison between the fees and conditions each clinic offers in order for you to make a well informed choice.
FAQs from users
What types of semen anatomical abnormalities exist?
Potential defects or anomalies that can be found in sperm include:
- Head defects
- too small, too large, double-headed, balloon-shaped, with too large vacuoles...
- Midpiece defects
- too thin, too thick, too short, too long, bent, without neck...
- Tail defects
- too short, too long, duplicate tails, coiled, detached tail...
A single spermatozoon can have just one anomaly or, conversely, multiple defects.
In any case, with just an abnormality in one part, the sperm cell is considered an abnormal one.
Can abnormal sperm morphology fertilize an egg?
Yes, as long as it is a mild case of teratozoospermia. In moderate or severe cases, techniques such as ICSI or even IMSI, in which the specialist inserts the sperm cell manually into the egg, would be needed.
What happens if a sperm has two heads?
Double-headed sperm are non-viable. They are unable to fertilize the egg and result in viable embryos. Thus, they are always dismissed in IVF cycles. When a sperm has two heads, the genetic material is also duplicated, which results in triploid embryos. When this happens, embryonic arrest occurs a few days following fertilization anyway.
What is the meaning of globozoospermia?
Globozoospermic sperm resemble a balloon, hence the name (from globe (from Latin globus, ‘spherical object’). These sperm lack an acrosome, a small deposit located at one end of the head, and which contains a substance that is able to weaken the egg coat, allowing the sperm to penetrate it.
For this reason, balloon-shaped sperm cannot fertilize an egg either naturally or artificially with a fertility treatment like IUI or IVF. Only if ICSI is used, where the embryologist injects the sperm cell manually into the egg cell, fertilization with globozoospermic spermatozoa is possible.
In short, achieving a full-term pregnancy with globozoospermia is unlikely. Moreover, these sperms can carry genetic abnormalities.
How does a pinhead sperm look like?
In pinhead sperms, distinguishing the head from the midpiece is almost impossible.
This sperm defect is extremely serious, since the absence of head means that the sperm cell lacks genetic material. In other words, fertilization won't be possible in any way.
Suggested for you
Throughout this post, we have made various references to the diagnosis of teratozoospermia and morphological defects. If you are interested in delving deeper into this, click here: Diagnosis of Teratozoospermia.
Based on the type of teratozoospermia, a man may need to turn to a fertility treatment to have a baby or not. To learn more, read: Achieving Pregnancy with Teratozoospermia.
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
Auger J, Jouannet P, Eustache F. Another look at human sperm morphology. Hum Reprod. 2016;31(1):10-23.
Fujihara Y, Oji A, Larasati T, Kojima-Kita K, Ikawa M. Human Globozoospermia-Related Gene Spata16 Is Required for Sperm Formation Revealed by CRISPR/Cas9-Mediated Mouse Models. Int J Mol Sci. 2017;18(10).
Han F, Liu C, Zhang L, Chen M, Zhou Y, Qin Y, Wang Y, Chen M, Duo S, Cui X, Bao S, Gao F. Globozoospermia and lack of acrosome formation in GM130-deficient mice. Cell Death Dis. 2017;8(1):e2532.
Sha YW, Ding L, Wu JX, Lin SB, Wang X, Ji ZY, Li P. Headless spermatozoa in infertile men. Andrologia. 2017;49(8).
World Health Organization (WHO) (2010). WHO laboratory Manual for the examination of human semen and sperm-cervical mucus interaction. Cambridge Academic Press.
FAQs from users: 'What types of semen anatomical abnormalities exist?', 'Can abnormal sperm morphology fertilize an egg?', 'What happens if a sperm has two heads?', 'What is the meaning of globozoospermia?' and 'How does a pinhead sperm look like?'.




Dear sir,
My TZI =2.47
SDI =2.37
HEAD DEFECTS = 47.26%
Midpiece defects = 24.89%
Need help
Hello Mohamed Eisa,
Your TZI (teratozoospermia index) is close to 3, which means that yours is a case of severe teratozoospermia, and abnormalities are present in more than one part of the sperms you produce.
I am sorry!
Best wishes